Fall-Related Injuries in the Elderly, Prevention of
Published 2016
Citation: J Trauma. 81(1):196–206, July 2016
Authors
Crandall, Marie MD, MPH; Duncan, Thomas DO; Mallat, Ali MD; Greene, Wendy MD; Violano, Pina MSPH, RN-BC, CCRN, PhD; Christmas, A. Britton MD; Barraco, Robert MD
Author Information
From the Eastern Association for the Surgery of Trauma Injury Control and Violence Prevention Committee and Practice Management Guidelines Section, Department of Surgery (M.C.), University of Florida Jacksonville, Jacksonville, FL; Department of Surgery (T.D.), Ventura County Medical Center, Ventura, CA, Department of Surgery (A.M.), University of Michigan, Ann Arbor, MI; Department of Surgery (W.G.), Howard University Hospital, Washington, DC; Department of Surgery (P.V.), Yale-New Haven Hospital, New Haven, CT, Department of Surgery (A.B.C.), Carolinas Healthcare Systems, Charlotte, NC; and Department of Surgery (R.B.), Lehigh Valley Health Network, Allentown, PA.
Submitted: November 13, 2015, Revised: January 8, 2016, Accepted: February 8, 2016, Published online: March 7, 2016.
These data were presented at the 27th annual meeting of the Eastern Association for the Surgery of Trauma, Januryar 14–18, 2014, in Naples, Florida.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s website (www.jtrauma.com).
Address for reprints: Marie Crandall, MD, MPH, Department of Surgery, 655 W 8th St, Jacksonville, FL 32209; email: Marie.crandall@jax.ufl.edu.
Introduction
Fall-related injuries among the elderly, defined as individuals aged 65 and older, are both frequent and serious. Prospective studies of community-dwelling elderly have found that more than 30% of the elderly fall at least once per year, and the proportion rises steeply with age.[1][2] Up to 10% of independent older adults who fall will sustain a serious injury,[3] such as a femur fracture, which may reduce mobility, limit social interactions, decrease physical fitness, lower quality of life, and increase risk of early death.[4] In 2013, 2.5 million nonfatal falls among older adults were treated in emergency departments, and more than 734,000 of patients were hospitalized. In addition, approximately 25,500 older adults died from unintentional fall-related injuries in the same year.[5] Costs of care for fall-related injuries in the elderly can also be prohibitive; annual nonfatal and fatal costs in the US totaled $23.3 billion in 2008,[6] while the direct medical costs of falls (adjusted for inflation) were $34 billion in 2013.
Prevention of falls among the elderly is an important goal worldwide. Currently, there is a strong body of literature examining strategies for preventing falls using strategies such as exercise and footwear modification. Several meta-analyses and systematic reviews have identified successful strategies for preventing falls, proven effective in randomized controlled trials (RCTs).[7–9] The most successful prevention methods seem to be progressively challenging exercise training[7–9] and risk screening with environmental modifications. One of the limitations that has been identified in this body of work is the lack of injury outcomes.[10] While preventing falls certainly makes intuitive sense, if successful strategies do not affect the outcome of interest, perhaps better use could be made of limited resources for elderly health and wellness.
The Eastern Association for the Surgery of Trauma Injury Control and Violence Prevention Committee along with the Practice Management Guidelines Section produced a practice management guideline to assess the scientific evidence regarding fall-related injury prevention strategies for the elderly.
Objectives
The objective of this practice management guideline was to assess the scientific evidence regarding falls-related injury prevention strategies among the elderly (age 65 or older).
Methods
We used the validated Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology for this study.[11][12] The GRADE methodology entails creating a predetermined question or set of questions that the literature must answer, in the patient population, intervention, comparators, outcome (PICO) format. The PICO questions were created using a modified Delphi method by the Eastern Association for the Surgery of Trauma Injury Control and Violence Prevention Committee along with the Practice Management Guideline Section.
For this guideline, six topical PICO questions were estimated by the authors as the most salient aspects of injury-related falls prevention.
PICO Questions
P: Age 65 and older
I: Clinical interventions to reduce fall-related injuries
C: Intervention compared with control group
O: Injury due to falls
PICO 1: Should bone mineral–enhancing agents be used to prevent fall-related injuries in the elderly?
PICO 2: Should hip protectors be used to prevent fall-related injuries in the elderly?
PICO 3: Should exercise programs be used to prevent fall-related injuries in the elderly?
PICO 4: Should physical environment modifications be used to prevent fall-related injuries in the elderly?
PICO 5: Should risk factor screening be used to prevent fall-related injuries in the elderly?
PICO 6: Should multiple interventions tailored to the population or individual be used to prevent fall-related injuries in the elderly?
After completing a comprehensive literature search performed by a university-affiliated research librarian, three independent reviewers screened the titles and abstracts, excluding reviews, case reports, articles in which injury was not an outcome measure, and unrelated articles. The resulting studies were used for the guideline.
Inclusion Criteria for this Guideline
Study Types
Studies included RCTs, prospective and retrospective observational studies, case-control studies, and meta-analyses. Case reports and reviews containing no original data or analyses were excluded. No date range was specified so as not to exclude early, salient studies.
Participant Types
We included all studies of falls-related injury prevention for participants aged 65 and older.
Intervention Types
We included all studies of falls-related injury prevention methods related to our PICO questions of interest. For PICO 6, we included studies of multiple simultaneous interventions, such as vitamin D plus strength training, tailored to the individual or to a population.
Outcome Measure Types
We limited the review to studies in which injury was the outcome, not simply falls. Owing to the heterogeneity of injury reports, all injuries including, but not limited to, fractures, contusions, lacerations, and hemorrhage were felt to be essential to evaluating the literature within the GRADE framework.
