Emergency Department Thoracotomy in Children: A PTS, WTA, and EAST Systematic Review and Practice Management Guideline
Published 2022
Citation: J Trauma, Publish Ahead of Print
Authors
Leigh Selesner MD, Brian Yorkgitis DO, Matthew Martin MD, Grace Ng MD, Kaushik Mukherjee MD MSCI, Romeo Ignacio MD MSc, Jennifer Freeman MD, Lye-Yeng Wong MD, Samantha Durbin MD, Marie Crandall MD MPH, Shannon W Longshore MD, Claire Gerall MD, Katherine T. Flynn-O’Brien MD, Mubeen Jafri MD
Background
Trauma is the leading cause of morbidity and mortality in the United States pediatric population.[1] The creation of trauma centers and improvement in pre-hospital care has increased the number of injured children arriving in the emergency department (ED), who previously may have succumbed to their injury in the field.[2] The emergency department thoracotomy (EDT) is a controversial procedure performed in select patients presenting with refractory shock or circulatory arrest after injury. The practitioner must make an immediate decision, balancing patient survival with many risks, including performing a possibly futile procedure, resuscitating patients with anoxic brain injury, and exposing providers to unnecessary risks. A 2018 prospective study of 1360 surgeons performing 305 EDTs found 7.6% of EDTs were associated with blood or bodily fluid, and 1.6% of participants were exposed.3
Evidence-based guidelines have been created for adults without similar recommendations for children.[4],[5] Historically, the adult guidelines have been followed in children,[6] however, may be inappropriate. This work aims to provide evidence-based guidelines for physicians faced with a critically injured child to help decide whether to proceed with EDT using Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology.[7]
Objective:
Twelve adult and pediatric surgeons with pediatric trauma expertise representing PTS, EAST, and WTA formed a committee to determine if EDT, as opposed to resuscitation without EDT, improves outcomes in pediatric patients (<19 years old) who present to the ED pulseless after a traumatic injury. Our population, intervention, comparator, and outcome (PICO) questions are based on the 2015 EAST practice management guideline (PMG)[5] and are as follows:
Population:
- Pediatric patients presenting pulseless to the ED with signs of life (SOL) after penetrating thoracic injury
- Pediatric patients presenting pulseless to the ED without SOL after penetrating thoracic injury
- Pediatric patients presenting pulseless to the ED with SOL after penetrating abdominopelvic injury
- Pediatric patients presenting pulseless to the ED without SOL after penetrating abdominopelvic injury
- Pediatric patients presenting pulseless to the ED with SOL after blunt injury
- Pediatric patients presenting pulseless to the ED without SOL after blunt injury
Intervention: EDT
Comparator: Resuscitation without EDT
Outcomes:
- Hospital survival (HS)
- Neurologically intact hospital survival (NIS)
Signs of Life Definition:
As defined by the 2001 American College of Surgeons Committee on Trauma,[8] SOL were considered present with any of the following: cardiac electrical activity, respiratory effort, pupillary response, palpable pulses, measurable blood pressure, or extremity movement.
Methods
Inclusion Criteria
Study Types:
We included prospective observational studies, retrospective studies, cohort studies, and case series. No randomized control trials were found. Systematic reviews, case reports, letters, and articles without an English translation were excluded. Two retrospective studies using the National Trauma Database (NTDB) were identified.[9],[10] The NTDB has recognized limitations, including the retrospective design, lack of granular data (i.e., time to intervention), and significant proportions of missing variables (i.e., GCS at the scene). The NTDB also uses ICD-9 codes to retrieve data subject to coding errors and variations.[11] Flynn-O’Brien et al.’s NTDB-based study included children who underwent EDT from 2007 to 2012, which overlapped with other included studies; therefore, it was excluded.[10] However, Prieto et al.’s series was included as the children underwent EDT from 2013 to 2016, a period without overlap.
There was debate among the committee regarding challenges with the NTDB, including the impact of possibly flawed data on the final recommendations, which account for most survivors. Those who supported inclusion conceded its limitations but recognized the NTDB study uses combined data from individual trauma center registries, which are also used for other included studies. Moreover, data from the remaining literature could be subject to the same limitations (i.e., lack of granular data, input errors, etc.). After deliberation, 11/12 committee members voted to include the NTDB study.[12]
Participant Types:
All pediatric patients <19 years old who underwent EDT regardless of sex, ethnicity, or comorbidities were included.
