Blunt Thoracic Trauma (BTT), Pain Management in
Published 2004
Citation: J Trauma. 59(5):1256-1267, November 2005.
An evidence-based outcome evaluation
2nd review—2003
I Statement of Problem and Questions to be Addressed
Studies of the consequences and treatment of blunt thoracic trauma (BTT) remain hampered by a varying pathologic definition of the disease. Entities typically classified as BTT include chest wall lesions such as rib fractures, flail chest and soft tissue contusion; intrapleural lesions such as hemothorax and pneumothorax; parenchymal lung injuries such as pulmonary contusion and lung laceration; and finally mediastinal lesions such as blunt cardiac injury.[1] [2] For purposes of this evidence-based review we are concerned primarily with those injuries to the chest wall that produce their morbidity through pain and it’s associated mechanical ventilatory impairment. Thus, blunt chest trauma (BTT) is defined here to include soft tissue trauma and injuries to the bony thorax such as rib fractures and flail chest.[3]
Within the scope of this definition, the incidence and morbidity of BTT clearly remains significant. Rib fractures themselves are believed to be very common and have been documented in up to two thirds of the cases of chest trauma.[4] [5] In another review 10% of all patients admitted to one trauma center had radiographic demonstration of rib fractures.[3] Isolated single or multiple rib fractures are one of the most common injuries in the elderly, at about 12% of all fractures, with an increasing incidence recorded as the population ages.[6] The true incidence of bony thoracic injury may be under-reported as up to 50% of fractures may be undetected radiographically[7] .
For patients with blunt chest wall trauma the morbidity and mortality are significant. These injuries are associated with pulmonary complications in more than one-third of cases[3] and pneumonia in as many as 30% of cases.[3] [8] [9] Patients over 65 may be even more prone to major complications after blunt chest wall injury[3] [10] [11] [12] with 38% respiratory morbidity from isolated rib fractures in another review.[13] Since blunt chest wall trauma causes death indirectly, through pulmonary and non-pulmonary complications, the true mortality rate for these injuries is hard to evaluate. In one study, 6% of patients with blunt chest trauma died and at least 54% of these deaths could be directly attributed to secondary pulmonary complications.[3] An elderly group of patients suffered an 8% mortality from isolated rib fractures.[13] Mortality of isolated flail chest has been as high as 16%.[14] The incremental costs attached to pulmonary complications of blunt chest trauma has not been addressed in the literature, but clearly would be measured in “ICU days” and “ventilator days”, both expensive commodities.
The treatment for injuries of the bony thorax has varied over the years, ranging from various forms of mechanical stabilization[15] [16] through obligatory ventilatory support.[17] [18] [19] It is now generally recognized that pain control, chest physiotherapy and mobilization are the preferred mode of management for BTT.[9] [20] Failure of this regimen and ensuing mechanical ventilation sets the stage for progressive respiratory morbidity and mortality.[3] [8] [20] Consequently, several different strategies of pain control have been employed, including intravenous narcotics, local rib blocks, pleural infusion catheters, paravertebral blocks and epidural analgesia. Each of these modalities has its own unique advantages and disadvantages and the overall most efficacious method has not previously been clearly identified. Subsequently, analgesic practices vary widely in this crucial setting. In one recent review, the majority of BTT patients were still managed with intravenous or oral narcotics.[21] Other authors noted that epidural catheters were offered in only 22% of elderly BTT patients and 15% of a younger cohort.[9]
This review seeks to identify the optimal method(s) of pain control for patients with blunt chest trauma. The specific questions which will be addressed utilizing an evidence-based approach for outcome evaluation are:
- Which patients with blunt chest trauma are at particular risk for respiratory morbidity due to a pain and deserve special attention to pain management?
- With consideration for safety, feasibility and therapeutic effectiveness, what is the optimal method of pain control in blunt chest trauma?
- For the recommended modality / modalities, what technical recommendations can be made for the administration of analgesia in blunt chest trauma.
- Anesthetic and technology concerns
- Nursing considerations
II Process
A computerized search was conducted of the Medline, Embase and Cochrane controlled trials databases for North American and European English language literature for the period from 1966 through July 1, 2003. The initial search terms were “chest injuries”, “thoracic injuries”, “rib fractures” and “flail chest”. These were cross-referenced for the secondary terms “analgesia”, “anesthesia” and “pain”. This search initially yielded 213 articles. 128 of these articles were excluded as being case studies, reviews, letters, or otherwise irrelevant to the questions being asked. This yielded a file of 85 articles for review. An additional 51 articles were obtained from the references of these studies yielding a total of 136 studies for review and grading. 91 of these were deemed appropriate for inclusion in the final evidentiary tables.
The practice parameter workgroup for analgesia in blunt thoracic trauma consisted of five trauma surgeons, one trained as a thoracic surgeon, two anesthesiologists and one trauma clinical nurse specialist. All studies were reviewed by two committee members and graded according to the standards recommended by the EAST Ad Hoc Committee for Guideline Development.[22] Grade I evidence was also sub-graded for quality of design utilizing the Jahad Validity Scale published in Controlled Clinical Trials in 1996.[23] Any studies with conflicting grading were reviewed by the committee chairperson and were all Grade I studies. Recommendations were formulated based on a committee consensus regarding the preponderance and quality of evidence.
III Recommendations
A. Efficacy of Analgesic Modalities
Level I
1. Use of epidural analgesia (EA) for pain control after severe blunt injury and non-traumatic surgical thoracic pain significantly improves subjective pain perception and critical pulmonary function tests compared to intravenous narcotics. EA is associated with less respiratory depression, somnolence and gastrointestinal symptoms than IV narcotics. EA is safe with permanent disability being extremely rare and negligible mortality attributable to treatment.
Level II
- Epidural analgesia may improve outcome as measured by ventilator days, ICU length of stay and hospital lengths of stay.
- There is some class I and adequate class II evidence to indicate that paravertebral or extrapleural infusions are effective in improving subjective pain perception and may improve pulmonary function.
Level III
- Though paravertebral or extrapleural analgesia is effective, there is an inadequate quantity of comparative evidence or information regarding safety to establish any recommendation with regard to overall efficacy.
- The information regarding both the effectiveness and safety of intrapleural and intercostal analgesia is contradictory and experience with trauma patients is minimal. Consequently no recommendation can be made regarding overall efficacy of this modality.
B. Clinical Application of Pain Management Modalities to Treatment of Blunt Thoracic Trauma
Level 1
- Epidural analgesia is the optimal modality of pain relief for blunt chest wall injury and is the preferred technique after severe blunt thoracic trauma.
Level II
- Patients with 4 or more rib fractures who are>65 years of age should be provided with epidural analgesia unless this treatment is contraindicated.
- Younger patients with 4 or more rib fractures or patients aged>65 with lesser injuries should also be considered for epidural analgesia.
Level III
- The approach for pain management in BCT requires individualization for each patient. Clinical performance measures (pain scale, pulmonary exam / function, ABG) should be measured as judged appropriate at regular intervals.
- Presence in elderly patients of cardiopulmonary disease or diabetes should provide additional impetus for epidural analgesia as these comorbidities may increase mortality once respiratory complications have occurred.
- Intravenous narcotics, by divided doses or demand modalities may be used as initial management for lower risk patients presenting with stable and adequate pulmonary performance as long as the desired clinical response is achieved.
- High-risk patients who are not candidates for epidural analgesia should be considered for paravertebral (extrapleural) analgesia commensurate with institutional experience.
- A specific recommendation cannot be made for intrapleural or intercostal analgesia based on the available evidence but its’ apparent safety and efficacy in the setting of thoracic trauma has been reported.
C. Technical Aspects of Epidural analgesic agents
Level I
There is insufficient Class I and Class II evidence to establish any specific techniques of epidural analgesia as a standard of care.
Level II
Combinations of a narcotic ( i.e. – fentanyl ) and a local anesthetic (i.e.bupivicaine) provide the most effective epidural analgesia and are the preferred drug combinations for use by this route. Use of such combinations allows decreased doses of each agent and may decrease the incidence of side effects attributable to each.
Level III
- While reliable literature describes the safe use of epidural analgesia on regular surgical floors, most victims of blunt thoracic trauma receiving this modality of treatment will have other primary indications for a higher level of care. Consequently, such patients in general, should be nursed in a monitored setting with cardiac monitoring and continuous pulse oximetry.
- There is insufficient evidence at this time to make a recommendation regarding the use of continuous epidural infusion vs. intermittent injection in trauma patients.
IV Scientific Foundation
a. Historical Perspective
The treatment of blunt thoracic trauma has undergone dramatic evolution over the twentieth century. In the first half of the century, the primary emphasis was on mechanical stabilization of the bony injury. This was first done by such external devices as sandbags or traction systems, and later by various surgical methods such as wires or screws.[24] After 1950, the concept of “internal pneumatic stabilization” with positive pressure mechanical ventilation was developed.[25] This became more prevalent and obligatory mechanical ventilation became the standard for chest wall trauma.[26]
The management of severe, blunt thoracic trauma evolved into the modern era with the publication of two studies in 1975. In a small series, Trinkle,[27] demonstrated that optimal pain control, chest physiotherapy and noninvasive positive pressure ventilation could avert the need for intubation and mechanical ventilation. Also in 1975, Dittman [28] published the first in a series of 3 articles on pain management in blunt chest trauma. In the first study, nineteen patients with multiple rib fractures and flail segments were treated with continuous epidural analgesia while intubation and mechanical ventilation were withheld. Using objective clinical criteria to monitor progress ( vital capacity, respiratory rate and tidal volume), seventeen patients were successfully managed without positive pressure ventilation. Dittman [29] subsequently showed that 46 of 49 (94%) of spontaneously breathing patients maintained a vital capacity greater than 13 ml/kg and avoided positive pressure ventilation through the use of morphine analgesia via a thoracic epidural catheter. Other European studies demonstrated good clinical results with epidural analgesia in blunt chest wall injuries when combined with pulmonary toilet and selective mechanical ventilation.[30-32]
Thus, the management of blunt thoracic trauma today focuses on both the underlying lung injury and on optimization of mechanics through chest physiotherapy and optimal analgesia.[30] [ 33-36] The critical importance of measuring ventilatory function tests as an objective means of monitoring adequacy of this analgesia was emphasized by the authors of the early studies.[33-36] Subsequent studies of pain management in blunt thoracic trauma patients would utilize the same methodology and additionally focus on comparisons between modalities and on objective outcome parameters.[ 37-40]
b. Modalities of Analgesia
Intravenous Narcotic
Intravenous narcotics have historically been the initial and most prevalent modality for relief of surgical and traumatic pain of all types. They are administered either by intermittent injection when pain is noted by the patient,[41] or continuous infusion.[42] Most recently intravenous patient-controlled analgesia (PCA) has been developed to exploit the benefits of both methods.[43] [44] In this modality a baseline intravenous infusion of morphine is provided and the patient may elicit an additional bolus for breakthrough pain.
The obvious advantages of intravenous narcotics are ease of administration and monitoring by nursing without the risks of an invasive procedure or need for specialized personnel. The efficacy of this modality for blunt chest wall trauma is controversial. Intravenous narcotics have been shown to improve pain scores and vital capacity, yet some clinicians consider them inadequate in this setting.[41] [43] The disadvantages of systemic narcotics are the tendency to cause sedation, cough suppression, respiratory depression and hypoxemia.[42]
Epidural Narcotics / Anesthetics
Epidural Analgesia (EDA) is a method whereby narcotics, anesthetic agents or combinations thereof are introduced into the spinal epidural space at the thoracic or lumbar level to provide regional analgesia. This is accomplished by introduction of a polyvinyl catheter into the epidural space and delivery of agents by either a bolus, continuous infusion, or more recently by a demand system.[32] [39] [45-50]
The major advantage of EDA is its apparent effectiveness in the absence of sedation.[32] [39] [45-50] Epidural has been shown to result in an increased functional residual capacity (FRC), lung compliance and vital capacity, a decreased airway resistance and increased pO2.[45] Tidal volume is increased and chest wall paradox in flail segments in reduced.[28] Patients with EDA generally remain awake and can cooperate with pulmonary toilet.[28] [47]
There are numerous real and theoretical disadvantages to EDA. Insertion may be technically demanding. Epidural anesthetics can cause hypotension, particularly in the face of hypovolemia, and occasional epidural infection.[46] [47] Epidural hematoma, accidental entry into the spinal canal and spinal cord trauma can also occur.[45]
Inadvertent “high block” may lead to respiratory insufficiency. By combining an epidural narcotic with the anesthetic agent, the dose of anesthetic can be decreased and these effects mitigated. However, the narcotic can cause nausea, vomiting, urinary retention, pruritis and occasionally respiratory depression.[28] [42] [51] The contraindications to epidural may prove problematic in the trauma patient. These include fever, coagulation abnormalities of even minor degrees and altered mental status. There is some anecdotal concern that the bilateral analgesia effect may mask the symptoms of intra-abdominal injury.[52] Finally, nursing intensity in monitoring for the effects of sympathetic block is somewhat more demanding than that for intravenous analgesia.[53]
Intercostal Nerve Block
Intercostal analgesia or “intercostal nerve block” traditionally involves individual injections of local anesthetic into the posterior component of the intercostal space.[45] [54-56] Because of segmental overlap of intercostal nerves, it is necessary to induce block above and below any given fractured rib. Blocks of adequate scope have been shown to relieve pain with multiple rib fractures and improve peak expiratory flow rate and volume.[57] However, the effect lasts only approximately six hours.
As a unilateral block, hypotension is rare and bladder and lower extremity sensation are preserved. The disadvantages of intercostal block include the need to palpate the fractured ribs for injection, and the need for multiple and repeated injections.[45] Local anesthetic toxicity may theoretically occur because of the higher doses needed and the incidence of pneumothorax increases with the number of ribs blocked.[58] Also, inducing block for upper rib fractures is technically difficult due to proximity of the scapula. Intercostal catheterization and continuous infusion has been successfully used and mitigates the need for multiple injections.[43] [54] However, the anatomic endpoint of catheter placement, piercing of the “posterior intercostal membrane” is often unclear raising the possibility of misplacement.[59-61] The full anatomic limits of the spread of intercostal drugs is unclear.[60-61]
Intrapleural Anesthesia
Intrapleural analgesia involves placement of a local anesthetic agent into the pleural space via an indwelling catheter.[62] The produces a unilateral intercostal nerve block across multiple dermatomes by gravity-dependent retrograde diffusion of agent across the parietal pleura.[45] As a unilateral modality it has advantages similar to intercostal block as regards hypotension and bladder and lower extremity sensation. Successful use of this modality has been reported in blunt thoracic trauma patients.[38] [63-65]
In terms of disadvantages, a significant amount of anesthetic may be lost if a tube thoracostomy is in place, which is often the case with trauma patients.[66] [67] This can be mitigated by temporary “clamping” of the thoracostomy which in turn evokes concerns of tension pneumothorax. Conversely, in the absence of a tube thoracostomy, intrapleural catheter placement may cause a pneumothorax. The presence of hemothorax, also common in thoracic trauma patients may theoretically impair diffusion of anesthetic.[68] Since distribution of agent is gravity-dependent, effectiveness also varies with patient position, catheter position and location of fractured ribs. Diffusion is most widespread when supine which is not optimal for pulmonary function in the trauma patient.[45] Conversely, the semi-upright position may allow disproportionate diffusion inferiorly and adversely affect diaphragmatic function.[69]
Thoracic Paravertebral Block
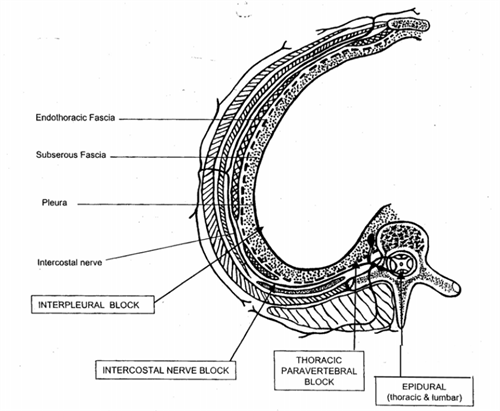
Figure 1. The anatomic location of delivery for the various modalities of regional thoracic analgesia From Karmakar MJ, Anthony MH, Acute Pain Management of Patients with Multiple Rib Fractures. J Trauma 2003; 54: 615-625
Thoracic Paravertebral block involves the administration of a local anesthetic agent in close proximity to the thoracic vertebrae. This can be achieved by intermittent injection, bolus via a catheter or continuous infusion and produces a unilateral somatic and sympathetic block which extended over multiple dermatomes.[31] [43] [66] [70-76]
Despite the fact that little recent investigation has been done with his modality, its theoretical advantages are numerous. It does not require painful palpation of ribs, is not in conflict with the scapula and is felt by some to be technically easier than epidural.[74] [77] Because there is no risk of spinal cord injury as with epidural, this modality can be instituted on sedated or anesthetized patients. It has few contraindications and requires no special nursing management.[73] [74] The most common complications are vascular puncture, pleural puncture and pneumothorax.[45] The unilateral nature of the block makes hypotension rare, preserves bladder sensation and allows monitoring of the lower extremity neurological exam when necessary.