Data Sources and Search
References were identified by research librarians using the Cochrane Library, the MEDLINE database in the National Library of Medicine, and the National Institutes of Health via Entrez (www..gov) in November 2012 with a simple search in March 2015. The search was designed to identify English-language citations regarding fall-related injury prevention in the elderly. Our search strategy was defined a priori to evaluate only those articles in which injury was the outcome, not falls alone. Supplemental digital content 1 contains the MESH terms used for the initial search (see Supplemental Digital Content 1, http://links.lww.com/TA/A745). The articles were limited to humans, clinical trials, RCTs, practice guidelines, meta-analyses, and reviews. A total of 1,830 studies were initially identified.
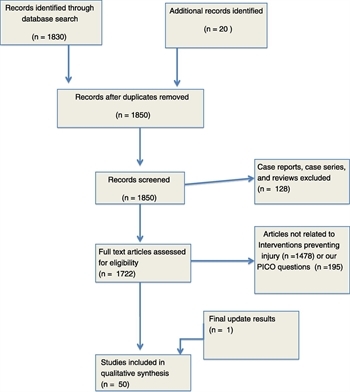
Figure 1: PRISMA diagram.
Study Selection
Case reports and small case series were excluded (n = 128). The authors then reviewed the articles for relevance and excluded articles that did not include injury as a specific outcome of interest (n = 1478). Articles not relevant to our specific PICO interventions (n = 195) were also excluded. Additional articles were added to the literature summary after reading relevant review articles and meta-analyses (n = 20). The final list of 49 articles was reviewed and used to create the recommendations. Each author separately reviewed the evidence to support recommendations using the GRADE methodology in December 2012. Finally, we performed a focused search update in March 2015, during the review and manuscript preparation stages. One additional article was identified and included in the analysis at that time, for a final total of 50 articles reviewed.[13–64] The study selection process is highlighted in the PRISMA flow diagram for Figure 1.
Data Extraction and Management
All studies used for the review were entered into a Microsoft Excel (Redmond, WA) spreadsheet containing information on authors, article title, study methodology, and intervention and outcome measures. A master copy was provided to all reviewers.
Methodological Quality Assessment
We used the validated GRADE methodology for this study.[11][12] Each designated reviewer independently evaluated the data in aggregate with respect to the quality of the evidence to adequately answer each PICO question and quantified the strength of any recommendations. Reviewers are asked to determine effect size, risk of bias, inconsistency, indirectness, precision, and publication bias.
Recommendations are based on the overall quality of the evidence. The GRADE methodology suggests the phrases, “we strongly recommend” for strong evidence, and “we conditionally recommend” for weaker evidence.
Results
We identified 50 articles regarding fall-related injury prevention among the elderly, addressing our six main areas of interest: bone mineral–enhancing agents, hip protectors, exercise programs, physical environment modifications, risk screening strategies, and combined programs. Each evidence profile was evaluated separately as it related to our predetermined PICO question.
PICO 1: Should bone mineral–enhancing agents be used to prevent fall-related injuries in the elderly? (Table 1)
To answer the question of the effectiveness of bone mineral-enhancing agents and fall-related fractures, a meta-analysis was performed by Bischoff-Ferrari et al.[13] in 2005. This review summarized the results of eight RCTs with fractures as a primary outcome;[14–20][26] two of the studies were the same cohort but analyzed with and without an intention-to-treat analysis.[14][26] The authors of the meta-analysis found a statistically significant difference in the treatment arm for all fractures and a trend to decreased hip fractures in the treatment arm. However, the daily dosages ranged from 400 IU cholecalciferol[15][18] to 800 IU;[14][17][19] another study administered 100,000 IU every 4 months.[20] Calcium was either supplemented[14][17][19] or assessed by food intake.[15][16][18][20] The sensitivity analysis suggested that lower doses were not effective.[15][18] Calcium was supplemented in all but one of the higher-dose trials, which makes its inclusion in a regimen unclear.
Subsequent to the meta-analysis, there have been four RCTs published on this topic.[21–24] These trials used a variety of vitamin D administration methods (weekly, monthly, and annually) to achieve a dosing of at least 1,000 IU/day, and again, calcium was either supplemented or assessed. The outcomes of these trials were either not significant[21][24] or favored treatment.[22][23]
PICO 2: Should hip protectors be used to prevent fall-related injuries in the elderly? (Table 2)
Padded hip protectors have been used since the early 1990s to decrease the likelihood that a fall onto a hard surface will cause a fracture. These were extensively studied throughout the 1990s, and in 2004, a Cochrane Database Review of the evidence was published.[27] Although most of the included studies did not show an effect despite having very large sample sizes,[28][29][31][32][34–40] several studies among dependent elderly showed a marked effect.[30][33][41]The conclusions of the authors were that hip protectors are a reasonable consideration for elderly living in nursing homes, with a 19% decrease in hip fracture rates. However, mixed results have been reported in three subsequent RCTs and reviews.[40–42]
PICO 3: Should exercise programs be used to prevent fall-related injuries in the elderly? (Table 3)
In 2001, Robertson et al.[43] published a meta-analysis of RCTs performed in New Zealand looking at exercise programs and injurious falls.[44–46] The authors calculated a 35% reduction in both falls and fall-related injuries among older people using home exercise programs Two other, subsequent RCTs have looked at exercise programs, with one study finding a 10% reduction in falls and a decrease in fall-related injuries[47] and the other finding no effect.[48]Many of these studies are challenged by smaller sample sizes, heterogeneity of follow-up protocols, and self-reported injury outcome measures.