Intervention Types:
Based on the pre-establish methodology described in Seamon et al. in 2015,[5] the probability of hospital survival without EDT was estimated. CI: confidence interval; RR: risk ratio.
We included studies where EDT was performed, injury mechanism and SOL were defined, and outcomes of interest were measured. Studies involving prehospital or operating room thoracotomy were excluded. No HS or NIS data for similar groups who did not undergo EDT were available in the literature. For the EAST 2015 PMG, the subcommittee estimated these values. Individual members were polled to predict patient HS and NIS without EDT, but standard resuscitation and emergent transport to the operating room as needed. Outliers were excluded, and mean survival probability was calculated.[5] Our working group agreed to use these estimations for our comparator groups understanding the results would be heavily based on expert opinion (Table 2).
Outcome Measure Types:
Per GRADE, outcomes were selected and voted on independently by each author in order of importance (1 to 9, with 7 to 9 representing critical outcomes). Outcomes considered were HS, NIS, exposure to blood-borne pathogens, and costs. Only HS and NIS were determined to be “critical” for decision-making. NIS was defined as having full neurological function on discharge.
Review Methods
Electronic Search:
The protocol was registered in PROSPERO (CRD42022344883). An information specialist assisted with a search of the National Institute of Health MEDLINE database using Ovid with citations published between 1946 and September 2, 2021 (Appendix 1, http://links.lww.com/TA/C921). The terms searched included “children” and the following: “thoracotomy,” “emergency medical services,” “emergency treatment,” “emergencies,” “emergency room,” “emergency department,” “emergency service,” and “emergency ward.” We used the “related articles” function and manually searched bibliographies of recent reviews and articles.
Study Selection and Data Extraction:
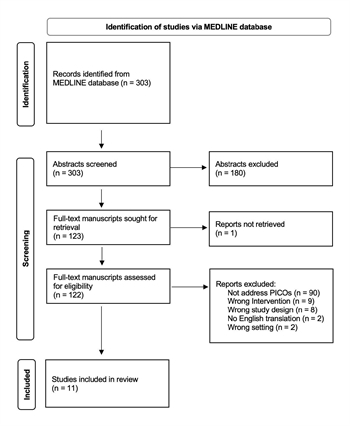
Figure 1: Preferring Reporting Items for Systematic Reviews and Meta-analyses Diagram of Included Studies
Covidence Systematic Review Software (Veritas Health Innovation, Melbourne, Australia) was used for study selection and data extraction. Titles and abstracts from the electronic search were screened for relevance to the PICO questions. Those adherent to the inclusion criteria underwent a full-text review to determine final appropriateness (Figure 1). Two committee members independently performed all abstract screening, manuscript review, and data extraction, with conflicts resolved by a third.
Measures of Treatment Effect:
Data on HS and NIS after EDT from included studies were collected. Event rates were calculated and compared to the expected survival probabilities without EDT for each PICO question by calculating relative risk (RR) and confidence intervals (CI). Meta-analysis and heterogeneity analysis could not be calculated without a comparison group in each individual study.
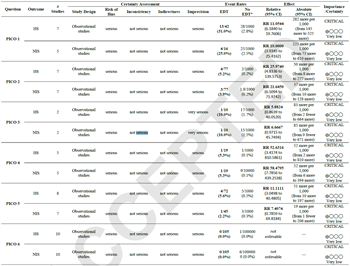
Assessment of Methodological Quality:
In accordance with GRADE,[7] the evidence quality was assessed by: risk of bias, inconsistency, indirectness, imprecision, and publication bias and categorized as either of high, moderate, low, or very low quality. Evidence profile tables were generated using GRADEpro Guideline Development Tool (McMaster University and Evidence Prime Inc., Hamilton, ON, Canada). The survival probability estimation for patients without EDT is not part of standard GRADE methodology. All committee members independently voted on the proposed recommendations. The strength of recommendations was determined by considering the evidence quality, risk-versus-benefit profile, resource utilization, and patient values and preferences. The strength of the recommendation was classified as either “strong” or “weak,” prefaced by “strongly recommend” or “conditionally recommend,” respectively, and reflects the degree of confidence a provider can have for the recommendation to promote benefit over harm.[13] The committee unanimously voted for the following voting thresholds: for a recommendation to be “strong,” at least 70% of the group must vote for a strong recommendation. A recommendation either against or for EDT was based on majority vote. The committee approved the final recommendations. Differences in opinion were resolved via conference call and email. AGREE guideline was used to ensure proper reporting of methods, results, and discussion (Supplemental Digital Content, http://links.lww.com/TA/C922).