The anatomic location of delivery for the various modalities of regional thoracic analgesia is illustrated in Figure 1.
c. Support for Risk Assessment in Blunt Thoracic Trauma
In 1993, Sariego,[78] showed that while trauma score and ISS predicted mortality in blunt thoracic trauma, neither identfied those survivors who would develop pulmonary complications. Clearly, factors leading to pulmonary sepsis and / or mechanical ventilation set the stage for severe morbidity or mortality. Studies addressing risk assessment in blunt thoracic trauma are tabulated in table 2.
Extent of injury to bony thorax
In a very large (n=692) retrospective class II series, Svennevig [79] identified the presence of four or more rib fractures as an independent predictor of dramatically increased mortality. Patients with 3 or less fractures suffered only a 2.5% mortality while those with four or more had a 19% mortality (p<.05). Similarly, in a large (n=105,000) state registry review (Class III) Lee [80] noted a 4% mortality rate for 2,477 patients with three or more rib fractures and a 1% rate for a similar group with two or less fractures. (p<.001) The “two or less” fracture group had a statistically similar mortality to the control group in which the patients had no rib fractures.
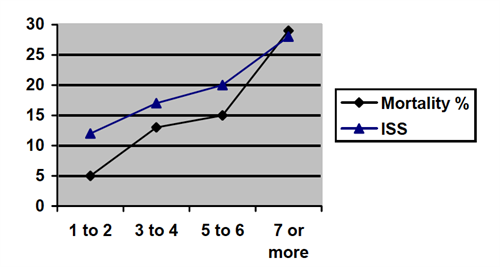
Figure 2. From Ziegler V et al, Mortality and Morbidity of Rib Fractures. J Trauma 37:975-979
Finally, Ziegler,[81] also in a large retrospective review (n=711), analyzed mortality in relation to incrementally increasing number of rib fractures. He found 5% mortality with 1-2 fractures, 13% mortality with 3-4 fractures and 29% mortality with 7 or more fractures. Analysis of these results did identify an inflection point for increased mortality at four fractures as noted in figure 2. It should be noted that only 6% of patients had isolated rib fractures and correction was not made for ISS, which tracked the number of fractures. Consequently, the contribution of the primary chest wall injury to mortality cannot not be isolated reliably.
Age
The salient class II study was performed by Bergeron and associates[82] in 2002. His group prospectively divided 405 patients with rib fractures in to a “65 or above age group” and a “less than 65 age group”. The elderly patients had a significantly higher comorbidity rate (61% vs. 8% p<.0001) Their analysis corrected for varying ISS, comorbidity and a slight difference in mean fracture number. They identified a five times greater risk of dying in the over 65 age group (9% vs. 19% morality p <.01). This finding is most compelling since the elderly group had a significantly lower ISS despite their higher mortality. (p<.031)
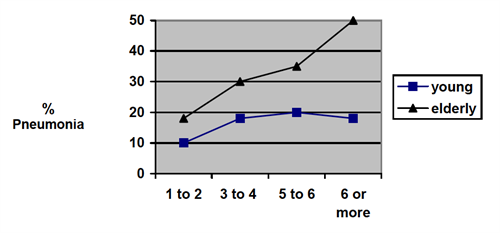
Figure 3. Number of Rib Fractures vs. incidence pneumonia for Elderly and Young Populations. From Bulger EM, Rib Fractures in the Elderly. JTrauma, 48: 1040-1047
Finally, an elegant attempt to relate the cumulative or synergistic effects of age and extent of chest wall injury was made by Bulger and colleagues[83] in their retrospective (class II) study of 458 blunt thoracic trauma patients. These authors also divided their population into a customary “65 or older group” and a “younger than 65” group which were well matched in terms of injury severity. Pneumonia and mortality occurred twice as frequently in the older group (31% vs. 17% and 22% vs. 10% respectively; both p<.01). Similarly, pneumonia and mortality tracked the number of rib fractures in both groups with a mortality odds ratio of 1.2 for each additional fractured rib at any age.(p<.001) Not surprisingly, the rate of pneumonia increased more rapidly with increasing rib fractures for the elderly group as noted in figure 3.
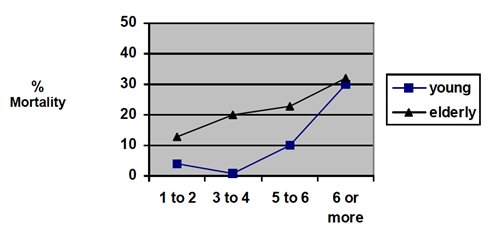
Figure 4. Number of Rib Fractures vs. % Mortality for Elderly and Young Populations. From Bulger EM, Rib Fractures in the Elderly. JTrauma, 48: 1040-1047
The critical finding in this study is that ventilator days, ICU days, hospital length of stay (LOS) and mortality increased more rapidly with increasing number of rib fractures for the elderly population. However, this difference was only statistically significant in the mid-range of rib fractures, three through six, giving rise to a characteristic curve for these parameters. (p<.05 or less) This distinctive pattern is illustrated in figure 4 by the “number of fractures vs mortality” plot.
The authors postulate that this characteristic curve results from the poor tolerance by the elderly for “moderate" levels of injury which are well tolerated by a younger cohort. At the upper extremes of chest wall injury, both groups do poorly and the curves again approach. All in all the cumulative effect of age and severity of chest wall injury was powerful. In this study, an elderly person with six rib fractures had a mortality risk of 24% and a pneumonia rate of 35% vs. 10% and 20% respectively for a younger patient. ((p<.05).
Co-morbidity
Barnea and colleagues[84] retrospectively reviewed 77 elderly (age>65) with isolated rib fractures. They identified a strong relationship between non-survival and the presence of diabetes or congestive heart failure. (p=.0095 and .001 ) Similarly, Alexander[85] retrospectively reviewed 62 elder patients with isolated rib. Complications occurred in 55% (n=17) of patients with cardiopulmonary disease ( “CPD+” for coronary artery disease or chronic obstructive lung disease) but in only 13% (n=4) of those without. (“CPD-“) (p<.05) Mortality occurred in only in the CPD+ group (10% n=3 p<.05) Upgrade in level of care was more common in the CPD + group. Length of ICU stay and hospital stay was double in the CPD+ group. (p<.03).
Conversely, Ziegler [81] in a retrospective review of 711 patients was unable to find a correlation between mortality and the co-morbidities of chronic obstructive lung disease (n=37), diabetes (n=55) or hypertension (n=155). There was also no increase in mortality noted for patients with coronary artery disease (n=116) as defined by a previous myocardial infarction or treatment for angina or for patients with a previous stroke (N=27) Specific statistical information is not provided in this study.
Concurrent extrathoracic injury
The cumulative effect of distant injury on the mortality of blunt thoracic trauma has rarely been specifically addressed. In Svennevig’s [79] retrospective, class II review of 652 blunt trauma patients previously discussed, the presence of one extrathoracic injury did not significantly increase mortality. However, the presence of two extrathoracic injuries increased mortality dramatically, and the highest death rate occurred in the thoracoabdominal injury sub-group. (see table 1)
| N | Mortality (%) | P< | |
|---|---|---|---|
| Solitary Thoracic injury | 226 | 5 (2.2) | |
| 1 Extrathoracic injury | 267 | 9 (3.4) | |
| >2 Extrathoracic injuries | 159 | 36 (22.6) | 0.05 |
| Thoracoabdominal subgroup | 96 | 24 (25.0) | 0.05 |
This would not seem surprising as the injury severity score has traditionally been accepted as an overall predictor of mortality. However a number of studies suggest that ISS may not be a valid predictor of risk of death in the elderly.[86] [87] [88] Consequently, the incremental effect of distant injury on the mortality of blunt thoracic trauma becomes difficult to assess.
| NS = not significant | ||||
| Author/year | Class | N | Significant Findings | P< |
|---|---|---|---|---|
| Extent of thoracic injury | ||||
| Svennevig 86 | II | 652 | > 4 or more rib fractures associated with 19% mortality vs. 2.5% for less than 4 fractures | .05 |
| Lee 90 | III | 105,000 | >3 rib fractures associated with 4% mortality vs 1% for <2 fractures | .001 |
| Ziegler 94 | III | 711 | Mortality with rib fractures 1-2 = 5%; 3-4 = 13%; >7 = 29% | .05 |
| Bulger 2000 | II | 464 | 1.2 odds ratio for mortality for each additional fracture > 2. | .001 |
| Age | ||||
| Bergeron 02 | II | 405 | ISS of elderly group lower yet 5x mortality over age 65. ( 9% vs. 19%). Multivariate egression to compensate for differing co-morbidity. | .01 |
| Svennevig 86 | II | 652 | Analyzed age in 10 year increments. Mortality >80 = 26%; >70 = 16%. Mortality < 70 = 6.8% or less. | .05 |
| Albaugh 2000 | III | 58 | Risk of mortality increased by factor of 2.3 for every 10 years of age >20 | .05 |
| Bulger 2000 | II | 464 | Pneumonia and mortality occurred 2x as frequently in >65. Ventilator, ICU and hospital days were also statistically greater. | .01 |
| Age and extent of injury | ||||
| Bulger 2000 | II | 464 |
Mortality, pneumonia, ventilator, ICU and hospital days increased more rapidly with increasing fractures in the elderly group. (age>65) |
.01 .05 |
| Co-morbidity | ||||
| Barnea 02 | III | 77 | Strong mortality risk in the elderly incurred by CHF or diabetes. | .001 |
| Alexander 2000 | III | 62 | Upgrade in care, ICU LOS, hospital LOS, complications, mortality significantly higher with co-morbidity or cardiopulmonary disease | .05 |
| Ziegler 94 | III | 711 | No correlation with mortality and COPD, Diabetes, HTN, CAD or CVA. | NS* |
| Distant injury | ||||
| Svennevig 86 | II | 652 | No increased mortality with one extrathoracic injury. Significantly increased mortality with 2 or more. Greatest incremental mortality with thoracoabdominal injury | .05 |
d. Support for Choice of Pain Management Modality
1. Effectiveness of Analgesic Modalities
Thoracic Epidural Analgesia
Studies relating to epidural analgesia are summarized in table 3. The greatest recent experience with invasive, regional pain management in the Western world, and in North America in particular rests with epidural modalities (EDA). Yet there is minimal compelling evidence that EDA improves outcome in trauma patients. Review yielded only one credible study to this end; Ullman et al,[39] in a landmark class I review in 1989 randomized 28 isolated blunt chest trauma (BCT) patient to receive continuous epidural narcotic or intermittent IV injection. The epidural group had significantly less ventilator days (3.1+ 1.4 vs 18.3+ 8.1, p<.05), shorter ICU length of stay ( 5.9+ 1.5 vs 18.7+5.3, p<.02), and shorter hospital length of stay (14.9+ 2.2 vs 47.7+14.6, p<.02). The EDA group also had a tracheostomy rate of 7% vs 38% for the control group. Though the sample size was small, the study was adequately powered to the detect the differences indicated.
In an early, class II study, Gibbons [30] in 1973, noted that 27 blunt chest trauma patients treated with lumbar EDA anesthetic required ventilatory support half as frequently as 30 patients who received intravenous narcotic or single dose intercostal blocks. However, randomization criteria are not specified and there was hesitancy to use thoracic EDA for upper rib fractures at that time. Similarly, in a retrospective study, Wisner [40] applied multiple logistic regression analysis to registry data of 465 elderly patients with blunt chest trauma. His group identified the use of EDA as an independent predictor of decreased mortality and pulmonary complications in elderly blunt trauma patients.
Similarly, though EDA is virtually routine in elective thoracic surgery, literature supporting improved outcomes are surprising scare for this popular application as well. The solitary class I study in this field was available only as recently as 2003. In this work, Della Rocca[89] showed a 9 day versus 11 day hospital stay for 280 thoracotomy patients who received EDA compared to a similar control group. However, the application of outcome measures from an elective thoracic surgery population to the multiple trauma patient is without validation and conceptually problematic.
Conversely, while quality proof of improved outcome is limited, the evidence that epidural modalities improve subjective pain scores and a variety of pulmonary functions in blunt thoracic trauma patients is abundant and compelling. (see tabulation table “Epidural Analgesia”) Four additional class I studies,[37] [38] [42] [44] five class two studies [29] [30] [46] [50] [90] and five class III studies [28] [32] [49] [91] [92] document significant improvements in commonly accepted analog pain scales and such pulmonary parameters as vital capacity, tidal volume, negative inspiratory force (NIF), maximum inspiratory flow rate (MIF) and minute ventilation (Ve). Among salient class I studies, Moon[44] performed a randomized comparison of narcotic / anesthetic epidural with PCA in two well-matched groups (n=24) of blunt chest trauma patients. The EDA group had a continual increase in maximal inspiratory force (24% from baseline) over the first 3 days while the PCA group had an 18% decrease in the same period. Similarly, initial tidal volume (Vt) for the two groups was not significantly different. However, Vt for the PCA group fell 56% by day three while that for the EDA group rose by 48%. At the end of this study period, mean Vt was 590 ml for the EDA group vs. 327 ml for the PCA group.(p<.05). Subjective pain scores were similarly dramatically improved ( 3.8 for EDA vs 6.2 for PCA p<.05).
Similarly, Mackersie et al[42] randomized 32 multiple rib fracture patients to receive fentanyl by either continuous epidural route or continuous intravenous infusion. Mean vital capacity (VC) was dramatically improved in the EDA group vs the IV group ( 5.1 ml/kg vs 2.8 ml/kg; p<.002) as was maximum inspiratory pressure ( 17 cm H20 vs 5.3 cm H20; p <..05). In this study there was no significant change produced in tidal volume, respiratory rate or minute volume assessed to either method. Though there was a trend toward better improvement in subjective pain scores with EDA, this did not reach statistical significance for the small study group. Similarly, in an early, but sizeable class II observational study, Worthley[47] treated 147 non-ventilated patients with bolus EDA using local anesthetic. A doubling of vital capacity was noted after each dose of the epidural. 9% of patients required mechanical ventilation.
The literature derived from elective thoracic surgery is similarly supportive of the benefits of epidural modalities. Four credible class I studies totaling over 600 patients document very significant improvements in subjective pain control and pulmonary function.[89] [93-95] One well-designed, class I study failed to identify any subjective pain score benefits to lumbar epidural fentanyl vs. continuous fentanyl infusion.[96] However, the study population was small (n=30), combination epidural anesthetic was not used and dosing was subjectively titrated for equivalent pain control. Conversely, in a very large prospective review of 2670 EDA patients and 1026 IVA controls, Flisberg [97] noticed dramatic improvement in subjective pan scale.
Other Analgesic Modalities
Little evidence exists for the efficacy of other modalities of invasive, regional analgesia. Ideally these methods should first be compared to control cases receiving intravenous medication to establish baseline effectiveness. They should then be compared to epidural modalities, with which the most experience exists so as to identify the most effective technique. Studies relating to other modalities of analgesia are summarized in tables 4 through 6.