PICO 4: Should physical environment modifications be used to prevent fall-related injuries in the elderly? (Table 4)
It is certainly plausible that flooring and shoe choices, along with other physical environment modifications, may help decrease the risk of injurious falls. In a cluster-randomized pilot study, Drahota et al.[49] examined flooring in particular and found that springier floors were half as likely to lead to fall-related injuries among hospitalized elderly, but the difference was not significant owing to small sample sizes. The rate of falls was equal in both groups. Investigators in Norway examined nearly 200,000 person-hours of community-dwelling elderly and found benefits to community-based programs designed to eliminate household environmental hazards, with substantial decreases in admissions for fall-related fractures.[50] A much smaller study in the United States had not demonstrated a benefit, but noted that certain aspects, such as grab bars, warranted further study.[51]
Of note, for institution-dwelling elderly, several investigators have examined the effects of restraint use for individuals with dementia. While this is not exactly an environmental modification, it is worth noting that restraints do not seem to improve safety and may in fact be associated with more injuries.[67][68]
PICO 5: Should risk factor screening be used to prevent fall-related injuries in the elderly? (Table 5)
Risk factor screening has been studied extensively by the Epidémiologie de l’ostéoporose investigators. In a series of articles beginning in 1996, the authors have identified various risk factors associated with hip fracture risk, such as neurologic and visual impairment,[52] markers of bone resorption,[53] and bone density.[54] The authors have also described various algorithms combining clinical assessments and bone screening examinations to better assess at-risk elderly.[55][56]
PICO 6: Should interventions tailored to the population or individual be used to prevent fall-related injuries in the elderly? (Table 6)
Many groups have attempted to decrease fall-related injuries by using multiple strategies at a time. For example, investigators in Finland created a program that combined strength and balance training, medical review and referrals, medication review, nutrition counseling, and home hazard assessment and found a nearly 30% reduction in fall-related injuries.[62] Combining these strategies has been commonly studied, with mixed results, although the larger studies seem to have more positive outcomes.[59][61][62]
Discussion
In summary, fall-related injuries are a significant problem among the elderly; more than 95% of hip fractures are caused by falls. Each year, there are more than 258,000 fall-induced hip fractures, and the rate for females is almost twice the rate for males.[65] Hip fractures in particular are associated with increased mortality, even after adjusting for preexisting factors.[69] It is for that reason we examined the literature regarding the effectiveness of fall-related injury prevention strategies.
There has been considerable interest in the use of bone mineral–enhancing agents for the prevention of osteoporotic fractures in the elderly. This makes intuitive sense, as bone mineral density can be improved with vitamin D and calcium supplementation;[70] vitamin D in particular may also improve muscle strength and balance.[71] However, one of the challenges in interpreting the literature is the wide variation in study population characteristics and dosing strategies. In addition, sex and racial homogeneity predominated, which may decrease generalizability. However, the bulk of the evidence favors higher-dose vitamin D supplementation, particularly in independent elderly.
Hip protectors seem to be modestly effective at secondary prevention of fall-related fractures. However, a key issue is compliance, which is generally poor for these devices,[27][31][36][38][39][41][42][72–76] and the negligible treatment effect for community-dwelling elderly suggests that the number needed to treat would be excessive for that population.[27]
Strength and balance training are reasonable strategies for decreasing fall-related injuries. Exercise may decrease the likelihood of falling in the first place, and then, by improving general health and perhaps bone density, decrease the likelihood of having injury. Prospective RCTs support the use of exercise programs to decrease falls, but the data on decreasing fall-related injury are mixed, possibly partly attributable to the heterogeneity of study participants and smaller sample sizes.
Environmental hazard reduction has been studied, but with mixed results. Like many of these interventions, potential hazards are varied, and the ability to make modifications to the environment may also be imperfect.
Risk factor screening, while not directly an intervention, may be able to help identify higher-risk individuals for targeted strategies. For example, identifying people with visual impairment or balance deficits, limiting medications that may cause altered mentation or strength, and treating conditions such as nocturia, which may cause night falls, are all potential strategies to reduce fall-related injuries.
Finally, mixed strategies seem to help decrease fall-related injuries among the elderly, but the results are hampered by heterogeneity. In addition, the largest positive studies have been conducted in health care systems with universal access and a central payer. In alternative health care systems, or fee-for-service, cost-effectiveness of these comprehensive strategies would have to be assessed.
Recommendations
PICO 1: Should bone mineral–enhancing agents be used to prevent fall-related injuries in the elderly? (Table 7)
Recommendation: We conditionally recommend vitamin D and calcium supplementation for frail elderly individuals.
Although the data vary widely in study population and dosing strategy, it is safe to say that most studies favor a higher dose of vitamin D. Usual daily dosing ranging from 400 IU to 800 IU cholecalciferol, while another regimen involves 100,000 IU cholecalciferol every 4 months. Calcium dosing ranges from 1,000 to 1,500 mg/day. This has been shown to improve muscle strength and balance. Sex and racial homogeneity predominated in most of the studies, which may decrease generalizability.
PICO 2: Should hip protectors be used to prevent fall-related injuries in the elderly?
Recommendation: We conditionally recommend hip protectors for frail elderly individuals in the appropriate environment.
It is a known fact that hip fractures cause substantial morbidity, disability, and mortality among the elderly. Evidence shows a modest decrease in hip fractures when worn properly. The major issue with hip protectors is compliance; especially with unattractive hip widening that accompanies usage of protective padding.
PICO 3: Should exercise programs be used to prevent fall-related injuries in the elderly?
Recommendation: We conditionally recommend evidence-based exercise programs for frail elderly individuals.
The data vary in modesty regarding use of exercise programs in decreasing fall-related injuries, mostly due to small sample sizes. Nevertheless, most of the results depict reduction of injuries related to falls, when used in the appropriate setting.
PICO 4: Should physical environment modifications be used to prevent fall-related injuries in the elderly?
Recommendation: We conditionally recommend physical environment modification for frail elderly people.
Owing to difficulty in making appropriate changes to the environmental factors that truly affect fall-related injuries, the data render mixed results in this arena; although grab bars, clutter removal, etc. seem to be of benefit.
PICO 5: Should risk factor screening be used to prevent fall-related injuries in the elderly?
Recommendation: We conditionally recommend frailty screening for the elderly.
Although risk factor screening is not a direct intervention, it may be used as a mechanism of which higher-risk individuals can be targeted for appropriate risk-reduction interventions.
PICO 6: Should multiple interventions tailored to the population or individuals be used to prevent fall-related injuries in the elderly?
Recommendation: We strongly recommend risk stratification with targeted, comprehensive risk-reduction strategies tailored to particular high-risk groups.