Results
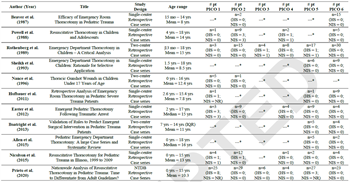
Author, year of publication, title, study design, age range, and mean/median age of included patients is included. The last six columns show the number of patients in each study that address each PICO as well as the number of patients with hospital survival (HS) and neurologically intact hospital survival (NIS). *No patients within the paper address the PICO. Copyright © 2023 Wolters Kluwer Health, Inc. All rights reserved.
The literature search yielded 303 studies, of which 180 were removed after title and abstract review. Of the 123 full-text manuscripts reviewed, 111 were excluded: 90 studies not addressing our PICO questions (i.e., adult population, outcomes not broken down by SOL), 11 studies with the wrong intervention (i.e., operating room thoracotomy, prehospital thoracotomy), 8 systematic reviews, 2 non-English articles and 1 full-text unable to be retrieved. Ultimately, 11 retrospective case series were included (Figure 1).[9],[14-23] Seven were single-center,[14],[15],[17],[18],[20-22] 3 were two-center,[16],[19],[23] and 1 used the NTDB (Table 1).[9] The included studies provided 319 children who underwent EDT, of which 142 (44.5%) sustained penetrating and 177 (55.5%) sustained blunt injury. Overall survival in the penetrating group was 13.4% (19/142) and 2.3% (4/177) in the blunt group. Across all included children who underwent EDT, 7.2% (23/319) survived.
PICO 1
In pediatric patients presenting pulseless to the ED with SOL after penetrating thoracic injury, should EDT be performed, versus resuscitation without EDT, to improve HS and NIS?
Qualitative Synthesis:
Seven retrospective case series (n=42) evaluated HS, of which 5 (n=16) discussed NIS.[9],[17-21],[23] Three studies reported no survivors (n=9), and all sustained thoracic gunshot wounds (GSWs).[19],[21],[23] Conversely, two series reported 100% HS.[17],[24] Easter et al. described three 17-year-old patients between 1995 and 2009 who sustained cardiac stab wounds and survived intact.[17] Hofbauer et al. reported the survival of 1 child (<16 years) from 1992 to 2008 with an isolated chest stab wound but omitted NIS data.[18] Of the included studies, Prieto et al. incorporated the most significant population using the NTDB between 2013 and 2016. Thirty-two percent (8/25) survived (all <16 years), but NIS was not reported.[9]
Quantitative Synthesis:
Pooled data from included studies showed 31% survival (13/42). Based on previously described methods,[5] the estimated HS following resuscitation without EDT is 2.8% (RR=11.1; 95% CI=6.18-19.8; p<0.0001). NIS from pooled data was 25% (4/16) compared to the estimated 2.5% without EDT (RR=10.0; 95% CI=3.93-25.4; p<0.0001) (Table 2).[17],[19-21],[23]
Recommendation:
The committee conditionally recommends EDT for a pediatric patient presenting pulseless to the ED following a penetrating thoracic injury with SOL. All authors voted for a conditional or strong recommendation in support. Our analysis demonstrated improved outcomes with EDT, but the recommendation was made conditional given the poor evidence quality and paucity of patients. The committee also considered that available data in adult populations support EDT in this scenario.[5]
PICO 2
In pediatric patients presenting pulseless to the ED without SOL after penetrating thoracic injury, should EDT be performed, versus resuscitation without EDT, to improve HS and NIS?
Qualitative Synthesis:
Seven retrospective studies (n=77) provided HS and NIS data,[9],[15],[17],[19-21],[23] which includes children who, in addition to their thoracic injury, may also have an extrathoracic injury (n=5).[17],[21] During EDT, aortic control is often performed to limit exsanguination from distal anatomic structures. Thus, we include extrathoracic injuries for which aortic control may reduce exsanguination.