Paravertebral block as described in greater detail above, is a method in which a bolus injection of anesthetic or a continuous infusion is delivered to the thoracic paravertebral space at the level of rib fractures producing a unilateral, multilevel somatic and sympathetic block.[72] [74] This method is essentially a modality of extrapleural analgesia as the drug is delivered posterior to the parietal pleura but anterior to the costotransverse ligament near the spine. While there are a number of anecdotal reports, [70] [71] [98-100] the evidence supporting this modality in trauma patients or general thoracic patients is scant. In a small prospective study, (class II) Gilbert[70] administered a single paravertebral anesthetic dose to a mixed group of patients suffering blunt or penetrating thoracic trauma. VC increased by 65%, and respiratory rate decreased by 35%, both to highly significant degrees. Pain scale improved significantly while measures of flow rates (MMEFR and FEV1/FVC) were unchanged. In a similar class II, prospective study, Karmakar[76] administered continuous paravertebral anesthetic to fifteen patients with isolated unilateral rib fractures. There was highly significant (all p<.01 to .0001) sustained improvements in analog pain scores, vital capacity, and peak expiratory flow rate (PEFR). Interestingly, oxygen saturation (SaO2) and O2 index (paO2/FiO2 ratio) also improved significantly. (P<.05)
Extrapleural analgesia is a technique closely related to the paravertebral modality whereby a catheter is positioned in an extrapleural location and a continuous infusion of local anesthetic is delivered. In a prospective class I study, Haenal [43] administered continuous extrapleural anesthetic to fifteen patients with three or more unilateral rib fractures without other injuries. Visual analog pain scale halved and incentive spirometry doubled. This was significant despite the small study size.(p<.05) The authors of this study further noted that an anesthesiologist was not utilized to initiate this therapy at their institution. Similar results have been reported in two class II [102] [104] and one class I [103] study in the thoracic surgery literature.
Intrapleural catheters are placed percutaneously in patients with or without chest tubes and used to infuse local anesthetics. They have also been placed through the tracts of in situ tube thoracostomies. Among the salient class I studies, Gabram [104] randomized 42 blunt chest trauma patients to receive systemic narcotics (IVA) or intrapleural anesthetics (IPA) Half the IVA group required crossover to another modality or received mechanical ventilation while this occurred in only 10% of the IPA group. (p<.05) Changes in pulmonary functions did not reach statistical significance. In a randomized, blinded study Kottenbelt [64] administered intrapleural anesthetic or intrapleural saline to 120 blunt and penetrating trauma patients. 62% of the test group but only 15% of the placebo group received satisfactory analgesia by a visual analog scale. (p<.00001) Additionally, responders in the treated group had maintenance of their pain relief for a significantly longer period. (3.9 hrs vs. .9 hours; p<.005) Pulmonary functions were not assessed. Conversely, in a class I blinded study of IPA anesthetic vs. IPA placebo in 16 blunt trauma patients, Short [68] identified no difference in pulmonary function tests, arterial blood gases, subjective pain score or breakthrough narcotic use. It is noted that the study size was limited. In similar study, Schneider [105] found no benefit to IPA in terms of pain scale, length of stay or sparing of intravenous narcotics.
Intercostal block (ICB) was initially performed both by multiple single injections but more recently through a percutaneously placed catheter.[31] Murphy [54] retrospectively reviewed 57 trauma and general surgery patients treated with multiple intercostal catheter injections of bupivicaine. In this anecdotal, class III study, patients allowed chest wall palpation and appeared to tolerate physiotherapy better after catheter injection. Analgesia duration was 8 to 12 hours with one dose. All further reviews of ICB were embedded in comparative studies and will be considered as such below.
Comparative Studies
Few comparative studies of the treatment of thoracic pain are to be found in the trauma or general thoracic literature. Shinohara [38] performed a small, randomized cross-over study examining intrapleural (IPA) and epidural (EDA) in 17 patients with multiple unilateral rib fractures. Subjective pain scores were similar, but since IPA induced a unilateral sympathetic block, blood pressure did not fall with IPA while it did with EDA. This difference was not significant however. Luchette and associates [37] similarly performed a prospective randomized comparison of continuous EDA anesthetic vs intermittent IPA anesthetic in nineteen blunt thoracic trauma patients. Their epidural patients had significantly less pain at rest and with motion and this difference continued to widen and was dramatic by day three. Breakthrough IV narcotic use was proportionately different also. Most importantly in this study, tidal volume and negative inspiratory pressure differences were highly significant by day 3 in favor of the epidural route. ( All p<.05) Vital capacity and minute volume were unaffected. .These authors concluded that continuous epidural was superior to the intrapleural route in terms of pain control and pulmonary function improvement. Though performed in thoracic surgery patients (N=40), Bachmann-Mennenga [56] carried out an elegant randomized four-limb study comparing intercostal block, intrapleural analgesia, thoracic epidural block and intravenous narcotic. In their study intercostal and epidural produced the greatest pain relief to a high degree of significance (p<.01) and had commensurate low levels of narcotic use. Intrapleural block had no narcotic-sparing effect over baseline IV analgesia even though catheter placement was confirmed at surgery. It was postulated that the thoracostomy tubes were draining off the anesthetic agent. Though most effective, the epidural route gave the least systemic anesthetic levels. The authors concluded that epidural an intercostal anesthetics constituted the most effective modalities for control of thoracic pain. Other studies in thoracic surgery patients show preference for intrapleural over intercostal analgesia and paravertebral over intrapleural routes.[37] [38] [55] [56] [66] However all comparative studies are few and their total patient numbers small. Comparative studies are summarized in table 7.
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
|
Bold = Class 1 studies, Grey Background = Class III EDA = epidural analgesia, IPA = intrapleural analgesia, PVA = paravertebral or extrapleural analgesia, IVA = Intravenous analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases, TV = tidal volume, MIF = maximum inspiratory force, VC = vital capacity |
|||||
| Ullman 89 | EDA vs IVA | Blunt Trauma | I | 28 | Decreased tracheostomy, vent days, ICU and hospital LOS with EDA |
| Cicala 90 | Thoracic EDA anesthetic vs Lumbar EDA narcotic | Blunt Trauma | I | 14 | Both were equally effective on pain scores. Thoracic anesthetic modestly superior in improving PFTs. |
| Mackersie 91 | EDA vs. IVA non-random | Blunt Trauma | I | 32 | EDA narcotic improved MIF and ABG >> IVA. EDA improved VC > IVA. Subjective pain scale trended towards sig. for EDA |
| Luchette 94 | EDA vs. IPA | Blunt Trauma | I | 19 | EDA > IPA in improvement in PFTs and decreased narcotic use. |
| Shinohara 94 | EDA vs. IPA | Blunt Trauma | I | 17 | Subjective pain control same. Slightly less Cx with IPA |
| Moon 99 | EDA vs IVA | Blunt Trauma | I | 24 | EDA superior pulmonary function, pain relief and decreased proinflammatory cytokines. |
| Gibbons 73 | EDA vs (ICB or IVA) Non-randomized | Blunt Trauma | II | 60 | EDA required vent ••• as frequently. |
| Dittman 78 | EDA vs. obligatory vent Non-randomized | Blunt Trauma | II | 283 | Pulmonary mechanics improved with EDA. 5 patients on EDA limb needed 2o vent but groups not randomized. |
| Rankin 84 | EDA single limb – descriptive | Blunt Trauma | II | 50 | Subjective pain scores decreased. |
| Worthley 85 | EDA single limb – observational | Blunt Trauma | II | 147 | V.C. doubled. Early study showing avoidance of obligatory mechanical ventilation. |
| KOH 91 | EDA single limb – observational | Mixed Trauma | II | 19 | TV, VC, NIF and subjective pain score better with EDA > IVA |
| Govindrajan 02 | EDA single limb – observational | Blunt Trauma | II | 27 | PFTs and subjective pain rating improved |
| Dittman 75 | EDA single limb retrospective | Blunt Trauma | III | 6 | Significant improvement in VC |
| Abouhatem 84 | EDA single limb retrospective | Blunt Trauma | III | 19 | “Good” subjective pain control |
| Mackersie 87 | EDA single limb retrospective | Blunt Trauma | III | 40 | Significant increase in VC, MIF, Smaller increase TV, Ve. Good subjective pain relief |
| Wisner 90 | EDA single limb retrospective | Blunt Trauma | III | 50 | EDA was predictor of decreased pulmonary complications and mortality |
| Doss 99 | EDA anesthetic single limb retrospective | Blunt Trauma | III | 57 | “Good” subjective pain control |
| WU 99 | EDA vs IVA (PCA) retrospective | Blunt trauma | III | 57 | Significantly lower pain scores with EDA bupivicaine and fentanyl |
| Shulman 84 | EDS narcotic vs IV Narcotic | Thoracic Surgery | I | 30 | EDA provided less pain, lower RR, better PFTs. Subjective pain score unchanged. |
| Logas 87 | EDA narcotic vs EDA anesthetic vs both vs placebo | Thoracic Surgery | I | 53 | Re: pain control and narcotic needs. EDA narcotic 2x EDA anesthetic. Combination even more effective. |
| Saliomaki 91 | EDA narcotic vs IVA | Thoracic Surgery | I | 20 | EDA > IVA for pain relief and respiratory function (RR and ABG) |
| Sandler 92 | EDA narcotic vs IVA | Thoracic Surgery | I | 29 | Modalities same in terms of pain control and respiratory depression. Plasma Fentanyl conc. Same. |
| Bachmann 93 | IPA vs ICB vs EDA vs IVA | Thoracic Surgery | I | 40 | EDA = ICB>>IPA for pain scale and decreased narcotic use. |
| Hansdottir 96 | Lumbar EDA narcotic vs thoracic EDA narcotic vs thoracic combination | Thoracic Surgery | I | 37 | Combination gave superior analgesia at rest and with activity. Less rescue narcotics. Complication rates the same. |
| Wiebalck 97 | EDA anesthetic vs. EDA combination | Thoracic Surgery | I | 100 | Lower pain scores and lower doses of anesthetic used with combination. |
| Kaiser 98 | EDA vs EPA | Thoracic Surgery | I | 30 | Equivalent pain scores and return of pulmonary function. Slightly less IV narcotic use with EPA. |
| Della Rocca 03 | EDA narcotic vs. IVA | Thoracic Surgery | I | 563 | EDA significantly better pain control and decreased LOS !! IV group had more complications, nausea, vomiting. |
| Melendez 89 | Narcotic Lumbar EDA single limb – observational | Thoracic Surgery | II | 17 | Decreased pain scale. No increased respiratory depression |
| Scherer 93 | TEA – single limb observational | Mixed | II | 11K | Minimal complication rates in huge series. No permanent disability or death. |
| Giebler 97 | TEA – single limb observational | Mixed | II | 2059 | Overall complications 3%. Permanent neuro disablity .07% |
| Flisberg 03 | EDA vs IVA Prospective non-random | Thoracic Surgery | II | 2670 | Better subjective pain control and less narcotic sde effects with EDA |
| Fromme 85 | Lumbar vs Thoracic Narcotic EDA | Thoracic Surgery | III | 122 | Both equally effective. |
| Ready 91 | EDA Narcotic – single limb observational | Mixed | III | 1106 | Minimal complications in huge review. No permanent disability or death. |
| Kurek 97 | Continuous combination EDA to bolus narcotic EDA | Mixed | III | 98 | Contnuous infusion had higher complication rate. But also utilized a local anesthetic. |
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| IVA = Intravenous analgesia, EDA = epidural analgesia, IPA = intrapleural analgesia, EPA = extrapleural analgesia, PVA = paravertebral analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases | |||||
| O’Kelly 81 | EPA single limb – descriptive | Blunt trauma | N/A | 4 | Patients reported decreased pain |
| Haenel 95 | EPA single limb – observational | Blunt trauma | II | 15 | Spirometry doubled and decreased analog pain scale. |
| Gilbert 89 | PVA single limb – observational | Blunt trauma | II | 10 | Pain control and RR improved. No sig. Change in PFTs. |
| Karmakar 03 | PVA single limb – observational | Blunt trauma | II | 15 | Improved pain score, PFTS, ABG. No sig. complications |
| Lonnqvist 95 | PVA sinle limb – observational | Mixed | II | 367 | 10% failure rate. Authors claim similar complication rat to EDA. |
| Richardson 95 | PVA vs IPA | Thoracic surgery | I | 45 | PVA had improved PFTS, respiratory morbidity and LOS. Less complications. Breakthrough narcotics same. |
| Kaiser 98 | EPA vs EDA | Thoracic surgery | I | 30 | Good pain scores and return of pulmonary function.with EPA. Slightly less IV narcotic use than EDA. |
| Author/year | Nature of Study | Population | Class | N | Statistically Significant Findings |
|---|---|---|---|---|---|
| EDA = epidural analgesia, IPA = intrapleural analgesia, PVA = paravertebral or extrapleural analgesia, IVA = Intravenous analgesia ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases | |||||
| Luchette 94 | IPA vs EDA | Blunt trauma | I | 1 9 | EA Reduced narcotic use and improved PFTS > IV |
| Shinohara 94 | IPA vs EDA | Blunt Trauma | I | 1 7 | Subjective pain control same. Slightly less Cx with IPA |
| Grabram 95 | IPA vs IVA | Blunt Trauma | I | 4 2 | IPA improved PFTS > IVA and required vent ••• as often |
| Short 96 | IPA anesthetic vs IPA placebo | Blunt trauma | I | 1 6 | No difference in narcotic use, PFTS, ABG, subjective pain |
| Kottenbelt 91 | IPA anesthetic vs IPA placebo | Blunt and penetrating Tr | I | I | IPA dramatically improved subjective pain score. |
| Symreng 88 | IPA anesthetic vs IPA placebo | Thoracic Surgery | I | 1 5 | IPA improved pain scores, PFTS, decreased narcotic use |
| Shafei 90 | IPA vs ICB | Thoracic Surgery | I | 5 4 | IPA decreased narcotic use > ICB. Complications same. |
| Bachmann 93 | IPA vs ICB vs EDA vs IVA | Thoracic Surgery | I | 4 0 | IPA had no narcotic spariing effect over IVA in setting of tube thoracostomies. |
| Schneider 93 | IPA vs placebo | Thoracic Surgery | I | 1 9 | No difference between IPA and plebo as measured by pain scale, IV narcotic sparing or length of hospitalization. |
| Richardson 95 | IPA vs PVA | Thoracic Survery | I | 4 5 | IPA inferior to PVA in terms of narcotic use, PFTS, LOS and respiratory morbidity. IPA had sig. bupivicaine toxicity effects |
| Gomez 87 | IPA observational | Thoracic Surgery | II | 1 8 | Described very significant failure and complication rate in small study. |
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| EDA = epidural analgesia, IPA = intrapleural analgesia, PVA = paravertebral or extrapleural analgesia, IVA = Intravenous analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases | |||||
| Shafei 90 | ICB vs IPA | Thoracic Surgery | I | 54 | Greater narcotic use with the ICB group. Narcotic requirements were higher. |
| Bachmann 93 | ICB vs IPA vs EDA vs IVA | Thoracic Surgery | I | 40 | ICB and EDA provided greatest pain score improvement and narcotic sparing. |
| Murphy 83 | ICB descriptive | Blunt Trauma | III | 57 | Anecdotally, patients allowed rib palpation and tolerataed physiotherapy better after catheter injection. Analgesia duration 8-12 hours. |
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| EDA = epidural analgesia, IPA = intrapleural analgesia, PVA = paravertebral or extrapleural analgesia, IVA = Intravenous analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases | |||||
| Luchette 94 | EDA vs. IPA | Blunt Trauma | I | 19 | EDA > IPA in improvement in PFTs and decreased narcotic use. |
| Shinohara 94 | EDA vs. IPA | Blunt Trauma | I | Subjective pain control same. Slightly less Cx with IPA | |
| Della Rocca 03 | EDA narcotic vs. IVA | Thoracic Surgery | I | 56 3 | EDA significantly better pain control and decreased LOS !! IV group had more complications, nausea, vomiting. |
| Flisberg 03 | EDA vs IVA Prospective non-random | Thoracic Surgery | II | 26 70 | Better subjective pain control and less narcotic sde effects with EDA |
| Shafei 90 | ICB vs IPA | Thoracic Surgery | I | 54 | Greater narcotic use with the ICB group. Narcotic requirements were higher. |
| Bachmann 93 | ICB vs IPA vs EDA vs IVA | Thoracic Surgery | I | 40 | ICB and EDA provided greatest pain score improvement and narcotic sparing. |
| Richardson 95 | IPA vs PVA | Thoracic Surgery | I | 45 | IPA inferior to PVA in terms of narcotic use, PFTS, LOS and respiratory morbidity. IPA had sig. bupivicaine toxicity effects |
| Kaiser 98 | EDA vs EPA | Thoracic Surgery | I | 30 | Equivalent pain scores and return of pulmonary function. Slightly less IV narcotic use with EPA. |
2. Complications and Safety of Analgesic Modalities
Epidural
A number of sizeable studies have addressed the safety of epidural analgesia in various populations. Scherer[106] performed a prospective observational ( class II) study of 1071 patients in which he reviewed the complication rates but did not address the incidence of expected minor side effects. Patients received epidural narcotic or combination narcotic / analgesic. His group’s findings are indicated in table 8.
| Complications | N | % |
|---|---|---|
| Unsuccessful catheterization | 17 | 1.7 |
| Primary Dural perforation | 13 | 1.2 |
| Peripheral Nerve Damage | 9 | .8 |
| Postoperative radicular pain | 4 | .4 |
| Radicular pain during puncture | 2 | .2 |
| Respiratory Depression | 1 | .1 |
Overall treatment related complications were seen in 37 patients (3.5%). The peripheral nerve damage seen in .8% of patients was limited to tingling in various extremities, all of which resolved spontaneously. It is not clear if some of these may have been related to patient positioning during surgery. There were no sensory or motor deficits, meningitis or permanent neurologic sequelae. Though 116 patients (10.8%) showed at least one abnormal clotting parameter, there were no clinical hemorrhagic events related to the procedure. One patient experienced respiratory depression temporally related to injection which required intubation. He recovered without sequelae. The authors concluded that EDA was a safe modality with minimal risk of technique –related or pharmacological complications.