Although mixed strategies seem to assist in decreasing fall-related injuries among the elderly, the results are hampered by heterogeneity such as differing medication dosages, variable sample sizes, and participant adherence. The largest favorable studies have been conducted in health care systems with universal access and a central payer. In alternative health care systems (or fee-for-service-systems), cost-effectiveness of these comprehensive strategies would have to be assessed.
Conclusion
In summary, several strategies have been found to decrease the risk of fall-related injuries among the elderly; but racial, socioeconomic, and population disparities have created a knowledge gap and may limit generalizability. This committee recommends further research to strengthen future evidence-based guidelines.
Authorship
M.L.C. contributed to conceptualization, evidence grading, and manuscript preparation. T.D. and P.V. contributed to evidence grading and manuscript preparation. A.B.C., R.B., A.M., and W.G. participated in evidence grading and editorial support.
Disclosure
The authors declare no conflicts of interest. They did not receive funding for this work.
References
- Hayes WC, Myers ER, Robinovitch SN, Van Den Kroonenberg A, Courtney AC, McMahon TA. Etiology and prevention of age-related hip fractures. Bone. 1996;18(Suppl 1):77S–86S.
- Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050–1056.
- Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18(2):141–158.
- Rapp K, Lamb SE, Erhardt-Beer L, Lindemann U, Rissmann U, Klenk J, Becker C. Effect of a statewide fall prevention program on incidence of femoral fractures in residents of long-term care facilities. J Am Geriatr Soc. 2010;58(1):70–75.
- Centers for Disease Control and Prevention. Older adult falls: get the facts. Available at: http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed June 1, 2015.
- Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21(8):1295–1306.
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(12):2234–2243.
- Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, Rowe BH. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;2:CD007146.
- Chang JT, Morton SC, Rubentstien LZ, Mojica WA, Maglione M, Suttorp MJ, Roth EA, Shekelle PG. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials.BMJ. 2004;328(7441):680.
- Schwenk M, Lauenroth A, Stock C, Moreno RR, Oster P, McHugh G, Todd C, Hauer K. Definitions and methods of measuring and reporting on injurious falls in randomised controlled fall prevention trials: a systematic review.BMC Med Res Methodol. 2012;12:50.
- Jaeschke R, Guyatt GH, Dellinger P, Schünemann H, Levy MM, Kunz R, Norris S, Bion J; GRADE Working Group. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008;337:a744.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926.
- Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293(18):2257–2264.
- Grant AM, Avennell A, Campbell MK, McDonald AM, MacLennan GS, McPherson GC, Anderson FH, Cooper C, Francis RM, Donaldson C, et al. Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trial. Lancet. 2005;365(9471):1621–1628.
- Chapuy MC, Arlot ME, Delmas PD, Meunier PJ. Effect of calcium and cholecalciferol treatment for three years on hip fractures in elderly women. BMJ. 1994;308(6936):1081–1082.
- Lips P, Graafmans WC, Ooms ME, Bezemer PD, Bouter LM. Vitamin D supplementation and fracture incidence in elderly persons. A randomized, placebo-controlled clinical trial. Ann Intern Med. 1996;124(4):400–406.
- Dawson-Hughes B, Harriss SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337(10):670–676.
- Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res. 2000;15(6):1113–1118.
- Meyer HE, Smedshaug GB, Kvaavik E, Falch JA, Tverdal A, Pedersen JI. Can vitamin D supplementation reduce the risk of fracture in the elderly? A randomized controlled trial. J Bone Miner Res. 2002;17(4):709–715.
- Chapuy MC, Pamphile R, Paris E, Kempf C, Schlichting M, Arnaud S, Garnero P, Meunier PJ. Combined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II study. Osteoporos Int. 2002;13(3):257–264.
- Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ. 2003;326(7387):469.
- Law M, Withers H, Morris J, Anderson F. Vitamin D supplementation and the prevention of fractures and falls: results of a randomised trial in elderly people in residential accommodation. Age Ageing. 2006;35(5):482–486.
- Sato Y, Iwamoto J, Kanoko T, Satoh K. Low-dose vitamin D prevents muscular atrophy and reduces falls and hip fractures in women after stroke: a randomized controlled trial. Cerebrovasc Dis. 2005;20(3):187–192.
- Sato Y, Kanoko T, Satoh K, Iwamoto J. Menatetrenone and vitamin D2 with calcium supplements prevent nonvertebral fracture in elderly women with Alzheimer’s disease. Bone. 2005;36(1):61–68.
- Smith H, Anderson F, Raphael H, Maslin P, Crozier S, Cooper C. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women—a population-based, randomized, double-blind, placebo-controlled trial.Rheumatology (Oxford). 2007;46(12):1852–1857.
- Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med. 1992;327(23):1637–1642.
- Ringe JD. The effect of Vitamin D on falls and fractures. Scand J Clin Lab Invest Suppl. 2012;243:73–78.
- Parker MJ, Gillespie LD, Gillespie WJ. Hip protectors for preventing hip fractures in the elderly. Cochrane Database Syst Rev. 2004;3:CD001255.
- Lauritzen JB, Petersen MM, Lund B. Effect of external hip protectors on hip fractures. Lancet. 1993;341(8836):11–13.
- Kannus P, Parkkari J, Niemi S, Pasanen M, Palvanen M, Jarvinen M, Vuori I. Prevention of hip fracture in elderly people with use of a hip protector. N Engl J Med. 2000;343(21):1506–1513.
- Chan DK, Hillier G, Coore M, Cooke R, Monk R, Mills J, Hung WT. Effectiveness and acceptability of a newly designed hip protector: a pilot study. Arch Gerontol Geriatr. 2000;30(1):25–34.
- Hubacher M, Wettstein A. Acceptance of hip protectors for hip fracture prevention in nursing homes. Osteoporos Int. 2001;12(9):794–799.
- Harada A, Mizuno M, Takemura M, Tokuda H, Okuizumi H, Niino N. Hip fracture prevention trial using hip protectors in Japanese nursing homes. Osteoporos Int. 2001;12(3):215–221.