Most articles found 0% survival,[9],[15],[17],[19],[23] of which, the largest included 29 patients (all <16 years).[9] Conversely, Powell et al. (n=9) found 3 children between 1981 and 1986 with NIS, of which 2 sustained chest stab wounds and 1 had a GSW to the chest and thigh. Importantly, all survivors were 17 or 18 years old. Nicolson et al. found 1 survivor (<16 years) between 1999 and 2009 without NIS (n=12) after penetrating cardiac injury.
Of note, time duration without SOL was not consistently reported. Most studies only indicated if SOL were present on ED arrival,[12],[15],[23],[25] including the NTDB study. Easter et al., however, who found 0 survivors (n=9), described transport time by EMS for all patients as <30 minutes.[17] Powell et al. detailed whether SOL were present in the field and the ED. Of those who survived, 1 had field SOL but was unknown for the other 2 survivors. Two patients with field SOL died.[21] Lastly, for the patient who survived without NIS, transport time was 3 minutes. For the rest of that series, known average transport time was 10.3 minutes (range 3-21 minutes).[20]
Quantitative Synthesis:
Pooled data demonstrated that 5.2% (4/77) survived, compared to the estimated probability without EDT of 0.2%5 (RR=26.0, CI=4.83-139.6; p=0.0001). Of 77 children, 3 survived intact, conferring an event rate of 3.9% compared to the estimated NIS without EDT of 1.8%.5 (RR=21.6; CI=6.51-72.0; p<0.0001) (Table 2).
Recommendation:
In a child presenting pulseless to the ED following penetrating thoracic injury without SOL, we conditionally recommend against EDT with 8 votes from the authors. However, 4 authors conditionally recommended EDT. Only 4 patients survived in the literature: 1 without NIS (<16 years) and 3 who were 17 and 18. Children >15 may have hemodynamic differences from younger children that should be considered.[26] The committee also acknowledged that time duration without SOL is crucial while decision-making, but more data is needed to specify an acceptable duration. Given the available data regarding lack of SOL on ED arrival in this population, and the work group’s clinical expertise, a conditional recommendation against EDT was made to allow for the discretion of the treating provider, who has intimate knowledge of the patient's physiology and time of lost SOL.
PICO 3
In pediatric patients presenting pulseless to the ED with SOL after penetrating abdominopelvic injury, should EDT be performed, versus resuscitation without EDT, to improve HS and NIS?
Qualitative Synthesis:
Two studies (n=10) addressed PICO 3.[9],[23] Rothenberg et al. included 4 patients (<19 years) between 1977 and 1988 with penetrating abdominal injury. One survived and remained neurologically intact.[23] The NTDB review from 2013 to 2016, however, found 0 “noncranial” extrathoracic survivors (<16 years; n=6).[9]
Quantitative Synthesis:
The estimated HS and NIS for those who do not undergo EDT are 1.7% and 1.5%, respectively.[5] Pooled data revealed 10% HS and NIS in patients who underwent EDT (1/10) (HS RR=5.88; CI=0.86-40.1; p=0.07); (NIS RR=6.67; CI=0.97-45.7; p=0.05) (Table 2).
Recommendation:
We conditionally recommend EDT for a pediatric patient presenting pulseless to the ED following a penetrating abdominopelvic injury with SOL. Nine authors voted in support, while 2 voted for a conditional recommendation against EDT. Comprehensive literature review revealed insufficient data. The committee voted for a conditional recommendation based on support from the adult literature but recognized that all extrathoracic injury sites may not confer the same survival rates and need to be considered.[5]
PICO 4
In pediatric patients presenting pulseless to the ED without SOL after penetrating abdominopelvic injury, should EDT be performed, versus resuscitation without EDT, to improve HS and NIS?
Qualitative Synthesis:
Five studies (n=19) reported HS and NIS data; most found 0% survival following EDT.[9],[17],[20],[21],[23] The site of injury was defined as abdominal (n=9)[23],[27] or “noncranial extrathoracic” (n=4).[12] Patients who sustained concurrent thoracic (n=3) and unspecified aortic injury were also included (n=2).[17],[21] Powell et al. described one 18-year-old patient (n=2) with NIS after GSW to the thigh and chest.[21]
Quantitative Synthesis:
The estimated HS and NIS without EDT are 0.1% and 0.09%, respectively.5 Analysis of pooled EDT data demonstrated both HS and NIS as 5.3% (1/19) (HS RR=52.6; CI=3.42-810.6; p=0.005) (NIS RR=58.5; CI=7.79-439.3; p=0.0001) (Table 2).