Similarly, Ready[107] and colleagues retrospectively reviewed 1100 postoperative epidural catheters managed outside of an intensive care setting. Narcotics only were used and therefore anesthetic complications such as hypotension were not assessable. These authors noted significant rates of pruritis (25%) and nausea (29%), though neither of these complications were disabling and were generally managed successfully. The only significant catheter-related problem was dislodgment which occurred at the rate of 3%. The salient complications noted in this study are summarized in table 9.
| Complication | % | 99% CI % |
|---|---|---|
| Pruritis | 25 | 23 |
| Nausea, vomiting | 29 | 25 |
| Respiratory depression | .2 | .07 |
| Neurologic injury | 0 | .4 |
| Death | 0 | .4 |
| Premature dislodgment | 3 | 5 |
It should be noted for completeness that as of April 1998, the Food and Drug Administration had recorded fifty spontaneous anecdotal safety reports describing the development of epidural hematomas with the concurrent use of low molecular weight heparins (i.e. – enoxaparin sodium) and epidural analgesia. The use of these medications for deep venous thrombosis prophylaxis may be a relative contraindication to epidural modalities.[108] [109]
Several studies have attempted to address comparative EDA complication rates against a control of intravenous narcotic.[39] [42] [89] [92] [93] [95-97] These studies are summarized in table 10 In general, the smaller studies are often conflicting and fail to identify the same differences in types or rates of complications.[39] [42] [92-94] When considering several larger class I and II comparative reviews, it is evident that each modality has a unique complication profile but that in both cases, the rates of significant morbidity are low. Intravenous analgesia tends to have significantly more respiratory depression, central sedative effects and gastrointestinal effects. Conversely epidural modalities tend to have more peripheral neurologic effects, pruritis, and when anesthetic agents are used, mild hypotensive effects. Luchette et al reported significant hypotenson with test boluses of Lidocaine.[37] However, all in all both modalities have similar, excellent safety profiles.
Other Modalities
The single large class II review of paravertebral analgesia, achieved with local anesthetic agents prospectively identified a 10% failure rate in 367 cases.[75] (see table 11) Hypotension requiring treatment occurred in 4.6%. Vascular puncture without morbidity occurred in 3.8% Pleural puncture without pneumothorax occurred in 1.1% and an additional .5% of patients (n=18) developed a pneumothorax. Some degree of contralateral anesthesia occurred in 1%. There were no instances of entrance into the spinal canal. It should be noted that these cases were accrued from three institutions and therefore represent only modest experience at each center. The time course of the study is not specified and the yearly experience at each institution may be small, thereby accounting for the increased complication and failure rate. Though the authors felt the complication rate was similar to that for epidural, other studies have identified lower epidural complication rates at approximately 3%.[39] [42] [89] [95] Regardless, no serious complications attributable to PVA were noted in this study. Other studies on paravertebral analgesia are tabulated in the table. A solitary case of transient Horner’s Syndrome was reported.[76] The single small class II study of the closely-related extrapleural analgesia noted no drug or catheter-related complications.[43]
The majority of small class I studies addressing the safety of intrapleural catheters identify no significant drug or catheter related complications for a total of 151 patients.[38] [55] [64] [68] [104] However one prospective observational study of 18 patients noted 11 incorrectly positioned catheters.[110] Seven were in lung tissue and three in the chest wall. One tension pneumothorax resulted. The authors postulated that these poor results were experience-dependent. In a small randomized comparative study, Richardson [66] noted significant bupivicaine toxicity with intrapleural catheters that did not occur with the paravertebral route. Studies addressing the safety of intrapleural analgesia are summarized in table 12.
The solitary retrospective, class III study addressing complication of intermittent intercostal block via an indwelling catheter, identified no catheter or drug-related complications in 57 patients.[54] (see table 13)
e. Technical Recommendations regarding conduct of Epidural Analgesia
Studies regarding technical recommendations for the conduct of epidural analgesia are summarized in table 14.
1. Pharmacology
In 1990, Cicala and colleagues[111] compared the effectiveness of a thoracic epidural local anesthetic to a lumbar epidural narcotic in blunt trauma patients. This group found that both modalities were equally effective in decreasing pain scores and the anesthetic agent was modestly superior in improving pulmonary function tests. The sample size was small (n=14) though the study was randomized and blinded. The authors theorized that the anesthetic agent benefits pulmonary function by blocking inhibitory neural impulses destined for the diaphragm thereby improving diaphragmatic function.
The bulk of the information regarding the pharmacology of epidural analgesia arises from elective thoracic surgical literature. In a randomized blinded study of 53 thoracic surgery patients, Logas showed that epidural narcotic was significantly more effective than anesthetic in subjective pain relief.[94] The combination was even more effective. Similarly, other randomized, blinded studies have showed lower pain scores and greater IV narcotic sparing with combination therapy as compared to epidural narcotic or anesthetic alone.[112] [113] Also, it is possible to use lower doses of both agents when used in combination.[112]
2. Mode of Infusion
The only study comparing continuous to bolus epidural in trauma patients (blunt and penetrating) was conducted by Kurek and colleagues[114] in 1997. In this retrospective study, the continuous infusion method had a slightly, though significantly higher complication rate (p<.05) than the bolus route. The most common complications with the continuous method were motor blockade (18%), nausea/vomiting (18%) and catheter leaks (12%). For bolus infusions nausea/vomiting ( (25%), mental status changes (21%) and local erythema (13%) were most common. There were no serious or permanent complications in either group.
3. Nursing Environment
Ready and colleagues[53] conducted a large retrospective review (n=1106) of a mixed patient population with epidural catheters managed at a general surgical floor level of care. Catheter related complications occurred in less than 5% of patients. None were serious complications and there were no deaths.
IVA = Intravenous analgesia, EDA = epidural analgesia, IPA = intrapleural analgesia, EPA = extrapleural analgesia, PVA = paravertebral analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| Ullman 89 | EDA Narcotic vs IVA | Blunt Trauma | I | 28 | No procedure related complications. No respiratory depression or pruritis. 2 cases urinary retention |
| Mackersie 91 | EDA vs. IVA non-random | Blunt Trauma | II | 32 | IV group has significant decrease in pO2 ( p<.03) and rise in pCO2 (p<.013) N,V, pruritis same but sample size small. No catheter related complications |
| WU 99 | EDA vs IVA (PCA) retrospective | Blunt trauma | III | 57 | No differences with respect to pulmonary, neurologic or cardiac complications. |
| Shulman 84 | EDS narcotic vs IV Narcotic | Thoracic Surgery | I | 30 | No sig differences in VS, somnolence score, nausea, vomiting. PCO2 significantly elevated in both groups. Four cases of pruritis with epidural / none with IV. Small sample size. |
| Saliomaki 91 | EDA narcotic vs IVA | Thoracic Surgery | I | 20 | Slow repiratory rate and apnea greater in IV group but not to signficance. Somnolence (p<.02) and nausea (p<.001) less with EDA Urinary retention equivalent. |
| Sandler 92 | EDA narcotic vs IVA | Thoracic Surgery | I | 29 | Modalities same in terms mild respiratory depression and incidence of side effects (Nausea, vomiting). |
| Della Rocca 03 | EDA narcotic vs. IVA | Thoracic Surgery | I | 563 | IV group had more complications, nausea, vomiting. |
| Flisberg 03 | EDA vs IVA prospective non-random | Thoracic Surgery | II | 2670 | Respiratory depression, sedation, hallucination more with IV narcotic group. Orthostasis, leg weakness, pruritis more with EDA group. |
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| IVA = Intravenous analgesia, EDA = epidural analgesia, IPA = intrapleural analgesia, EPA = extrapleural analgesia, PVA = paravertebral analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases | |||||
| Haenel 95 | EPA single limb – observational | Blunt trauma | II | 15 | No catheter or drug-related complications |
| Gilbert 89 | PVA single limb – observational | Blunt trauma | II | 10 | One mild hypotensive event. |
| Karmakar 03 | PVA single limb – observational | Blunt trauma | II | 15 | No sig. Complications. One case transient ipsilateral Horner Syndrome. |
| Lonnqvist 95 | PVA single limb – observational | Mixed | II | 367 | 10% failure rate. Similar complication rate to EDA. Hypotension 4.6% Vascular puncture 3.8% Pleural puncture 1.1% Pneumothorax .5% |
| Author/year | Nature of Study | Population | Class | N | Statistically Significant Findings |
|---|---|---|---|---|---|
| IVA = Intravenous analgesia, EDA = epidural analgesia, IPA = intrapleural analgesia, EPA = extrapleural analgesia, PVA = paravertebral analgesia, ICB = intercostal block, PFTS = pulmonary function tests, ABG = arterial blood gases | |||||
| Shinohara 94 | IPA vs EDA | Blunt Trauma | I | 17 | No toxic consequences of IPA. No catheter-related complications. |
| Gabram 95 | IPA vs IVA | Blunt Trauma | I | 42 | 21 IPA patients: No serious complications: |
| Short 96 | IPA anesthetic vs IPA placebo | Blunt trauma | I | 16 | No catheter of drug related toxicity. |
| Kottenbelt 91 | IPA anesthetic vs IPA placebo | Blunt and penetrating Tr | I | 120 | No catheter related complications. Of the 60 patients in treated group, no toxicity. |
| Shafei 90 | IPA vs ICB | Thoracic Surgery | I | 16 | 16 pts. In IPA limb; No drug or.catheter-related complications |
| Richardson 95 | IPA vs PVA | Thoracic Survery | I | 23 | 5/23 IPA had sig. bupivicaine toxicity resulting in confusion (p<.02) |
| Gomez 87 | IPA observational | Thoracic Surgery | II | 18 | 11/18 catheters incorrectly positions: 3 in chest wall; 7 in lung tissue; 1 tension pneumothorax. Authors postulated this was operator-dependent and experiential. |
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| Murphy 83 | ICB descriptive | Blunt Trauma | III | 57 | No catheter or drug complications |
| Author/year | Nature of Study | Population | Class | N | Findings |
|---|---|---|---|---|---|
| Cicala 90 | Thoracic EDA anesthetic vs Lumbar EDA narcotic | Blunt Trauma | I | 14 | Both were equally effective on pain scores. Thoracic anesthetic modestly superior in improving PFTs. |
| Logas 87 | EDA narcotic vs EDA anesthetic vs both vs placebo | Thoracic Surgery | I | 53 | Re: pain control and narcotic needs. EDA narcotic 2x EDA anesthetic. Combination even more effective. |
| Hansdottir 96 | Lumbar EDA narcotic vs thoracic EDA narcotic vs thoracic combination | Thoracic Surgery | I | 37 | Combination gave superior analgesia at rest and with activity. Less rescue narcotics. Complication rates the same. |
| Wiebalck 97 | EDA anesthetic vs EDA combination | Thoracic Surgery | I | 100 | Lower pain scores and lower doses of anesthetic used with combination. |
| Niemi 98 | Addition of Epinephrine to narcotic / anesthetic epidurals | Mixed | I | 24 | Better sensory block, similar side-effects, lower serum narcotic levels |
| Dernedde 03 | High concentration vs. low concentration anesthetic for continuous epidural | Mixed | I | 27 | For same total dose, high concentration / low volume provided equivalent pain score with less motor block and less hemodynamic consequences. |
| Fromme 85 | Lumbar vs Thoracic Narcotic EDA | Thoracic Surgery | III | 122 | Both equally effective. |
| Kurek 97 | Continuous combination EDA to bolus narcotic EDA | Mixed | III | 98 | Continuous infusion had higher complication rate. But also utilized a local anesthetic. |
V Summary
In identifying the patients at high risk for morbidity and mortality from blunt chest trauma, outcome clearly worsens with increasing numbers of rib fractures and increasing age. However, identifying a true “inflection point” in the morality curve at which to apply our resources is difficult for either of these parameters. Additionally, as a marker of overall injury severity, it is unclear to what extent ameliorating the effects of fractures themselves will improve outcome. Consequently, studies such as those by Svennevig[10] which identify rib fractures as an independent predictor of mortality are the most valuable. Yet, it should be remembered that the mortality identified in all studies is nonetheless real, and attempts to minimize the thoracic contribution to that mortality is appropriate for those patients at significant risk of dying.
While it is clear that certain analgesic modalities improve subjective pain sensation, the importance of this to recovery, other than in the humanistic sense is unclear. While improvement in objective pulmonary function can clearly be documented, the correlation of this to outcome remains somewhat elusive. Just how much improvement in vital capacity is needed to significantly impact ventilator days, or ICU length of stay, or survival? While most would conceptually agree that improved pulmonary parameters are a good sign in blunt chest injury, the factors affecting outcome particularly in multi-trauma patients are complex and interwoven. Significant populations of isolated chest-injured patients are difficult to mobilize for study. Studies derived from elective thoracic surgery are certainly more available and clearly deal with isolated chest wall pain. However their validity as models of trauma patients are questionable at best, at least in terms of outcome measures.
As far as effectiveness and complication rates for various modalities, it is reasonable to assume that regional anesthetic techniques, like surgical procedures, have a significant learning curve. Lack of experience with a given modality may contribute to lower success rates and increased complications thereby negatively impacting on the tendency for future investigation.. Modalities such as intrapleural, extrapleural or paravertebral analgesia may have greater potential for safety than has been realized and fewer contraindications which may thus augment their applicability to a trauma population. If efficacy were adequately documented, each of the described modalities offers the promise of it’s own unique advantages which would further enhance the armamentarium and pain control flexibility of the trauma surgeon and trauma anesthesiologist. However, the only analgesic modality for which widespread experience exists today in trauma patients is that of epidural administration of narcotics and anesthetics. It is clear that epidural administration of narcotic / analgesic combinations are highly effective in controlling subjective pain and improving pulmonary function. In experienced hands its’ rate of complication is minimal and of significant morbidity virtually negligable. Contraindications particularly prevalent in the trauma patient, such as slightly abnormal coagulation, spinal fractures and fever may limit its use though the extent to which this occurs is not known.