- van Schoor NM, Smit JH, Twisk HW, Bouter LM, Lips P. Prevention of hip fractures by external hip protectors: a randomized controlled trial. JAMA. 2003;289(15):1957–1962.
- Birks YF, Hildreth R, Campbell P, Sharpe C, Torgerson DJ, Watt I. Randomised controlled trial of hip protectors for the prevention of second hip fractures. Age Ageing. 2003;32(4):442–444.
- Cameron ID, Cumming RG, Kurrle SE, Quine S, Lockwood K, Salkeld G, Finnegan T. A randomised trial of hip protector use by frail older women living in their own homes. Inj Prev. 2003;9(2):138–141.
- Meyer G, Warnke A, Bender R, Mühlhauser I. Effect on hip fractures of increased use of hip protectors in nursing homes: cluster randomised controlled trial. BMJ. 2003;326(7380):76.
- Birks YF, Porthouse J, Addie C, Loughney K, Saxon L, Baverstock M, Francis RM, Reid DM, Watt I, Torgerson DJ. Randomized controlled trial of hip protectors among women living in the community. Osteoporos Int. 2004;15(9):701–706.
- O’Halloran PD, Cran GW, Beringer TR, Kernohan G, O’Neill C, Orr J, Dunlop L, Murray LJ. A cluster randomised controlled trial to evaluate a policy of making hip protectors available to residents of nursing homes. Age Ageing. 2004;33(6):582–588.
- Kiel DP, Magaziner J, Zimmerman S, Ball L, Barton BA, Brown KM, Stone JP, Dewkett D, Birge SJ. Efficacy of a hip protector to prevent hip fracture in nursing home residents: the HIP PRO randomized controlled trial. JAMA. 2007;298(4):413–422.
- Koike T, Orito Y, Toyoda H, Tada M, Sugama R, Hoshino M, Nakao Y, Kobayashi S, Kondo K, Hirota Y, Takaoka K. External hip protectors are effective for the elderly with higher-than-average risk factors for hip fractures.Osteoporos Int. 2009;20(9):1613–1620.
- Sawka AM, Boulos P, Beattie K, Thabane L, Papioannou A, Gafni A, Cranney A, Zytaruk N, Hanley DA, Adachi JD. Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2005;16(12):1461–1474.
- Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta-analysis of individual-level data. J Am Geriatr Soc. 2002;50(5):905–911.
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–1069.
- Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ. 2001;322(7288):697–701.
- Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ. 2001;322(7288):701–704.
- Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil. 2005;84(4):238–250.
- Sakamoto K, Nakamura T, Hagina H, Endo N, Mori S, Muto Y, Harada A, Nakano T, Itoi E, Yoshimura M, et al. Effects of unipedal standing balance exercise on the prevention of falls and hip fracture among clinically defined high-risk elderly individuals: a randomized controlled trial. J Orthop Sci. 2006;11(5):467–472.
- Drahota AK, Ward D, Udell JE, Soilemezi D, Ogollah R, Higgins B, Dean TP, Severs M. Pilot cluster randomised controlled trial of flooring to reduce injuries from falls in wards for older people. Age Ageing. 2013;42(5):633–640.
- Sattin RW, Rodriguez JG, DeVito CA, Wingo PA. Home environmental hazards and the risk of fall injury events among community-dwelling older persons. Study to Assess Falls Among the Elderly (SAFE) Group. J Am Geriatr Soc. 1998;46(6):669–676.
- Ytterstad B. The Harstad injury prevention study: community based prevention of fall-fractures in the elderly evaluated by means of a hospital based injury recording system in Norway. J Epidemiol Community Health. 1996;50(5):551–558.
- Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Breart G. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348(9021):145–149.
- Garnero P, Dargern-Molin P, Hans D, Schott AM, Breart G, Meunier PJ, Delmas PD. Do markers of bone resorption add to bone mineral density and ultrasonographic heel measurement for the prediction of hip fracture in elderly women? The EPIDOS prospective study. Osteoporos Int. 1998;8(6):563–569.
- Schott AM, Cornier D, Hans D, Favier F, Hausherr E, Dargent-Molina P, Delmas PD, Ribot C, Sebert JL, Breart G, Meunier PJ. How hip and whole-body bone mineral density predict hip fracture in elderly women: the EPIDOS Prospective Study. Osteoporos Int. 1998;8(3):247–254.
- Dargent-Molina P, Douchin MN, Cormier C, Meunier PJ, Breart G, EPIDOS Study Group. Use of clinical risk factors in elderly women with low bone mineral density to identify women at higher risk of hip fracture: The EPIDOS prospective study. Osteoporos Int. 2002;13(7):593–599.
- Dargent-Molina P, Piault S, Breart G. A comparison of different screening strategies to identify elderly women at high risk of hip fracture: results from the EPIDOS prospective study. Osteoporos Int. 2003;14(12):969–977.
- Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporos Int. 2008;19(6):801–809.
- Campbell AJ, Robertson MC, La Grow SJ, Kerse NM, Sanderson GF, Jacobs RJ, Sharp DM, Hale LA. Randomised controlled trial of prevention of falls in people aged > or =75 with severe visual impairment: the VIP trial.BMJ. 2005;331(7520):817.
- Jensen J, Lundin-Olsson L, Nyberg L, Gustafson Y. Fall and injury prevention in older people living in residential care facilities. A cluster randomized trial. Ann Intern Med. 2002;136(10):733–741.
- Jensen J, Nyberg L, Gustafson Y, Lundin-Olsson L. Fall and injury prevention in residential care—effects in residents with higher and lower levels of cognition. J Am Geriatr Soc. 2003;51(5):627–635.
- Kita K, Hujino K, Nasu T, Kawahara K, Sunami Y. A simple protocol for preventing falls and fractures in elderly individuals with musculoskeletal disease. Osteoporos Int. 2007;18(5):611–619.
- Palvanen M, Kannus P, Piirtola M, Niemi S, Parkkari J, Järvinen M. Effectiveness of the Chaos Falls Clinic in preventing falls and injuries of home-dwelling older adults: a randomised controlled trial. Injury. 2014;45(1):265–271.