Recommendation:
In a pediatric patient presenting pulseless to the ED following a penetrating abdominopelvic injury without SOL, we conditionally recommend against EDT. Ten authors voted against EDT, while one voted for a conditional recommendation in support. If the one survivor (thigh/chest injury) were removed from analysis, the pooled survival would be 0. The small number of patients resulted in a skewed analysis showing a survival benefit. Based on the committee’s expertise, a conditional recommendation was made to allow for discretion by the treating provider, who knows the patient’s physiology and time without SOL and can use adjuncts such as ultrasound to assist in the evaluation and management.[6]
PICO 5
In pediatric patients presenting pulseless to the ED with SOL after blunt injury, should EDT be performed, versus resuscitation without EDT, to improve HS and NIS?
Qualitative Synthesis:
Eight studies (n=72) addressed HS[9],[14],[16-18],[20],[22],[23] and 7 (n=45) evaluated NIS.[14],[16-18],[20],[22],[23] There were no survivors in 6 studies.[14],[16-18],[20],[22] The NTDB review, between 2013 and 2016, reported 3 survivors (<16 years; n=27), but NIS data were omitted.[9]: Rothenberg et al. (n=17) found 1 with thoracic injury and NIS between 1977 and 1988.[23] Reporting of blunt injury location was inconsistent, and several articles did not provide a definition, including the NTDB study.[12],[16],[22] Of those which did, sites included chest, neck, abdomen, brain, aorta, “multiple” or unknown.[14],[17],[23],[24],[27]
Quantitative Synthesis:
The estimated HS without EDT is 0.5%, and NIS is 0.3%.[5] Pooled data evaluating HS demonstrated an event rate of 5.6% (4/17) (RR=11.1; CI=3.05-40.5; p=0.0003).[9],[14],[16-18],[20],[22],[23] Pooled data revealed a NIS of 2.2% (1/45) (RR=7.41; CI=0.76-69.8; p=0.08) (Table 2).
Recommendation:
In a pediatric patient presenting pulseless to the ED following a blunt injury with SOL, we conditionally recommend EDT, following the performance of emergency adjuncts, including ultrasound and thoracostomies, to determine injury location and/or reversible causes of shock, if able. Seven committee members voted in support; however, four votes were made for a conditional recommendation against EDT. As traumatic brain injury (TBI) is a leading cause of death in pediatric trauma patients, discussion regarding concomitant TBI raised concerns leading to some authors recommending against EDT. The authors considered that patients might not want to undergo EDT, given the possibility of severe TBI or poor neurological outcomes. Given the available data and the working group’s expertise, a conditional recommendation was made to allow for treating provider discretion, who knows the totality of the patient’s injury burden.
PICO 6
In pediatric patients presenting pulseless to the ED without SOL after blunt injury, should EDT be performed versus resuscitation without EDT to improve HS and NIS?
Qualitative Synthesis:
Literature review identified 10 studies (n=105) with no survivors.[9],[14-18],[20-23] Reporting of injury location was inconsistent.
Quantitative Synthesis:
HS and NIS are estimated as 0.001% and 0.0006%, respectively.[5] In our literature review, we found no survivors conferring an event rate of 0% for both outcomes of interest. RR and CI could not be calculated (Table 2).
Recommendation:
In a pediatric patient presenting pulseless to ED following a blunt injury without SOL, we strongly recommend against EDT. The committee unanimously voted strongly against EDT.
Despite low-quality evidence and a small population, the committee believed that most patients would not favor EDT in this scenario due to dismal survival rates and the likelihood of poor neurological outcomes, supported by our review and the adult literature.[5]
Grading the Evidence
By employing GRADE, the overall quality of evidence for all PICO questions was very low, determined by the serious risk of bias for the research design and the serious risk of imprecision due to small population sizes. PICO 3 was determined to have a very serious risk of imprecision for an extremely low sample size (n=10) (Table 2).