Consequent to the above issues, this group’s recommendations reflect what is known and reasonable regarding identification of those patients at risk from blunt thoracic injury and those analgesic modalities most likely to provide a net positive effect on their outcome.
VI Areas for Future Development
Based on assessment of current and recent work, the following areas are appropriate for further research:
- Outcome studies regarding epidural analgesia in trauma patients -the effect on primary outcomes of this widely used modality needs to be better defined.
- Outcome studies involving pulmonary function parameters - A correlation needs to be established between improvements in pulmonary function and outcome measures so as to define specific physiologic goals for therapies
- Effectiveness / safety of other modalities. – additional investigations need to further evaluate the basic and comparative efficacy of intrapleural, paravertebral / extrapleural and intercostal modalities. Each of these modalities holds the promise of specific advantages and could extend the flexibility of analgesia if efficacy and safety could be better defined.
- New Frontiers – Emerging modalities such as liposomal –encapsulated anesthetic agents (ref) offer the potential for safer and more prolonged regional anesthesia. Trauma surgeons should partner with anesthesiologists to evaluate the applicability of new analgesic modalities for thoracic trauma patients.
References
- Wilson RF, Steiger Z: Thoracic Trauma: Chest Wall and Lung. In Wilson RF, Walt AJ (eds) Management of Trauma: Pitfalls and Practices. Baltimore, Md. Williams & Wilkins, 1996, pps 319-339
- Rodriguez A: Injuries of the Chest Wall, the Lungs and the Pleura. In Turney SZ, Rodriquez A, Cowley RA (eds)Management of Cardiothoracic Trauma. Baltimore, Md. Williams & Wilkins, 1990, pps 155-178
- Ziegler AW, Agarwal NN: Morbidity and Mortality of Rib Fractures. J Trauma. 1994;37:975-979
- Shorr RM, Crittenden M, Indeck M, Hartunian S, Cowley RA. Blunt thoracic trauma: analysis of 515 patients. Ann Surg 1987;206: 200-205
- Newman RJ, Phil D, Jones IS. A prospective study of 413 consecutive car occupants with chest injuries. J Trauma 1984;24: 129-135
- Palvanen M, Kannus P,Niemi S, Pakkari J, Vuori I. Epidemiology of minimal trauma rib fractures in the elderly. Calcif Tissue Int.1998;62: 274-277
- Trunkey DD: Cervicothoracic Trauma. In Blaisdell FW, Trunkey DD (eds) Trauma Management Vol III. New York, Thieme, 1986
- Bolliger CT, Van Eeden SF. Treatment of multiple rib fracture: randomized controlled trial comparing ventilatory with nonventilatory management Chest 1990;97:943-948
- Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma . 2000;48:1040-1047
- Svennevig JL, Bugge-Asperheim B, Geiran OR, et al. Prognostic factors in blunt chest trauma: analysis of 652 cases. Ann Chir Gynaecol. 1986;75:8-14
- Shorr RM, Rodriguez A, Indeck MC, Crittenden MD, Hartunian S, Cowley RA. Blunt chest trauma in the elderly. J Trauma 1989;29: 234-237
- Cameron P, Dziukas L, Hadj A, Clark P, Hooper S. rib fractures in major trauma Aust N Z J Surg. 1996;66:530-534
- Barnea Y, Kashtan H, Shornick Y, Werbin N. Isolated rib fractures in elderly patients: morality and morbidity. Can J Surg. 2002;45:43-46
- Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: Flail chest vs pulmonary contusion. J Trauma. 1988;28:298-304
- Sanchez-Lloret J, Letang E, Mateau M, et al. Indications and surgical treatment of the traumatic flail chest syndrome: an original technique. Thorac Cardiovasc Surg. 1982;30:294-297.
- Thomas AN, Blaisdell FW, Lewis FR Jr, Schlobohm RM. Operative stabilization for flail chest after blunt trauma. J Thorac Cardiovasc Surg. 1978;75:793-801.
- Blair E, Mills E. Rationale of stabilization of the flail chest with intermittent positive ventilation breathing. Am Surg. 1968;34:860-868.
- Cullen P, Model JH, Kirby RR, et al. Treatment of flail chest: Use of intermittent mandatory ventilation and positive end-expiratory pressure. Arch Surg 1975;110:1099-1103.
- Shackford SR, Smith DE, Jarins CK, et al. The management of flail chest: A comparison of ventilatory and non-ventilatory treatment. Am J Surg. 1976;132:759762.
- Richardson JD, Adams L, Flint LM. Selective management of flail chest and pulmonary contusion. Ann Surg. 1982;196:481
- Albaugh G, Kann B, Puc M, Vemulapalli P, et al. Age-adjusted outcomes in traumatic flail chest injuries in the elderly. Am Surgeon. 2000;66:978-981.
- EAST Ad Hoc Committee on Practice Management Guideline Development. Utilizing Evidence Based Outcome Measures to Develop Practice Management Guidelines: A Primer. Web-published; Eastern Association for the Surgery of Trauma. 2000 (www.east.org)
- Jadad AR, Moore RA, Carroll D,.et al. Assessing the Quality of reports of randomized clinical tirals.. Controlled Clinical Trials. 1996; 17: 1-12
- Findlay RT. Fractures of the scapula and ribs. Am J Surg 1937; 38:489
- Jensen NK. Recovery of pulmonary function after crushing injuries of the chest. Dis Chest 1952: 22:319
- Avery EE, Moerch ET, Benson DW. Critically crushed chests. J Thorac Cardiovasc Surg 1956; 32:291-309
- Trinkle JK, Richardson JA, Trany JL, Grover FL, et al. Management of flail chest without mechanical ventilation. Ann Thorac Surg 1975; 19:355-63
- Dittmann M, Ferstl A, Wolff G. Epidural analgesia for the treatment of multiple rib fractures. Europ J Intensive Care Med. 1975; 1:71-75
- Dittmann M, Keller R, Wolff G. A rationale for epidural analgesia in the treatment of multiple rib fractures. Intensive Care Med. 1978; 4:193-197
- Gibbons J, James O, Quail A, et al . Relief of pain in chest injury. Br J Anaesth. 1973; 45:1136-38
- O’Kelly E. Continuous pain relief for multiple fractures ribs. Br J Anaesth 1981; 53:989-91
- Abouhatem R, Hendrickx P, Titeca M. Thoracic epidural analgesia for fractured ribs and postoperative analgesia. Acta anaesth Belg 1984; 35:271-75
- Garzon AA, Seltzer B, Karlson KE. Pathophysiology of crushed chest injuries. Ann Surg 1968; 168:128-36
- Craven KD, Oppenheimer L, Wood LDH. Effects of contusion and flail chest on pulmonary perfusion and oxygen exchange. J Appl Physiol 1979; 47:729-37
- Roscher R, Bittner R, Stockmann U. Pulmonary contusion. Arch Surg 1974; 109:508-10
- Jette NT, Barash PG. Treatment of a flail injury of the chest. Anaesthesia 1977; 32:475-79
- Luchette FA, Radafshar SMN, Kaiser R, et al. Prospective evaluation of epidural versus intrapleural catheters for analgesia in chest wall trauma. J Trauma 1994; 36:865-70
- Shinohara K, Iwama H, Akama Y, et al. Intrapleural block for patients with multiple rib fractures: Comparison with epidural block. J Emerg Med 1994; 12:441-46
- Ullman DA, Wimpy RE, Fortune JB, et al. The treatment of patients with multiple rib fractures using continuous thoracic epidural narcotic infusions. Regional Anesth. 1989; 14:43-47
- Wisner DH. A stepwise logistic regression analysis of factors affecting morbidity and mortality after thoracic trauma: Effect of epidural analgesia. J Trauma 1990; 30:799-805
- O’Kelly E, Garry B. Continuous pain relief for multiple fractured ribs. Br J Anaesth. 1981; 53:989-91
- Mackersie RC, Karagianes TG, Hoyt DB, et al. Prospective evaluation of epidural and intravenous administration of fentanyl for pain control and restoration of ventilatory function following multiple rib fractures. J Trauma. 1991; 31:443-49
- Haenel JB, Moore FA, Moore EE, et al. Extrapleural Bupivicaine for amelioration of multiple rib fractures. 1995; 38:22-27.
- Moon MR, Luchette FA, Gibson SW, et al. Prospective, randomized comparison of epidural versus parenteral opioid analgesia in thoracic trauma. Amer Surg 1999; 229:684-92.
- Karmakar MJ, Ho AM, Acute pain management of patients with multiple rib fractures. J Trauma 2003; 54:615-25.
- Rankin AP, Comber RE. Management of fifty cases of chest injury with a regimen of epidural bupivacaine and morphine. Anaesth Intens Care 1984; 12:311-14.
- Worthley LI. Thoracic epidural in the management of chest trauma. Intensive Care Med 1985; 11:312-15.
- Romer HC, Russell GN. A survey of the practice of thoracic epidural analgesia in the United Kingdom. Anaesthesia. 1998; 53:1016-22.
- Doss NW, Veliyaniparambil I, Krishnan R, et al. Continuous thoracic epidural ropivacaine drips for multiple rib fractures. Proc West Pharmacol Soc 1999; 42: 99-100.
- Govindrajan R, Bakalova T, Michael R, et al. Epidural buprenorphine in management of pain in multiple rib fractures. Acta Anaesthesiol Scand 2002; 46:660-65.
- Johnston JR, McCaughey W. Epidural morphine: a method of management of multiple fractured ribs. Anaesthesia. 1980; 35:155-7.
- Ward AJ, Gillatt DA. Delayed diagnosis of traumatic rupture of the spleen: a warning of the use of thoracic epidural analgesia in chest trauma. Injury 1989; 20:178-9
- Ready LB, Loper KA, Nessly M, et al. Postoperative epidural morphine is safe on surgical wards. Anesthesiology. 1991; 75:452-6
- Murphy DF. Intercostal nerve block for fractured ribs and postoperative analgesia. Regional Anesthesia. 1983; 8:151-3
- Shafei H, Chamberlain M, Natrajan K, et al. Intrapleural bupivacaine for early post-thoracotomy analgesia; Comparison with bupivacaine intercostal block and cryofreezing. Thorac. Cardiovasc. Surgeon 1990; 38:38-41.
- Bachmann-Mennenga B, Biscoping J, Kuhn DF, et al. Intercostal nerve block, interpleural analgesia, thoracic epidural block or systemic opioid application for pain relief after thoracotomy. Eur J Cardiothoracic Surg. 1993; 7:12-18.
- Pedersen VM, Schulze S, Hoier-Madsen K, et al. Air flow meter assessment of the effect of intercostal nerve blockade on respiratory function in rib fractures. Acta Chir Scand. 1983; 149:119-20.
- Shanti CM, Carlin AM, Tyburski JG. Incidence of pneumothorax from intercostal nerve blocks for analgesia in rib fractures. J Trauma. 2001; 51:536-9.
- Baxter AD, Flynn JF, Jennings FO. Continuous intercostal nerve blockade. Br J Anaesth. 1984; 56:665-6
- Crossley AW, Hosie He. Radiographic study of intercostal nerve blockade in healthy volunteers. Br J Anaesth. 1987; 59:149-54
- Mowbray A, Wong KK, Murray JM. Intercostal catheterization; an alternative approach to the paravertebral space. Anaesthesia. 1987; 42:958-61.
- Kvalheim L, Reiestad F. Interpleural catheter in the management of postoperative pain. Anesthesiology. 1984; 61:A231
- Graziotti PJ, Smith GB. Multiple rib fractures and head injury: an indication for intercostal catheterisation and infusion of local anaesthetics. Anaesthesia. 1988; 43:964-6
- Knottennelt JD, James MF, Bloomfield M. Intrapleural bupivacaine analgesia in chest trauma: a randomized double-blind controlled trial. Injury. 1991; 22:114-116.
- Hudes ET. Continuous infusion interpleural analgesia for multiple fractured ribs. Can J Anaesth. 1990; 37:705.
- Richardson J, Sabanathan S, Mearns AJ, et al. A prospective randomized comparison of interpleural and paravertebral analgesia in thoracic surgery. Br J Anaesth. 1995; 75:405-8.
- Ferrante FM, Chan VW, Arthur GR, et al Interpleural analgesia after thoracotomy. Anesth Analg. 1991; 72:105-9.
- Short K, Scheeres D, Mlakar J, et al. Evaluation of intrapleural analgesia in the management of blunt traumatic chest wall pain: A clinical trial. Am Surg. 1996; 62:488-93.
- Seltzer JL, Larijani GE, Goldberg ME, et al. Intrapleural bupivacaine: a kinetic and dynamic evaluation. Anaesthesiology. 1987; 67:798-800.
- Gilbert J, Hultman J. Thoracic paravertebral block: a method of pain control. Acta Anaesthesiol Scand. 1989; 33:142-5.
- Williamson S, Kumar CM. Paravertebral block in head injured patient with chest trauma. Anaesthesia. 1997; 52:284-5.
- Cheema SP, Ilsley D, Richardson J, et al. A thermographic study of paravertebral analgesia. Anaesthesia. 1995; 50:118-21.
- Richardson J, Lonnqvist PA. Thoracic paravertebral Block. Br J Anaesth 1998; 81:230-8.
- Karmakar MK. Thoracic paravertebral block. Anaesthesiology 2001; 95:771-80
- Lonnqvist PA, MacKenzie J, Soni AK. Paravertebral blockade: failure rate and complicatons. Anaesthesia. 1995; 50:813-15.
- Karmakar MJ, Critchley AH, Ho AM, et al. Continous thoracic paravertebral infusion of Bupivicaine in patients with multiple rib fractures. Chest. 2003; 123:424-31.
- Eason MJ, Wyatt R. Paravertebral thoracic block: a reappraisal. Anaesthesia. 1979; 34:638-42.
- Sariego J, Brown JL, Matsumoto T. Predictors of pulmonary complications in blunt chest trauma. Int Surg 1993; 78:320-23.
- Svennevig JL, Bugge-Asperheim B, Geiran OR. Prognostic factors in blunt chest trauma: Analysis of 652 cases. Annales Chirurgiae et Gynaecologiae. 1986; 75:8-14.
- Lee RB, Bass SM, Morris JA. Three or more rib fractures as an indicator for transfer to a level I trauma center: A population-based study. J Trauma. 1990; 30:689-95.
- Ziegler V, Agarwal NA. Morbidity and mortality of rib fractures. J Trauma 1994; 37:975-79.
- Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at a greater risk of death and pneumonia. J Trauma 2002; 54:478-85.
- Bulger EM, Arneson MA, Mock CN. Rib fractures in the elderly. J Trauma 2000; 48:1040-47.
- Barnea Y, Kashtan H, Skomick Y, et al. Isolated rib fractures in elderly patients: mortality and morbidity. Can J Surg 2002; 45:43-46.
- Alexander JQ, Gutierrez CJ, Mariano MC. Blunt chest trauma in the elderly patient: How cardiopulmonary disease affects outcome. American Surgeon 2000; 9:855-57.
- Oreskovich MR, Howard JD, Copass MK, Carrico CJ. Geriatric trauma: injury patterns and outcome. J Trauma. 1984; 24:565-72
- DeMaria EJ, Kenney PR, Merriam MA, Et al . Survival after trauma in geriatric patients. Ann Surg. 1987; 206:738-43.
- Horst HM, Obeid FN, Sorenson VJ, et al. Factors influencing survival of eldery trauma patients. Crit Care Med. 1986; 14:681-84.
- Della Rocca G. Post-thoracotomy analgesia: epidural vs. IV morphine continuous infusion Minerva Anestesiol. 2003; 68:681-93.
- KOH SO, Kim JHO, Oh HK. Effects of epidural morphine on ventilatory function in chest trauma and thoracotomy patients. Yonsei Med J 1991; 32:250-54.