- Reinsch S, MacRae P, Lachenbruch PA, Tobis JS. Attempts to prevent falls and injury: a prospective community study. Gerontologist. 1992;32(4):450–456.
- Woolf AD, Akesson K. Preventing fractures in elderly people. BMJ. 2003;327(7406):89–95.
- Health Quality Ontario. Prevention of falls and fall-related injuries in community-dwelling seniors: an evidence-based analysis. Ont Health Technol Assess Ser. 2008;8(2):1–78.
- Sawka AM, Ismaila N, Cranney A, Thabane L, Kastner M, Gafni A, Woodhouse LJ, Crilly R, Cheung AM, Adachi JD, et al. A scoping review of strategies for the prevention of hip fracture in elderly nursing home residents.PLoS One. 2010;5(3):e9515.
- Frank C, Hodgetts G, Puxty J. Safety and efficacy of physical restraints for the elderly. Review of the evidence. Can Fam Physician. 1996;42:2402–2409.
- Wang WW, Moyle W. Physical restraint use on people with dementia: a review of the literature. Aust J Adv Nurs. 2005;22(4):46–52.
- Empana JP, Dargent-Molina P, Breart G. Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004;52(5):685–690.
- Ooms ME, Roos JC, Bezemer PD, van der Vijgh WJ, Bouter LM, Lips P. Prevention of bone loss by vitamin D supplementation in elderly women: a randomized double-blind trial. J Clin Endocrinol Metab. 1995;80(4):1052–1058.
- Bischoff-Ferrari HA, Dietrich T, Orav EJ, Dawson-Hughes B. Positive association between 25-hydroxy vitamin D levels and bone mineral density: a population-based study of younger and older adults. Am J Med. 2004;116(9):634–639.
- Berry SD, Misra D, Hannan MT, Kiel DP. Low acceptance of treatment in the elderly for the secondary prevention of osteoporotic fracture in the acute rehabilitation setting. Aging Clin Exp Res. 2010;22(3):231–237.
- Kannus P, Parkkari J. Prevention of hip fracture with hip protectors. Age Ageing. 2006;35(Suppl 2):ii51–ii54.
- Parkkari J, Heikkila J, Kannus IP. Acceptability and compliance with wearing energy-shunting hip protectors: a 6-month prospective follow-up in a Finnish nursing home. Age Ageing. 1998;27(2):225–229.
- van Schoor NM, Deville WL, Bouter LM, Lips P. Acceptance and compliance with external hip protectors: a systematic review of the literature. Osteoporos Int. 2002;13(12):917–924.
- Villar MT, Hill P, Inskip H, Thompson P, Cooper C. Will elderly rest home residents wear hip protectors? Age Ageing. 1998;27(2):195–198.
Tables
Table 1. Strength of Evidence for Bone MineralYEnhancing Agents in the Prevention of Fall-Related Injuries in the Elderly
|
Study |
Study Overview and Effect Size |
Risk of Bias |
Quality |
Importance |
|
Bischoff-Ferrari et al., 2005[13] |
Meta-analysis. Compared low (400 IU) and high (700Y 800 IU) dose Vit. D3 regimens. Bene?ts observed for higher dose Vit D in ambulatory or institutionalized elderly. Hip fx (n = 5572): 0.74 (0.68Y0.87) Other nonvertebral fx (n = 6098): 0.77 (0.68Y0.87) |
Low |
High |
High |
|
Grant et al., 2005[14] |
RCT. 800 IU Vit. D3, 1000 mg Ca2+, 800 IU Vit. D3 + 1000 mg Ca2+, or placebo. Compliance with Ca2+ lower. Findings do not support supplementation of oral Ca2+ or Vit. D routinely. Female gender bias. All fx (n = 5292): NS for Vit D, Calcium, or both |
Low |
|
|
|
Chapuy et al., 1994[15 ] |
RCT. 800 IU Vit. D3 + 1200 mg Ca2+ vs placebo. Decrease in hip fractures and other nonvertebral fractures. All fx (n = 2303): 0.79 (0.69Y0.92) |
Low |
|
|
|
Lips et al., 1996[16] |
RCT. Vit. D3 400 IU vs placebo. No decrease in incidence of hip fractures or other peripheral fractures in Dutch elderly. All fx (n = 2578): 1.10 (0.87Y1.39) |
Low |
|
|
|
Dawson-Hughes et al., 1997[17 ] |
RCT. 700 IU Vit. D3 + 500 mg Ca2+ vs placebo. Calcitriol levels increased in males vs females. Higher prevalence of lower winter time Calcitriol values increased risk of bone loss in elderly males. All fx (n = 389): 0.46 (0.24Y0.88) |
Low |
|
|
|
Pfeifer et al., 2000[18 ] |
RCT. 800 IU Vit. D3 + 1200 mg Ca2+ vs 1200 mg Ca2+. Improved physiology and biomechanics but not fall risk or injuries. All fx (n = 137): 0.48 (0.13Y1.78) |
Moderate |
|
|
|
Meyer et al., 2002[19] |
RCT. 400 IU Vit. D3 vs placebo. No fracture prevention effect in NH population fracture in frail elderly. All fx (n = 1144): 0.92 (0.68Y1.24) |
Low |
|
|
|
Chapuy et al., 2002[20] |
RCT. 800 IU Vit. D3 + 1200 mg Ca2+ vs placebo. Decreased both hip bone loss and risk of hip fracture in institutionalized elderly. All fx (n = 583): 0.85 (0.64Y1.13) |
Low |
|
|
|
Trivedi et al., 2003[21] |
RCT. 100,000 IU Vit. D3 every 4 months vs placebo. May prevent fractures without adverse effects in males and females. All fx (n = 2686): 0.67 (0.46Y0.99) |
Low |
|
|
|
Law et al., 2006[22 ] |
RCT. 1100 IU Vit. D3 vs control. Cluster design. No evidence that Vit. D prevents fractures or falls in elderly living in care homes. Fractures (n = 3717): NS |
Low |
|
|
|
Sato et al., 2005[23] |
RCT. 1000 IU Vit. D2 + 600 mg Ca2+ vs control. Low volume. 59% falls reduction. CI 95%, 28 Y 81%; p = 0.003. Vit. D may increase musculoskeletal strength, thereby decrease falls. Female gender bias. Hip fx (n = 96): log-rank p = 0.049 |
Moderate |
|
|
|
Sato et al., 2005[24 ] |
RCT. 45 mg menatetrenone + 1000 IU Vit. D2 + 600 mg Ca2+ vs control. Increased bone density in elderly females with Alzheimer, prevented nonvertebral fractures. All fx (n = 200): OR 7.5, p G 0.01 favoring treatment |