Discussion
Future directions:
This review revealed a paucity of data regarding the utility of EDT in the pediatric trauma population based on physiology. The number of included patients and data quality is low compared with similar adult studies. Despite the known physiological differences between adults and children, particularly the child’s response to hypotension[28] the committee had to consider adult outcomes when making recommendations. The committee also relied on expertise and experience to guide voting. This review proves that further focused studies are required to create evidence-based guidelines grounded on high-quality evidence.
There may also be significant differences in outcomes in young children versus adolescents that were not evaluated due to the lack of data for EDT outcomes based on both mechanism and physiology but should be considered. Dissimilar to adults, children hemodynamically compensate for acute blood loss until late in the clinical course. Therefore, decompensation reflects a greater degree of hemorrhage and is consequently less salvageable.29 A prospective observational study by Moore et al. included 179 pediatric EDT patients and compared survival between children (<=15 years) and adolescents (16-18 years). A higher survival rate in adolescents than pediatric patients (5% versus 0%, p=0.036) was found.[26]
This survival discrepancy may also be attributed to mechanism differences: pediatric patients sustained more blunt injury than adolescents in this study (72% versus 32 %, p<0.001).[26] Data from both adult and pediatric populations show improved mortality following penetrating over blunt injuries.[5],[30] Our survival data supports this: 13.4% of penetrating victims versus 2.3% of those bluntly injured. In a retrospective case series using the NTDB, Wyrick et al. described 316 children who underwent EDT, and all survivors (n=98) had penetrating injuries. Furthermore, penetrating injury was associated with decreased risk of death compared to blunt (OR=0.34, p=0.009).[30]
Limitations:
This study has several limitations, mainly derived from the low-quality evidence and scarcity of data. Our results rely on the NTDB, estimated probabilities of HS and NIS, and data from children >15 years. In addition, extrathoracic injury site, blunt injury location, and time without SOL were not well defined across the literature. Given the available data, expert opinion guided recommendation development, and there was nonunanimous voting. The committee voted to abide by the majority vote; however, due to the controversies, conditional recommendations were made to allow discretion to the treating provider, who is privy to the totality of injury burden and should employ adjuncts such as ultrasound to assist with decision-making. With expert opinion comes risk for bias, especially given the ethical dilemma surrounding the decision to perform or withhold this life-saving procedure. Lastly, only one database was queried.
Conclusion:
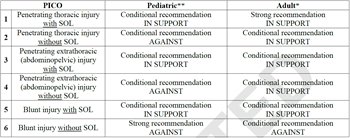
**This committee’s final recommendations. *Recommendations from EAST practice management guideline for emergency department thoracotomy in adult populations.[5]
Based on a comprehensive literature review, we provide evidence-based guidelines using GRADE (Table 3) to provide a framework for the physician facing a child in extremis following a traumatic injury based on mechanism and physiology. We found a lack of high-quality evidence addressing our PICOs, therefore, evidence from the adult literature, expert opinion, and patient/provider preference recognition guided our recommendations. These guidelines are intended to inform decision-making but not replace clinical judgment.
References
- Sathya C, Alali AS, Wales PW, et al. Mortality Among Injured Children Treated at Different Trauma Center Types. JAMA Surg. 2015;150(9):874-81.
- Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma-a review. Injury. 2006;37(1):1-19.
- Nunn A, Prakash P, Inaba K, et al. Occupational exposure during emergency department thoracotomy: A prospective, multi-institution study. J Trauma Acute Care Surg. 2018;85(1):78-84.
- Beall AC, Diethrich EB, Cooley DA, DeBakey ME. Surgical management of penetrating cardiovascular trauma. South Med J. 1967;60(7):698-704.
- Seamon MJ, Haut ER, Van Arendonk K, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;79(1):159-73.
- Burlew CC, Moore EE, Moore FA, et al. Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg. 2012;73(6):1359-63.
- Kerwin AJ, Haut ER, Burns JB, et al. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S283-7.
- Working Group AHSoO, A.erican College of Surgeons. Committee on Trauma. Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg. 2001;193(3):303-9.
- Prieto JM, Van Gent JM, Calvo RY, et al. Nationwide analysis of resuscitative thoracotomy in pediatric trauma: Time to differentiate from adult guidelines? J Trauma Acute Care Surg. 2020;89(4):686-690.