- Mackersie RC, Shackford SR, Hoyt DB, et al. Continuous epidural fentanyl analgesia: Ventilatory function improvement with routine use in treatment of blunt chest injury. J Trauma 1987; 27:1207-12.
- Wu CL, Jani ND, Perkins FM, et al . Thoracic epidural analgesia versus intravenous patient-controlled analgesia for the treatment of rib fracture pain after motor vehicle crash. J Trauma 1999; 47:564-67.
- Shulman M, Sandler AN, Bradley JW, et al. Post-thoracotomy pain and pulmonary function following epidural and systemic morphine. Anesthesiology 1984; 61:56975.
- Logas WG, El-Ganzouri A, et al. Continuous thoracic epidural analgesia for postoperative pain relief following thoracotomy: A randomized prospective study. Anesthesiology. 1987; 67:787-91.
- Saliomaki TE, Laitinen JO, Nuutinen LS. A randomized double-blind comparisonof epidural vs. intravenous fentanyl infusion for analgesia after thoracotomy. Anesthesiology 1991; 75:790-795.
- Sandler AN, Stringer D, Panos L, et al A randomized double-blind comparison of lumbar epidural and intravenous fentanyl infusions for post-thoracotomy pain relief. Anesthesiology 1992; 77:626-34.
- Flisberg P. Pain relief and safety after major surgery: Prospective study of epidural and IV analgesia in 2696 patients. Acta Anesthesiol Scand 2003; 47:457-65.
- McKnight CK, Marshall M. Monoplatythela and paravertebral block. Anaesthesia 1984; 39:1147.
- Karmakar MK, Kwok WH, Kew J. Thoracic paravertebral block: radiological evidence of contralateral spread anterior to the vertebral bodies. Br J Anaesth. 2000; 84: 263-265.
- Karmakar MK, Chio PT, Joynt GM, et al. Thoracic paravertebral block for management of pain associated with multiple fractured ribs in patients with concomitant lumbar spinal trauma. Reg Anesth Pain Med. 2001; 26:169-73.
- Sabanathan S, Mearns AJ, Bicvkford-Smith PJ, et al. Efficacy of continuous extrapleural intercostal nerve block post-thoracotomy pain and pulmonary mechanics. Br J Surg. 1990; 77:221
- Dryden CM, McMenemin I , Duthie DJR. Efficacy of continuous intercostal bupivacaine for pain relief after thoracotomy. Br J Anaesth 1993; 70:508.
- Deneuville M, Bisserier A, Regnard JF, et al. Continuous intercostal analgesia with .5% bupivacaine after thoracotomy: A randomized study. Ann Thorac Surg 1991; 55:381
- Gabram SG, Schwartz RJ, Jacobs LM, et al. Clinical management of patients with unilateral rib fractures: A randomized trial. World J Surg. 1995; 19:388-93.
- Schneider RF, Villamena PC, Harvey J, et al. Lack of efficacy of intrapleural Bupivacaine for postoperative analgesia following thoracotomy. Chest 1993; 103:414-16
- Scherer R, Schmutzler M, Giehler R, et al. Complications related to thoracic epidural analgesia: a prospective study of 10771 surgical patients. Acta Anaesthesiol Scand 1993; 37:370-374.
- Ready LB. Postoperative epidural morphine is safe on surgical wards. Anaesthesiology 1991; 75:452-56.
- U.S. Dept. of Health and Human Services. FDA Public Health Advisory. Webpubished: www.fda.gov/medwatch/safety/1997/antico.htm 1997
- U.S. Dept. of Health and Human Services. FDA Talk Paper: Health advisory for certain anticoagulant drugs (Low molecular weight heparins and heparinoids) Web-published: www.fda.gov/bbs/topics/ANSWERS/ANS00839.html. 1997
- Gomez MN, Symreng T, Johnson B. Intrapleural Bupivacaine for intraoperative analgesia – A dangerous technique? Anesth Analg 1987; 67:S1-S266
- Cicala RS, Voelter GR, Fox T, et al. Epidural analgesia in thoracic trauma: Effects of lumbar morphine and thoracic bupivacaine on pulmonary function. Crit Care Med. 1990; 18:229-31.
- Wiebalck A, Brodner G, Van Aken H. The effects of adding sufentanil to bupivacaine for postoperative patient-controlled epidural analgesia. Anesth Analg 1997; 85:124-9.
- Hansdottir V, Bake B, Nordberg G. The analgesic efficacy and adverse effects of continuous epidural sufentanil and bupivacaine infusion after thoracotomy. Anesth Analg 1996; 83:394-400.
- Kurek SJ, Lagares-Garcia J, Casella R, et al. Complications of epidural infusions for analgesia in postoperative and trauma patients. Am Surg 1997; 63:543-6.
Evidentiary Tables
| First Author | Year | Reference | Data Class | Conclusions |
|---|---|---|---|---|
| **Technologic assessment., Bold = class I evidence | ||||
| Definition, epidemiology, and natural history of blunt chest trauma related to pain management (7) | ||||
| Collie JA | 1967 | Practical points in the treatment of chest injuries. Anaesthesia. 22:392399 | III | Two year retrospective British review of BCT; the primary interest is historic perspective. Non-controlled, non-comparative description of thoracic extradural analgesia |
| Livingston DH | 1990 | Pulmonary disability after severe blunt chest trauma. J Trauma. 30:562-67 | II | A prospective, non-randomized series describing long-term recovery from BCT. As Determined by serial PFT’s recovery occurs in most patients by 4 months. |
| Kishikawa M | 1991 | Pulmonary contusion causes long-term respiratory dysfunction with decreased functional residual capacity. J Trauma. 31:1203-10. | II | Another small, prospective and randomized series on long-term recovery from BCT, this time from Japan, and focusing on pulmonary contusion. |
| Moore FA | 1993 | Blunt pulmonary injury. Adv in Trauma and Crit Care. 8:1-28 | III | Well-referenced (N=156) review article discussing the broad topic of BCT, with emphasis on clinical management. |
| Ferguson M | 1996 | Management of blunt chest injury. Resp Care Clin No Amer. 2:449-466 | III | An excellent review article on BCT and pain management techniques. |
| D’Amours RH | 1998 | Pathogenesis and management of postthoracotomy pain. Chest Surg Clin of North Amer. 8:703-22. | III | Review article on a topic with limited application to BCT. |
| Domino KB | 1999 | Evaluation, preparation, and management of the surgical patient with respiratory disease. Cont Surg 54:41-49 | III | Review of respiratory care issues in the surgical patient. |
| Indications for invasive pain management in BCT (population at risk) (10) | ||||
| Svennevig JL | 1986 | Prognostic Factors in Blunt Chest Trauma: Analysis of 652 Cases. Annales Chirurgiae et Gynaecologiae 75: 8-14 | II | Very large retrospective series with ex cellent statistical validation assessing risk factors for poor outcome in blunt chest trauma. Age>70 and four or more rib fractures was associated with dramatically increased motality (<4 fx = 2.5%; >4 fx = 19%) |
| Lee RB | 1990 | Three or More Rib Fractures as an Indicator for Transfer to a Level I Trauma Center: A Population-based study. J Trauma 30: 689-695 | III | A large statewide registry review of all discharged patient with rib fractures. Number of fractures >3 predicted increased hospital stay, ICU stay and ISS. The authors felt that 3 or more rib fractures thus warranted trauma center care. Since the groups were not corrected for differing ISS, the morbidity of the chest injury itself cannot be separated from the overall increased injury severity of which the rib fractures are a marker. The authors did notice that mortality increased at a faster rate with age for the group with 3 or more fractures. |
| Hoyt DB | 1993 | A risk analysis of pulmonary complications following major trauma. J Trauma. 35:524-31 | II | A prospective observational study. Pulmonary complications occurred in 11.2% of 3,289 patients meeting Major Trauma Outcome Study criteria, representing one third of all disease-related complications. Risk factors are discussed though chest injury was not isolated as a a cause of pulmonary morbidity. Little discussion of pain management. |
| Sariego J | 1993 | Predictors of Pulmonary Complications in Blunt Chest Trauma. Int Surg 78: 320-323 | III | A thorough descriptive, retrospective review of the thoracic complications of BCT. Delayed complications in the thorax occurred in 30% of 98 studied patients. While trauma score and ISS predicted morality as expected, they did not identify patients who developed delayed complications. |
| Ziegler V | 1994 | Morbidity and Mortality of Rib Fractures. J Trauma 37: 975-979 | III | A retrospective registry review of the mortality of rib fractures (n=711) Mortality with 1-2 fractures was 5% but rose to 13% with 4 fractures and 29% with > 7 fractures.. There was no significant difference in mortality between the various age groups, but groups were not defined as equivalent in ISS. The ISS increased with the number of fractures. Therefore, the relative contributions of pulmonary morbidity and distant injury could not be separated. Thus, the morality risk of chest injury alone could not be assessed. |
| Alexander JQ | 2000 | Blunt Chest Trauma in the Elderly Patient: How Cardiopulmonary Disease Affects Outcome. American Surgeon 9: 855-857 | III | A registry review study identifying fact that elderly patients (>65) with cardiopulmonary disease (CPD) had significantly higher mortality, morbidity and length of stay. The only deaths in the study occurred in the CPD+patients. Sample size was modest but study was adequately powered due to highly significant findings. |
| Albaugh G | 2000 | Age-Adjusted Outcomes in Traumatic Flail Chest Injuries in the Elderly. American Surgeon 66: 978981 | III | A retrospective registry review of 58 patients with flail chest injuries divided into <70 year and > 70 year groups. The risk of death increased by a factor of 2.3 for every 10 years above age 20. No inflection point in the mortality curve was identified. Possible shortcomings: study size was small and DOAs were excluded. Correction was not made for comorbidities so the isolated contribution of age cannot be fully assessed. Nonetheless, study supports findings of other works. |
| Bulger EM | 2000 | Rib Fractures in the Elderly. J Trauma 48: 1040-1047 | II | A large retrospective cohort study of 277 patients > age 65 with multiple rib fractures vs a random control of 187 patients under age 65 with a similar chest AIS. The older group had twice the mortality (22% v 10%) and pulmonary morbidity (31% pneumonia vs 17%). For each additional rib fracture in the elderly, mortality increased by 20% and morbidity ( pneumonia) by 27%. A particularly increased risk of mortality and morbidity could be assigned to each rib fracture >4. Though study was retrospective, sample size was large and data and statistics were clearly reliable. |
| Barnea Y | 2002 | Isolated Rib Fractures in Elderly Patients: mortality and morbidity Canadian Journal of Surgery 45:4346 | III | A retrospective review of a moderate size population (n=77) of elderly patients (age>65) admitted with isolated rib fractures. There was strong association between mortality and the co-morbidities of CHF (p=.001) and diabetes. (p=.0095). Low SaO2 at admission correlated with mortality (p=.0009) though exact level was not mentioned. With the study size a significant association between number of rib fractures and mortality could not be made though there was a trend to positive correlation. Small retrospective study but strong correlation achieved for factors identified. |
| Bergeron E | 2002 | Elderly Trauma Patients with Rib Fractures are at Greater Risk of Death and Pneumonia. J Trauma 54:478-85 | II | A prospective cohort study of 405 patients with rib fractures. When adjusting for ISS, TS, Co-morbidities, multiplicity of fractures, the > 65 group had 5 times the odds of dying compared to the < 65 age group. Authors concluded that particular attention and aggressive treatment should be provided to this cohort. |
| Pain management modalities in blunt chest trauma (33) | ||||
| Gibbons J | 1973 | Relief of pain in chest injury. Brit J Anaesth. 45:1136-38 | II | Early prospective observational study of 60 BCT patients. The subgroup undergoing epidural analgesia (EA) required ventilator support at half the frequency to those with intercostal blocks or IV narcotics.. Methodologic limitations include lack of control group or randomization, possibly introducing selection bias. |
| Dittmann M | 1975 | Epidural analgesia for the treatment of multiple rib fractures. Europ J Intensive Care Med. 1:71-75 | III | An elegant, early study of the role of EA in BCT patients, and using bedside objective measures before and after the analgesia to gauge its effectiveness. Identified significant improvements in V.C. with epidural. Authors implied that epidural analgesic use allowed avoidance of mechanical ventilation. However patients were not randomly selected and controls were historical and unmatched. Nonetheless, this study demonstrated early recognition of the importance of pain control and the desirability of avoiding mechanical ventilation. |
| Dittman M | 1978 | A rationale for epidural analgesia in the treatment of multiple rib fractures. Intensive Care Med. 4:19397 | II | Larger, prospective follow-up study to the previous one, comparing mechanical ventilation (without EA) to breathing spontaneously with EA. Methodologic problems with non-controlled groups in that criteria for epidural group may have selected out less injured patients. Some of these patients may have done well without epidural. Nonetheless, this was an important early study demonstrating that patients with chest wall trauma can be managed off ventilator assisted with epidural analgesia. Also demonstrated improved PFTS in selected patients. |
| O’Kelly E | 1981 | Continuous pain relief for multiple fractured ribs. Br J Anaesth. 53:98991 | na | Case report of the use of a continuous exptrapleural catheter for analgesia in BCT. |
| Dittman M | 1982 | Epidural analgesia or mechanical ventilation for multiple rib fractures? Intensive Care Med. 8:89-92 | II | Largest clinical Swiss trial (N=283), demonstrates that EA restores respiratory mechanics and decreases pulmonary complications compared to mechanical ventilation. Unfortunately, is neither randomized nor controlled. The less critically ill patients were pre-selected for epidurals opposed to obligatory ventilation. Did demonstrate that mechanical ventilation no necessarily indicated based on anatomic extent of injury alone. |
| Murphy DF | 1983 | Intercostal Nerve Block for Fractured Ribs and Postoperative Analgesia. Regional Anesthesia 8: 151-153 | III | A purely descriptive analysis of continuous intercostal administration of a long acting anesthetic via a catheter in the chest wall of 57 postoperative thoracic patients.. Anesthesia was maintained over a number o days with minimal morbidity. There were no pneumothoraces. This study constitutes “expert opinion” only and the author suggests the technique for use and further study. |
| Abouhatem R | 1984 | Thoracic epidural analgesia in the treatment of rib fractures. Acta anaesth. Belg. 35:271-75 | III | Early, Beligian experience with EA. Small, non-randomized, non-controlled observational, series. Authors noted good pain control in epidural patients, but no objective measures were used. While no statistical analysis was done, this is an elegant description of the importance of pain relief, rather than intubation per se, in the successful management of BCT. |
| Rankin AN | 1984 | Management of fifty cases of chest injury with a regimen of epidural bupivacaine and morphine. Anaesth Intens Care 12:311-14 | II | Prospective trial of EA, but descriptive in nature, neither randomized nor controlled. Combined epidural bupivacaine with epidural morphine for best results. 43/50 patients recovered without ventilatory support. No control group for comparison with other modalities. Complications were rare with one case of respiratory depression not requiring intubation and one possible case of meningitis responding to antibiotics and catheter removal. |
| Worthley LG | 1985 | Thoracic epidural in the management of chest trauma. Intensive Care Med. 11:312-15 | II | Non-controlled prospective cohort study suggests that intermittent bolus EA in BCT improves respiratory function without the need for mechanical ventilation in most patients. Vital capacity doubled after initial dose. Complications were 17% hypotension responding to fluids; 13% urinary retention; 4% dural puncture and one epidural abscess responding to antibiotics. Authors conclude epidural very effective but not without complications. Should be considered only in patients unable to cough effectively with IV medication. Large sample (n=147) but no statistics. Patients with other injuries and comorbidities were included. |
| Dickson GR | 1986 | Intrathecal Morphine and Multiple Rib Fractures. British Journal of Anaesthesia 1986 | III | A small retrospective series (n=19) of chest injury patients treated with the now rarely used technique of intrathecal anesthesia. Patients so treated had been unsuitable for epidural (EA) for various reasons. Subjective pain relief was described as “good” though no objective measures or statistical analysis were provided. Complications were frequent though none serious. Authors anecdotally felt epidural was more effective but recommended intrathecal when EA was contraindicated. |
| Mackersie RC | 1987 | Continuous epidural fentanyl analgesia: Ventilatory function improvement with routine use in treatment of blunt chest injury. J Trauma. 27:1207-12 | III | A non-randomized, non-controlled retrospective study of 40 patients in an 18 month period who received fentanyl via continuous epidural. Significant improvements in VC and Max Insp.Pressure. and slight improvements in Ve and TV. 85% had good pain relief. Complications minimal. The authors conclude that fentanyl via EA is safe and effective. |