Moderate |
|
|
|
Smith et al., 2007[25] |
RCT. Annual intramuscular Vit. D2 300,000 IU vs placebo. No impact on fracture risk after 3 years. All fx (n = 9440): NS |
Low |
|
|
|
Chapuy et al. 1992[26] |
RCT. 800 IU Vit. D3 + 1200 mg Ca2+ vs placebo. Decreased fracture risk among ambulatory women. All fx (n = 3270): 32% fewer (p = 0.04), hip fx: 43% fewer (p = 0.02) |
|
|
|
|
Ringe 2012[27 ] |
Rev. A thorough analysis supporting clinical experience of Vit. D-Ca2+ supplementation, depends on factors related to patient selection, medical intervention, and study design N/A |
Moderate |
|
|
Table 2. Strength of Evidence for Hip Protectors in the Prevention of Fall-Related Injuries in the Elderly
|
Study |
Study Overview and Effect Size |
Risk of Bias |
Quality |
Importance |
|
Parker et al., 2004[28] |
Meta-analysis. Quasi RCT. No adverse effects. Compliance low. No difference in home patients, but makes a difference in institutionalized hip fracture patients Hip fx: 0.81 (0.66Y0.99) |
Low |
High |
High |
|
Lauritzen et al., 1993[29] |
RCT. External hip devices can decrease hip fractures, but compliance is the main issue Hip fx (n = 665): 0.44 (0.17Y1.14) |
Low |
|
|
|
Kannus et al., 2000[30] |
RCT. Attitudes, education, and motivation of staff is a factor in achieving good compliance Hip fx (n = 1801): 0.4 (0.2Y0.8) |
Low |
|
|
|
Chan et al., 2000[31] |
RCT. Majority of falls occurred during day. Data on orientation incomplete. Compliance and appearance are both issues. Protective against hip fractures Hip fx (n = 71): 0.47 (0.12Y1.82) |
Moderate |
|
|
|
Hubacher and Wettstein 2001[32] |
RCT. Senior citizens initially prepared to wear protector tended to be physically restricted Hip fx (n = 548): 1.49 (0.31Y7.14) |
Moderate |
|
|
|
Harada et al., 2001[33] |
RCT. When Cox proportional hazard regression analysis used, concluded that hip protector is bene?cial for prevention of hip fractures. Female gender bias Hip fx (n = 164): 19.8% vs 2.0% per year, p = 0.01 |
Moderate |
|
|
|
Van Schoor et al., 2003[34] |
RCT. Targeted age 9 70 with low bone density. No statistically signi?cant difference between intervention group and control group. Hip fx: (n = 561): 1.05 (0.55Y2.02) |
Low |
|
|
|
Birks et al., 2003[35] |
RCT. Common dwelling study. No evidence that hip protectors are bene?cial Hip fx: (n = 366): 1.18 (0.79Y1.52) |
Low |
|
|
|
Cameron et al., 2003[36] |
RCT. Due to incomplete adherence, overall effectiveness not established Hip fx (n = 600): 0.94 (0.53Y1.67) |
Low |
|
|
|
Meyer et al., 2003[37] |
RCT. After adjustment for cluster randomization, proportion of fallers with compliant increased. Structural educational program was bene?cial Hip fx (n = 982): 0.57, p = 0.072) |
Low |
|
|
|
Birks et al., 2004[38] |
RCT. No evidence hip protectors among females living independently and at high risk had more fractures Second hip fx (n = 4169): 1.18 (0.80Y1.75) |
Low |
|
|
|
O’Halloran et al., 2004[39] |
RCT. Should consider targeting those with cognitive impairment. More apt to wear hip protectors Hip fx (n = 4117): 1.05 (0.75Y1.46) |
Low |
|
|
|
Kiel et al., 2007[40] |
RCT. 1 vs 2 hip protectors study terminated due to lack of ef?cacy Hip fx (n = 1042): 1.24 (0.65Y2.35) |
Low |
|
|
|
Koike et al., 2009[41] |
RCT. Cluster study. Hip protectors shown to decrease hip fractures in frail. Female gender bias Hip fx (n = 672): 0.38 (0.14Y0.98) |
Low |
|
|
|
Sawka et al., 2005[42] |
Review. Meta-analysis of 7 trials (12Y28 mos). Heterogeneity in studies. Little to no evidence to support use of hip protectors outside nursing home Hip fx (n = 5696): 0.56 (0.31Y1.01) |
Moderate |
|
|
Table 3. Strength of Evidence for Exercise Programs in the Prevention of Fall-Related Injuries in the Elderly
|
Study |
Study Type and Effect Size |
Risk of Bias |
Quality |
Importance |
|
Robertson et al., 2002[43] |
MA. Less known about effectiveness in preventing fall-related injuries. Cost per fall established. Some potential interventions of unknown effectiveness Injury (n = 1016): 0.65 (0.57Y0.75) |
Low |
Moderate |
High |
|
Campbell et al., 1997[44] |
RCT. After 6 mos, balance improved. Individual program of strength and balance retraining exercises. Improved physical function and effective in decreasing falls/injuries in females 9 80. Female gender bias Injury (n = 233): 0.61 (0.39Y0.97) |
Low |
|
|
|
Robertson et al., 2001[45] |
RCT. Single NH based program. Serious injuries and hospital admissions decreased. Cost effective in participants 9 80 Injury (n = 240): NS |
Moderate |
|
|
|
Robertson et al., 2001[46] |
RCT. Nurse led home based program. Effective program strategy should be combined with other successful interventions to form part of a home program Injury (n = 780): NS |
Low |
|
|
|
Means et al., 200547 Sakamoto et al., 2005[48] |
RCT. Showed decrease in injuries in 6 months post intervention Injury (n = 238): 10% decreased risk of falls (p = 0.034) |
Moderate Low |
|
|
|
Robertson et al., 2002[43] |
RCT. Unipedal standing balance exercise is effective to prevent falls, but not shown to be statistically signi?cant in preventing hip fractures Injury (n = 553): NS |