- Flynn-O'Brien KT, Stewart BT, Fallat ME, et al. Mortality after emergency department thoracotomy for pediatric blunt trauma: Analysis of the National Trauma Data Bank 2007-2012. J Pediatr Surg. 2016;51(1):163-7.
- Flynn-O'Brien KT, Stewart BT, Fallat ME, et al. Mortality after emergency department thoracotomy for pediatric blunt trauma: Analysis of the National Trauma Data Bank 2007-2012. Journal of pediatric surgery. 2016;51(1):163-7.
- Prieto JM, Van Gent JM, Calvo RY, et al. Nationwide analysis of resuscitative thoracotomy in pediatric trauma: Time to differentiate from adult guidelines? The journal of trauma and acute care surgery. 2020;89(4):686-690.
- Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
- Allen CJ, Valle EJ, Thorson CM, et al. Pediatric emergency department thoracotomy: a large case series and systematic review. J Pediatr Surg. 2015;50(1):177-81.
- Beaver BL, Colombani PM, Buck JR, Dudgeon DL, Bohrer SL, Haller JA. Efficacy of emergency room thoracotomy in pediatric trauma. J Pediatr Surg. 1987;22(1):19-23.
- Boatright DH, Byyny RL, Hopkins E, et al. Validation of rules to predict emergent surgical intervention in pediatric trauma patients. J Am Coll Surg. 2013;216(6):1094-102, 1102.e1-6.
- Easter JS, Vinton DT, Haukoos JS. Emergent pediatric thoracotomy following traumatic arrest. Resuscitation. 2012;83(12):1521-4.
- Hofbauer M, Hüpfl M, Figl M, Höchtl-Lee L, Kdolsky R. Retrospective analysis of emergency room thoracotomy in pediatric severe trauma patients. Resuscitation. 2011;82(2):185-9.
- Nance ML, Sing RF, Reilly PM, Templeton JM, Schwab CW. Thoracic gunshot wounds in children under 17 years of age. J Pediatr Surg. 1996;31(7):931-5.
- Nicolson NG, Schwulst S, Esposito TA, Crandall ML. Resuscitative thoracotomy for pediatric trauma in Illinois, 1999 to 2009. Am J Surg. 2015;210(4):720-3.
- Powell RW, Gill EA, Jurkovich GJ, Ramenofsky ML. Resuscitative thoracotomy in children and adolescents. Am Surg. 1988;54(4):188-91.
- Sheikh AA, Culbertson CB. Emergency department thoracotomy in children: rationale for selective application. J Trauma. 1993;34(3):323-8.
- Rothenberg SS, Moore EE, Moore FA, Baxter BT, Moore JB, Cleveland HC. Emergency Department thoracotomy in children--a critical analysis. J Trauma. 1989;29(10):1322-5.
- Hofbauer M, Hupfl M, Figl M, Hochtl-Lee L, Kdolsky R. Retrospective analysis of emergency room thoracotomy in pediatric severe trauma patients. Resuscitation. 2011;82(2):185-9.
- Nance ML, Sing RF, Reilly PM, Templeton JM, Jr., Schwab CW. Thoracic gunshot wounds in children under 17 years of age. Journal of pediatric surgery. 1996;31(7):931-5.
- Moore HB, Moore EE, Bensard DD. Pediatric emergency department thoracotomy: A 40-year review. Journal of pediatric surgery. 2016;51(2):315-8.
- Nicolson NG, Schwulst S, Esposito TA, Crandall ML. Resuscitative thoracotomy for pediatric trauma in Illinois, 1999 to 2009. American journal of surgery. 2015;210(4):720-3.
- Wyrick DL, Dassinger MS, Bozeman AP, Porter A, Maxson RT. Hemodynamic variables predict outcome of emergency thoracotomy in the pediatric trauma population. Journal of pediatric surgery. 2014;49(9):1382-4.
- Kissoon N, Dreyer J, Walia M. Pediatric trauma: differences in pathophysiology, injury patterns and treatment compared with adult trauma. CMAJ. 1990;142(1):27-34.
- Wyrick DL, Dassinger MS, Bozeman AP, Porter A, Maxson RT. Hemodynamic variables predict outcome of emergency thoracotomy in the pediatric trauma population. J Pediatr Surg. 2014;49(9):1382-4.