| Graziotti PJ | 1988 | Multiple rib fractures and head injury – an indication for intercostal catheterization and infusion of local anaesthetics. Anaesthesia. 43:964-66 | na | Case presentation (British) of intercostal catheterization for infusion of extra/intrapleural local anesthetic agents in BCT |
| Ullman DA | 1989 | The treatment of patients with multiple rib fractures using continuous thoracic epidural narcotic infusion. Regional Anesth. 14:43-47 | I Jadad 3 | Prospective, randomized series demonstrated lower rates of tracheostomy, and shorter ventilator, ICU and hospital lengths of stay in the EA (narcotic) group vs. control (IV narcotic). High level of stat. sig. Despite small study size |
| Gilbert J | 1989 | Thoracic paravertebral block: a method of pain control. Acta Anaesthesiol Scand. 33:142-45 | II | Single author’s observational series of 10 BCT patients undergoing single large dose paravertebral injection of local anesthetic. Subjective pain, respiratory parameters and need for repeat injection were endponts. Significance was achieved in terms of pain control and respiratory rate but not in spirometry. Study limited by small sample and lack of objective pain criteria. Mean duration of therapy <10 hours, placing this modality in the category of rib block both for technique and duration. of action. Applicability in trauma remains unclear from this study. |
| Cicala RS | 1990 | Epidural analgesia in thoracic trauma: Effects of lumbar morphine and thoracic bupivacaine on pulmonary function. Crit Care Med. 18:229-231 | I Jadad 3 | Prospective, randomized series compared thoracic EA anesthetic to lumbar EA narcotic. Both were equally effective in pain relief, but the thoracic anesthetic was modestly superior in improving pulmonary function (as measured by PFTs). Small group sizes but achieved stat. sig. due to dramatic differences in FVC, FEV1. Did not compare actual outcome parameters (i.e. -vent days) |
| Wisner DH | 1990 | A stepwise logistic regression analysis of factors affecting morbidity and mortality after thoracic trauma: Effect of epidural analgesia. J Trauma. 30:799-805 | III | Retrospective review of the effect of EA in elderly BCT patients. (age>60; n=50) The epidural study group had more severe thoracic trauma as measured by AIS. Yet, the use of epidural was an independent predictor of decreased mortality and decreased incidence of pulmonary complications as compared to parenteral narcotics. |
| Ravalia A | 1990 | I.V. Alfentanil analgesia for physiotherapy following rib fractures. Brit J Anaesth. 64:746-48 | na | Unusual British case report on the use of IV Alfentanil in a case of BCT. |
| Knottenbel t JD | 1991 | Intrapleural bupivacaine analgesia in chest trauma: a randomized double-blind controlled trial. Injury. 22:114-116 | I* Jadad 5 | Well-designed trial of intrapleural bupivacaine for the relief of thoracic pain. Intrapleural catheter dramatically superior to placebo in a mixed penetrating and blunt trauma population.. However only subjective pain scale used; no objective measures such as PFTs. Intrapleural catheter was not compared to other modalities. |
| Mackersie RC | 1991 | Prospective evaluation of epidural and intravenous administration of fentanyl for pain control and restoration of ventilatory function following multiple rib fractures. J Trauma. 31:443-451 | I Jadad 3 | One of the first well-designed American papers to directly address the question of EA vs. intravenous opiate in the management of the BCT patient. Compared to intravenous, EA significantly improves maximum inspiratory effort and arterial blood gas. . Both modalities showed improved vital capacity but more so with EA. Subjective pain improvement was greater with EA but not to statistical significance. Authors felt EA was method of choice for high risk chest trauma patients. This was a strong study statistically. Cohorts were well matched. |
| KOH SO | 1991 | Effects of Epidural Morphine on Ventilatory Function in Chest Trauma and Thoracotomy Patients Yonsei Medical Journal 32: 250-254 | II | In a small mixed group of patients treated with epidural morphine had improved ventilatory function (TV, VC, NIF) and subjective pain score. PaCO2 did not differ. Differences in ventilator hours and ICU LOS did not achieve statistical significance. Study is at risk for Type II error due to small sample size and questionable commonality with control group. |
| O’Connor CJ | 1993 | Thoracic Epidural Analgesia: Physiologic effects and clinical applications. J Cardiothoracic Vasc Anesth. 7:521-25 | III | Review article describing technique, physiologic effects and application of thoracic EA in a variety of clinical settings. |
| Luchette FA | 1994 | Prospective evaluation of epidural versus intrapleural catheters for analgesia in chest wall trauma. J Trauma. 36:865-870 | I Jadad 3 | Using reduction of parenteral narcotic use and improvement in respiratory function tests (TV, NIF) as outcome measures, EA was superior to intrapleural analgesia in this prospective, randomized trial. Achieved stat. sig. despite low power due to dramatic differences in measured parameters |
| Shinohara K | 1994 | Intrapleural block for patients with multiple rib fractures: Comparison with epidural block. J Emerg Med. 12:441-446 | I Jadad 3 | Prospective, randomized non-blinded “cross-over” study examining both intrapleural (IP) and Epidural (EA) in the same patient. (n=17) Failure with one modality lead to use of the other. Pain relief as determined by an analog scale was similar with both modalities. Transient hypotension was more common with EA. Hypesthesia was bilateral and more prolonged with EA while it was unilateral with IP. .Authors conclude IP is technically easier, with fewer side effects and may be ideal for trauma patients who need chest tubes. Study suffers from small sample size and lack of objective pulmonary measures. The validity of the crossover method without independent controls is unclear. |
| Gabram SG | 1995 | Clinical management of blunt trauma patients with unilateral rib fractures: A randomized trial. World J Surg. 19:388-93 | I Jadad 3 | In comparing systemic narcotics to intrapleural catheters: for the most severely injured patients, (FVC<20%) the intrapleural catheter patients had greater improvements in forced vital capacity and required cross-over to a new mode of therapy or vent support one half as often as the systemic group. |
| Haenel JB | 1995 | Extrapleural Bupivicaine for Amelioration of Multiple Rib Fractures J Trauma 38:22-27 | II | Small (n=15) prospective non-randomized study of rib fracture patients who failed IV analgesic treatment. Intercostal catheters were placed for 3 days without complications. Mean spirometry doubled and there were significant improvements in visual analog pain scale. No patients required mechanical ventilation. Authors conclude this modality is safe, simple and effective. Shortcomings of study are small sample size and non-randomization |
| Short K | 1996 | Evaluation of intrapleural analgesia in the management of blunt traumatic chest wall pain: A clinical trial. Am Surg. 62:488-93 | I Jadad 5 | 16 non-intubated BCT patients were randomized to receive placebo vs. local anesthetic via an intrapleural catheter and subsequently evaluated for various clinical variables, e.g. performance on spirometry. No significant differences were found between the groups. Small sample size but adequate based on power analysis. |
| Romer HC | 1998 | A survey of the practice of thoracic epidural analgesia in the United Kingdom. Anaesthesia. 53:1016-1022 | III | 275 British hospitals surveyed on the practice of EA use, including issues such as who manages the catheters and where, and the commonest drugs used. |
| Moon MR | 1999 | Prospective, randomized comparison of epidural versus parenteral opioid analgesia in thoracic trauma. Ann Surg. 229:684-92 | I Jadad 3 | An important study, with excellent methodology, relevant to BCT. In comparing the effects of EA and patient-controlled anesthesia (PCA), EA was associated with superior pain relief, improved pulmonary function and reduction in IL-8, proinflammatory cytokine. MIF, Vt and subjective pain control improved through study (day 1-3) with Epidural and decreased for PCA. LOS and ventilator use could not be assessed due to small sample size. (n=24) |
| Doss NW | 1999 | Continuous Thoracic Epidural Ropivacaine Drips for Multiple Rib Fractures. Proc. West. Parmacol. Soc. 42: 99-100 | III | A small retrospective review (n=57) of subjective pain relief with continuous thoracic epidural anesthesia (CTEA) in multiple rib fractures. No objective measures. The authors noted that this route offered good pain relief. |
| Wu CL | 1999 | Thoracic Epidural Analgesia versus Intravenous Patient-Controlled Analgesia for the Treatment of Rib Fracture Pain after Motor Vehicle Crash J Trauma 47:564-567 | III | A retrospective registry review: TEA with bupivicaine and fentanyl vs IV PCA with morphine for 64 patients with >3 rib fractures s/p MVC. Though the TEA patients had significantly more rib fractures and were significantly older, they had consistently lower pain scores at all times. No objective parameters were measured. No difference in complications or LOS was noted but the sample size was small and study may have been under-powered. |
| Govindrajan R | 2002 | Epidural buprenorphine in management of pain in multiple rib fractures. Acta Anaesthesiol Scand 46: 660-665 | II | Prospective non-controlled, non-randomized study of efficacy of epidural narcotic in setting of multiple rib fractures. Epidural produced significant improvements in PFTS (VC, TV, RR and Ve) and subjective pain rating on the 1st through 3rd days. Morbidity was minimal. Inclusion / exclusion criteria not well defined and sample size is small (N=27) leading to possibility of Type II error. Authors conclude that epidural narcotic delivery is efficacious in reduction of pain and improvement of ventilatory function. |
| Karmakar MJ | 2003 | Continuous Thoracic Paravertebral Infusion of Bupivicaine in Patients with Multiple Rib Fractures. Chest 123: 424-431 | II | Small prospective study of thoracic paravertebral anesthetic block (TPVB) in multiple rib fractures. (n=15) There was significant sustained improvement in subjective pain scale, respiratory function (RR, FVC, MEFR, SaO2). PCO2 was lower on day 4 though not initially. Hemodynamics were unaffected. There were no significant complications. Critical endponts such as pulmonary complications or ventilator days were not assessed. Therefore, improvement in respiratory function cannot be correlated with patient outcome. Also, limited by small sample size. |
| Karmaker MJ, Ho AM | 2003 | Acute pain management of patients with multiple rib fractures | n/a | Excellent, thorough review article of different modalities of analgesia for blunt thoracic trauma. |
| Pain management modadlities—non-blunt trauma studies (17) | ||||
| Shulman M | 1984 | Post-thoracotomy Pain and Pulmonary Function Following Epidural and SystemicMorphine Anesthesiology 61:569-575 | I Jadad 5 | PRCT, double-blinded, of lumbar epidural morphine vs IV morphine for the first day following thoracotomy. Epidural provided: significantly less pain , lower respiratory rate, higher FEV1 and FVC. ABG and somnolence score were unchanged. Authors conclude lumbar epidural is effective in alleviaing pain and improving respiratory function. Study is well composed with high validity assessment. |
| Fromme GA | 1985 | Comparison of Lumbar and Thoracic Epidural Morphine for Relief of Post-thoracotomy pain Anesth Analg 64:454-455 | III | Retrospective review of significant sample size (n=122) comparing lumbar and thoracic morphine for pain control after thoracotomy. With an endpoint of crossover to IV narcotics, both methods were equally efficacious. A slightly higher initial loading dose was required with the lumbar route. The authors conclude that either route equally efficacious. |
| Logas WG | 1987 | Contnous Thoracic Epidural Analgesia for Postoperative Pain Relief Following Thoracotomy: A Randomized Prospective Study Anesthesiology 67: 787-791 | I Jadad 5 | Prospective, randomized, controlled, double-blinded trial of 53 patients for elective thoracotomy. Patients divided into five groups (Epidural Morphine, epidural bupivicaine, morphene +bupivicaine, saline, IM morphine only) All analgesic modalities had stat sig. lower pain scores and supplemental narcotic use than epidural placebo. Epidural bupivicaine was no more effective than IM Morphine. Epidural morphine was twice as effective as either modality and the addition of bupivicaine to the morphine yielded even more effective pain control, to statistical significance. Complications were minimal. 4 patients had hypotension requiring pressors and one had respiratory depession requiring Narcan . These were not stat. associated with any one group. Landmark article; well designed with adequate sample size. Applicability to trauma unclear. |
| Symreng T | 1988 | Intrapleural Bupivacaine vs. Saline After Thoracotomy. Anesth Analg 67: S1-S266 | I Jadad 3 | Prospective, randomized, double-blinded, placebo-controlled trial of intrapleural bupivicaince vs. placebo after thoracotomy. Pain scores and PFTs were significantly increased at 30 minutes. IV morphine use decreased. Very small sample size. |
| Melendez JA | 1989 | Lumbar epidural fentanyl analgesia after thoracic surgery. J Cardiothoracic Anesth. 3:150-53 | II* | Prospective study demonstrating safety and efficacy of lumbar opiate EA in an elective thoracic surgery population*. There was significant reduction in pain based on a visual analog scale. There was no respiratory depression. (PaCO2 did not rise.) Non-randomized, lack of control group and small sample size (N=17) are further limitations of the study. |
| Shafei H | 1990 | Intrapleural Bupivacaine for early Post-Thoracotomy Analgesia. – Comparisom with Bupiacaine Intercostal Block and Cryofreezing. Thorac. Cardiovasc. Surgeon 38: 38-41 | I Jadad 2 | Prospective, randomized, controlled trial of intrapleural catheter with bupivicaine vs intercostal block in thoracotomy patients. (n=54) Fewer patients ikn the intrapleural catheter group required supplemental narcotics and the average narcotic dose was less in the first 2 postoperative days. No complications were noted. Authors conlucde that the modalities are comparable but that narcotic requirements may be reduced with intrapleural administration. Study was limited by small sample size. |
| Saliomaki TE | 1991 | A Randomized Double-blind Comparison of Epidural vs. Intravenous Fentanyl Infusion for Analgesia after Thoracotomy Anesthesiology 75:790-795 | I Jadad 4 | Prospective, randomized, double-blinded study of elective thoracotomy patients (n=20) comparing epidural fentanyl to intravenous morphine. Pain relief and respiratory function (RR and ABG) were significantly improved in the epidural group. Somnolence and nausea were significantly grater in the IV group. Both groups had small similar incidences of atelectasis and urinary retention. Authors conclude Epidural analgesic is superior to IV in terms of pain control, respiratory function and complication rate. Study suffers from small sample size and limited outcomes measured. |
| Sandler AN | 1992 | A Randomized Double-blind Comparison of Lumbar Epidural and Intravenous Fentanyl Infusions for Post-thoracotomy Pain Relief. Anesthesiology 77: 626634 | I Jadad 5 | PRCT doubled-blinded of healthy (ASA 1) post-thoracotomy patients comparing lumbar EDA (fentanyl) to IV fentanyl. Subjective pain control and respiratory depression as measured by pCO2 was not significantly different. Plasma fentanyl concentrations were similar.. Authors conclude EDA acts systemically and has little advantage over IV administation. Sample size was small and authors own power analysis yielded only a 54% chance of detecting differences. |
| Bachmann Mennenga B | 1993 | Intercostal nerve block (ICB), interpleural analgesia (IPA), thoracic epdural block (EDA) or systemic opioid (IVA) application for pain relief after thoracotomy | I Jadad 3 | A PRCT, non-blinded, of the effectiveness of these modalities for post-thoracotomy pain. (All except IV narcotic utilized bupivicaine). EDA and ICB produced the greatest pain relief to a high degree of significance (p<.01) and had significantly lower levels of breakthrough narcotic use. IPA had as much narcotic use as IV group even though catheter placement confirmed at surgery. Drop-off in bupivicaine levels led to postulate that chest tubes were draining off infusion. Epidural , though effective had least systemic absorption. Concluded that ICB and EDA most effective even though multi-level ICB technically cumbersome. IPA ineffective in this setting. Small numbers in each limb (10) but adequately powered. |