Low |
|
|
Table 4. Strength of Evidence for Physical Environment Modifications in the Prevention of Fall-Related Injuries in the Elderly
|
Study |
Study Type and Effect Size |
Risk of Bias |
Quality |
Importance |
|
Drahota et al., 2013[49] |
RCT. Future research should assess shock-absorbing ?ooring with better ‘‘push/pull’’ properties, and explore fall risks Injury (n = 442): 0.58 (0.18Y1.91) |
Low |
Moderate |
High |
|
Sattin et al., 1998[50] |
Case control study. After adjusting for important confounding factors, most of hazards were not associated with increased number of tripping hazards. Fall prevention strategies may have less potential effect than thought. Usefulness of grab bars appear to warrant further evaluation Injury (n = 961): NS |
Moderate |
|
|
|
Ytterstad 1996[51] |
Cohort study. Fall fracture prophylaxis in aged is possible in community based setting that utilizes high quality, local injury data Injury (n = 181,881 person-years): 26.3% decrease fx in private homes, NS for nursing homes |
Moderate |
|
|
Table 5. Strength of Evidence for Risk Factor Screening in the Prevention of Fall-Related Injuries in the Elderly
|
Study |
Study Type and Effect Size |
Risk of Bias |
Quality |
Importance |
|
Dargent-Molina EPIDOS Studies[52,56] |
Obs. Proposed screening strategy has the same discriminant value for hip fractures as BMD used as a population screening Hip fx (n = 7575): RR 1.1Y1.5 with certain risk factors |
Moderate |
Moderate |
Moderate |
EPIDOS, Epidémiologie de l’ostéoporose.
Table 6. Strength of Evidence for the Use of Multiple Simultaneous Interventions in the Prevention of Fall-Related Injuries in the Elderly
|
Study |
Study Type and Effect Size |
Risk of Bias |
Quality |
Importance |
|
Berggren et al., 2008[57] |
RCT. Team applying comprehensive geriatric assessment and rehab, including prevention and treatment of fall risk factors decreased inpatient falls and injuries, but no statistically signi?cant effect of program detected after discontinuance Injury (n = 199): NS |
Low |
Moderate |
High |
|
Campbell et al., 2005[58] |
RCT. Home safety program decreased falls, and more cost effective in elderly with poor vision. Otago exercise program not effective in decreasing falls, due to low compliance Injury (n = 391): NS |
Low |
|
|
|
Jensen et al., 2002[59] |
RCT. 11 wk multidisciplinary program run by staff and residents of home. May reduce falls and femoral fractures Femur fx (n = 439): 0.23 (0.06Y0.94) |
Low |
|
|
|
Jensen et al., 2003[60] |
RCT. Cluster study. 9 residential facilities.Higher Mini Mental Status Exam group led to fewer falls. Lower MMSE group did not respond to intervention Femur fx (n = 378): 0 vs 10 (p = 0.006) |
Low |
|
|
|
Kita et al., 2007[61] |
CS. Protocol safely implemented in large # of clinics in Japan. Decrease in frequency of falls and fractures suggests provides effective preventive care Any fx (n = 683): 47% fewer fractures (p G 0.01) |
Moderate |
|
|
|
Palvanen et al., 2014[62] |
RCT. Multifactorial group clinic Falls Prevention program effective in preventing falls of older adults by 30% Injury (1314): 0.74 (0.61Y0.89) |
Low |
|
|
|
Reinsch et al., 1992[63] |
RCT. 16 senior centers. No signi?cant difference in 1 year, time to ?rst fall. Secondary factors: strength, balance, fear of falling, perceived health did not change Injury (n = 230): NS |
Moderate |
|
|
|
Woolf and Akesson, 2003[64] |
Rev. Focused on prevention of fractures; reducing the number of falls, reducing the trauma associated with falls, and maximizing bone strength at all ages. No strong recommendations. N/A |
Moderate |
|
|
|
Health Quality Ontario 2008[65] |
Rev. Comprehensive GRADE-based review of risk factors and prevention. No strong recommendations N/A |
Low |
|
|
|
Sawka 2010[66] |
Rev. Systematic review of fall-related injury prevention; favored Vitamin D supplementation. N/A |
Moderate |
|
|
Table 7. EAST Evidence-Based Recommendations for the Prevention of Fall-Related Injuries in the Elderly
|
PICO Question |
Recommendation |
|
Should bone mineralYenhancing agents be used to prevent fall-related injuries in the elderly? |
We conditionally recommend vitamin D and calcium supplementation for frail elderly individuals. |
|
Should hip protectors be used to prevent fall-related injuries in the elderly? |
We conditionally recommend hip protectors for frail elderly individuals in the appropriate environment. |
|
Should exercise programs be used to prevent fall-related injuries in the elderly? |
We conditionally recommend evidence-based exercise programs for frail elderly individuals. |
|
Should physical environment modi?cations be used to prevent fall-related injuries in the elderly? |
We conditionally recommend physical environment modi?cation for frail elderly people. |
|
Should risk factor screening be used to prevent fall-related injuries in the elderly? |
We conditionally recommend frailty screening for the elderly. |
|
Should multiple interventions tailored to the population or individuals be used to prevent fall-related injuries in the elderly? |
We strongly recommend risk strati?cation with targeted, comprehensive risk-reduction strategies tailored to particular high-risk groups. |