| Benzon HT | 1993 | A Randomized Double-Blind Comparison of Epidural Fentanyl Infusion vs. Patient-Controlled Analgesia with Morphine for Post-thoracotomy Pain. Anesth Analg 76:316-322 | I Jadad 5 | Prospective, randomized, double-blind, placebo-controlled study of CEFA (continuous epidural fentanyl analgesia) vs. morphine PCA in 36 post-thoracotomy patients. Visual analog score for pain control was significantly lower in the CEFA group. There was no difference in FVC. More patients in PCA group had significant sedation on POD#1 (p,.005) while more patients in the CEFA group had pruritis. The authors conclude that CEFA is superior for analgesia post-thoracotomy than PCA. |
| Hurford WE | 1993 | Comparison of thoracic and lumbar epidural infusions of bupivacaine and fentanyl for post-thoracotomy analgesia. J Cardiothoracic Vasc Anesth. 7:52125 | I* Jadad 3 | Prospective, randomized study of elective thoracotomy patients to compare thoracic vs. lumbar EA techniques. No difference in pain relief or side effects in post-thoracotomy patients was seen. However, sample size was small (n-45) and lumbar epidural required larger doses. Authors suggest that a dose-related increase in complication rate might be seen with a larger sample size. |
| Schneider RF | 1993 | Lack of efficacy of intrapleural Bupivacaine for postoperative analgesia following thoracotomy | I jadad 5 | Prospective randomized, blinded study of IPA vs. saline placebo in thoracotomy patients . Small series ( n=19) but no subjective or objective benefits as measured by pain scale, length of stay or IV narcotic sparing. |
| Richardso n J | 1995 | A Prospective Randomized Comparison of Interpleural and Paravertebral Analgesia in thoracic surgery. British Journal of Anaesthesia 75: 405-408 | I Jadad 4 | A prospective, randomized, blinded study of 45 patients undergoing thoracotomy divided to receive intrapleural or paravertebral (extrapleural) bupivicaine. Both groups had equivalent breakthrough PCA requirements. The paravertebral group had improved PFTs, , decreased respiratory morbidity and LOS, all to the pont of statistical significance. The intrapleural group alone had a significant rate of confusion due to bupivicaine toxcity. Authors conclude that parvertebral anesthetic produced better preservation of lung function and fewer complications. |
| Hansdottir V | 1996 | The Analgesic Efficacy and Adverse effects of Continuous Epidural Sufentanil and Bupivacaine Infusion After Thoracotomy. Anesth Analg83:394-400 | I Jadad 3 | Double-blind randomized trial comparing lumbar epidural narcotic (sufentanil) to thoracic epidural narcotic to a combined thoracic narcotic and anestheteic (bupivicaine). Outcomes were pain scores and respiratory parameters. The combined treatment provided superior analgesia at rest and during function despite lower infusion rates and less need for rescue narcotics. Minor complication rates did not vary. Sample size was small. |
| Wiebalck A | 1997 | The Effects of Adding Sufentanil to Bupivacaine for Postoperative Patient-controlled Epidural Analgesia. Anesth Analg 85:124-9 | I Jadad 5 | Prospective randomized, double-blinded study of the addition of Epidural Analgesic ( sufentanil) to epidural anesthetic treatment (bupivicaine). The addition of the narcotic allowed lower doses of anesthetic. Yet the groups did not differ in the incidence of respiratory depression or motor block. The test group reported lower pain scores at rest and at activity for days 13. The writers concluded that addition of small amounts of epidural narcotics effectively augments analgesia though decreased complicatio rate not detected. Adequate study size of 100 patients. |
| Kaiser AM | 1998 | Prospective, Randomized Comparison of Extrapleural Versus Epidural Analgesia for Postthoracotomy Pain | I Jadad 3 | Both methods were equally effective and safe in relieving pain and promoting return of pulmonary function. There were minor statistically significant differences of deccreased narcotic use in favor of extrapleural. Authors conclude and the more widespread applicability make extrapleural analgesia a good alternative method when epidural is contraindicated. Small series of 15 patients in each limb. |
| Della Rocca G | 2003 | Post-thoracotomy analgesia: epidural vs. IV morphine continuous infusion Minerva Anestesiol. 68(9):681-93 | I Jadad 3 | Large PRCT, (n=563) non-blinded, of continuos EDA vs IV . EDA patients had significantly better subjective pain control while IV patients had more complications, nausea and vomiting. Hospital LOS significantly decreased in EDA group ( 9 vs. 11 days +/-4). Authors conlude EDA is superior for pain control, LOS and complications. Well-designed, large Class I study; one of few to show improvement in objective outcome measure. |
| Flisberg P | 2003 | Pain Relief and Safety after Major Surgery: Prospective Study of Epidural and IV Analgesia in 2696 Patients. Acta Anaesthesiol Scand 47(4):457-65 | II | Prospective non-random cohort study of 2670 epidural and 1026 IV patients having major abdominal or thoracic surgery. Orthostasis, LE weakness and pruritis more common with EDA. Respiratory depression, sedation, hallucination and confusion more common with IVA. Authors conclude that EDA patients have less pain while IV patients have more narcotic side-effects. EDA is safe for use on the ward with minimal adverse effects. Large study with excellent statistics. Objective measures such as PFTS not employed and actual outcomes not assessed. Meaningful as far as complication rates but efficacy application to thoracic trauma not clear. |
| Nursing issues with regard to pain management in blunt chest trauma (6) | ||||
| Soliman IE | 1985 | Successful management of an elderly patient with multiple trauma. J Trauma. 25:806-07 | na | Case report of an elderly woman with BCT and lower extremity fractures managed with concurrent thoracic and lumbar EA |
| Ready LB | 1991 | Postoperative epidural morphine is safe on surgical wards. Anesthesiology.75:452-56 | III | Large series (N=1106) of EA catheters managed on the surgical ward, outside of the ICU. Mild complication rates (pruritis 24%, nausea 29%), respiratory depression (0.2%) and no deaths. Overall, 95% of the patients had no complications in their catheter management. This study demonstrates that with proper training of nursing staff, careful dosaging and monitoring, epidural morphine is safe for use on surgical floors. |
| Slack JF | 1991 | Efficacy of epidural analgesia for pain management of critically ill patients and the implications for nursing care. AACN. 2:729-40 | I Jadad 2 | A very small (n=15) PRCT demonstrates efficacy of EA in an elective surgery/ICU population, and includes a good review of mechanisms of pain and of EA itself. Patients randomized to epidural narcotic, epidural anesthetic, epidural combination or IM narcotic. Patients with epidural morphine or combination had less subjective pain and better recovery of function at day 3. Side effects were minimal. Samples in each group were extremely small (n=3-4) and no statistical analysis provided. The value of this as an effficacy study is questionable at best. However, study does serve as further evidence that epidurals are safe if managed by trained nursing and appropriately monitored. |
| Kaiser KS | 1992 | Assessment and management of pain in the critically ill trauma patient. Crit Care Nurs Q. 15:14-34 | III | A well-researched, well-written review of major issues in the management of pain in the trauma patient. Includes section on EA. |
| Stanik-Hutt JA | 1993 | Strategies for pain management in traumatic thoracic injuries. Crit Care Nursing Clin No America. 5:713-22 | III | Literature review of pain management strategies specifically for the BCT patient. |
| Stevens DS | 1994 | Management of pain in mechanically ventilated patients. Crit Care Clin. 10:767-78 | III | Review article on variety of pain management methods, including patient-controlled EA. |
| Anesthesia concerns and complications from blunt chest trauma and its treatment (20) | ||||
| Ottesen S | 1978 | Cardiovascular effects of epidural analgesia: An experimental study in open-chest sheep. Acta Anaesth Scan. 69:1-16 | TA** | A thorough physiologic description of the sympatholytic and other cardiovascular effects of epidural anesthetic agents in the laboratory setting. |
| Mayumi T | 1983 | Plasma concentrations of lidocaine associated with cervical, thoracic and lumbar epidural anesthesia. Anesth Analg. 62:578-80 | II | Prospective observational study of systemic absorption of local anesthetic (lidocaine) when used in cervical, thoracic, and epidural anesthesia. The rate and extent of serum levels were virtually identical at all three levels and no drug side effects occurred. |
| Nordberg G | 1987 | Pharmacokinetics of different epidural site of morphine administration. Eur J Clin Pharmacol. 33:499-504 | TA** | Review of morphine pharmacokinetics during EA. |
| Gomez MN | 1987 | Intrapleural Bupivacaine for Intraoperative Analgesia – A Dangerous Technique? Anesth Analg 67: S1-S266 | II / I Jadad 4 | (In a placebo-controlled, randomized, double-blinded design, this study assessed intro-operative sparing of inhalational agents by intrapleural bupivicaine) In an observational manner (class II), the study reviewed the complication rate of inrapleural devices. It identified 11/18 incorrectly positioned catheters: 3 coiled in chest wall; 1 tension pneumothorax; 7 catheters placed in lung tissue. The study concluded that there was a high complication rate for intrapleural catheters but postulated that this was experiential and operator-dependent. Relevance to post-thoracic trauma pain management unclear. |
| Ward AJ | 1989 | Delayed diagnosis of traumatic rupture of the spleen – a warning of the use of thoracic epidural in chest trauma. Injury. 20:178-9 | na | Delayed splenic rupture case where the authors speculate that based on blockade of afferent Type C unmyelinated nerve fibers secondary to EA, peritoneal irritation went unnoticed. |
| Hopf HB | 1990 | High thoracic segmental epidural anesthesia diminishes sympathetic outflow to the legs, despite restriction of sensory blockade to the upper thorax. Anesthesiology. 73:882-89 | I Jadad 5 | Prospective, randomized, double-blind study to assess whether high thoracic epidural anesthesia may yield a more caudal sympathetic blockade than is indicated by the sensory level. Authors concluded that a widespread distal temperature change may indicate an unrecognized distal sympathetic block. A number of technical assumptions are made in this study which have been questioned in the anesthesiology community. Also, a high dose bolus was used and this may have little relevance for the continuous epidurals used in trauma patients |
| Ready LB | 1991 | Postoperative epidural morphine is safe on surgical wards. Anesthesiology. 75:452-56 (duplicate = see “Nursing” section) | III | Large multi-center retrospective survey (N=1106) of EA catheters managed outside the ICU, on the surgical ward. Mild complication rates: pruritis (24%), nausea 29%), respiratory depression (0.2%) and no deaths. Overall, 95% of the patients had no complications in their catheter management. This study, also listing under “nursing” section serves here as a large-scale retrospective review of epidural complication rates. Limitation of the study in consideration as Class II evidence is the multi-center structure with possible differences in reporting standards. |
| Scherer R | 1993 | Complications related to thoracic epidural analgesia: a prospective study in 10771 surgical patients Acta Anaesthesiol Scand 37: 370-374 | II | Large prospective (observational) series accurately identifying complication rates with epidural catheters: 1.2% dural puncture; 1.7% unsuccessful placement; .6% radiculopathy; .1% respiratory depression. |
| Sugimori K | 1993 | Thoracic epidural anesthesia causes rib cage distortion in anesthetized, spontaneously breathing dogs. Anesth Analg. 77:494-500 | Laboratory investigation (7 dogs) measuring electromyographic activity in parasternal muscles with EA demonstrates impaired contraction and diminished ventilation when using EA. | |
| Liem LK | 1994 | Thoracic epidural abscess. J Spinal Disord. 7:449-54 | III | In a retrospective, descriptive 10 year review of thoracic epidural abscess, 21 cases were identified. One of these (5%) was secondary to EA. Management of the complication is discussed. No denominator provided to assess incidence rate. |
| Lonnqvist PA | 1995 | Paravertebral Blockade: Failure Rate and Complications. Anaesthesia. 50:813-815 | II | Prospective observational study of the comoplications of paravertebral (extrapleural) block: 10% failure rate (higher than epidural) 4.6% hypotension; 3.8% vascular puncture; 1.1% pleural puncture; .5% pneumothorax. Authors identified higher failure rates than with epidurals but similar complication rates. They recommended this as an appropriate technique for coagulopathic or anticoagulated patient, particularly if chest tube already in place. |
| Warner DO | 1996 | Human chest wall function during epidural anesthesia. Anesthesiology. 85:761-73 | TA** | Studying the effects of EA on respiratory muscle activity in 6 uninjured persons using electromyography, authors show that FRC is increased primarily by the EA effect on caudal displacement of the diaphragm at end expiration. |
| Giebler RM | 1997 | Incidence of neurologic complications related to thoracic epidural catheterization. Anesthesiology. 86:55-63 | II | 4,185 patients studied, including 2,059 prospectively on the incidence of thoracic EA related complications. In this excellent review, the authors found an overall complication rate of 3.1% and a predicted risk for permanent neurologic complication of 0.07%. |
| Kurek SJ | 1997 | Complications of Epidural Infusions for Analgesia in Postoperative and Trauma Patients. American Surgeon 63: 543-546 | III | A retrospective review comparing continuous epidural analgesia (sufentanil and bupivicaine) to bolus injection (duramorph) in trauma and abdominal surgery patient. There was a significantly higher complication rate with continuous infusion (motor block, nausea/vomiting and catheter leak) vs the bolus group (nausea/vomiting, mental status change and local erythema). Motor block, catheter leak and urinary retention were essentially confined to the continuous infusion group. Authors conclude that though effective, epidural catheters are not without risk. Continuous infusion has a higher complication rate which must be weighed against its reported increased effectiveness. |
| Niimi Y | 1997 | Echocardiographic evaluation of global left ventricular function during high thoracic epidural anesthesia. J Clin Anesth. 9:118-124 | II | Observational study in healthy elective surgery patients of the effects of high thoracic epidural anesthetic (THE) versus lower thoracic epidural (LTE) on hemodynamics. Systemic BP, CO and heart rate had small but significant decreases with HTE but not LTE. Alterations were produced by changes in heart rate since ejection and disastolic filling as assessed by echo were unchanged. Applicability to sicker trauma patients is unclear. |
| Liu M | 1998 | Delayed Horner’s syndrome as a complication of continuous thoracic epidural analgesia. J Cardiothoracic Vasc Anesth. 12:195-196 | III | Case report of delayed Horner’s Syndrome, unilateral sympathetic block of the face, in continuous high thoracic epidural anesthesia.. Describes an uncommon complication of epidural anesthesia which might mimic neurologic complications of trauma and should be considered with new onset ptosis. |
| Niemi G | 1998 | Adrenaline markedly improves thoracic epidural analgesia produced by a low-dose infusion of bupivacaine, fentanyl and adrenaline after major surgery.Acta Anaesth Scand. 42:897-909 | I Jadad 4 | Prospective, double-blind, randomized, cross-over study of the addition of epinephrine to fentanyl / bupivicaine epidural.. Addition of epinephrine yielded better sensory block, less pain with coughing, similar side effected and lower serum fentanyl levels.. This is a highly relevant, strong study supporting the use of epinephrine in fentanyl /bupivicaine epidurals. |
| Wong D | 1998 | Spinal epidural abscess. NZ Med J. 111:345-47 | N/A | An anecdotal report indicating that spinal epidural absecess has been reported as a complication of epidural analgesia. |
| Kapral S | 1999 | The effects of thoracic epidural anesthesia on intraoperative visceral perfusion and metabolism. Anesth Analg. 88:402-6 | II | An prospective placebo-controlled observational study in 30 patients receiving thoracici epidural anesthesia (TEA) with bupivicaine for abdominal surgery. TEA prevented a decrease in gastric pHi and increase in PiCO2 during surgery. The authors conclude that TEA may be useful for pain control in settings of surgical stress. |
| Dernedde M | 2003 | Continuous Epidural Infusion of large concentration / small volume versus small concentration / large volume of levobupivicaine for pospterative analgesia. Anesth Analg. 96(3):796-801 | I Jadad 3 | PRCT of two concentration combinations for epidural bupivicaine analgesia administered at the same total dose. The large concentration / small volume dosing provided equivalent pain score assessment with less motor blockade and fewer hemodynamic consequences. Well designed study which is adequately powered. Relevant to the technique of epidural administration. |