Geriatric Trauma (Update)
Archived PMG
Published 2010
Authors
Eastern Association for the Surgery of Trauma Workgroup
James Forrest Calland, M.D., F.A.C.S., Assistant Professor of Surgery, Box 800709 -- Department of Surgery, Charlottesville, VA 22908, calland@virginia.edu
Angela M. Ingraham, Resident in General Surgery, University of Cincinnati, 234 Goodman St., Mail Location 0558, Cincinnati, OH 45267, angieingraham@gmail.com
Niels D. Martin, M.D., F.A.C.S., Assistant Professor of Surgery, Thomas Jefferson University, 1100 Walnut Street, Suite 702, Philadelphia, PA 19107, niels.martin@jefferson.edu
Gary T. Marshall, MD, FACS, Assistant Professor of Surgery and Critical Care Medicine, University of Pittsburgh Medical Center, 200 Lothrop St. -- PUH F1266.2, Pittsburgh, PA 15213, marshallgt@upmc.edu
Carl I. Schulman, MD, PhD, MSPH, FACS, Associate Professor of Surgery, Co-Director - William Lehman Injury Research Center, Associate Director Surgical Residency Program DeWitt Daughtry Family Department of Surgery, P.O. Box 016960 (D-40) Miami, FL 33101, cschulman@med.miami.edu
Tristan Stapleton, Research Assistant, University of Virginia School of Medicine, Box 800709 -- Department of Surgery, Charlottesville, VA 22908, stapletontristan@gmail.com
Robert D. Barraco, MD, MPH, FACS, FCCP, Associate Professor of Surgery, University of South Florida College of Medicine Lehigh Valley Health Network, 1240 S Cedar Crest Blvd, Suite 308, Allentown, PA 18103, Robert_D.Barraco@lvhn.org
Executive summary
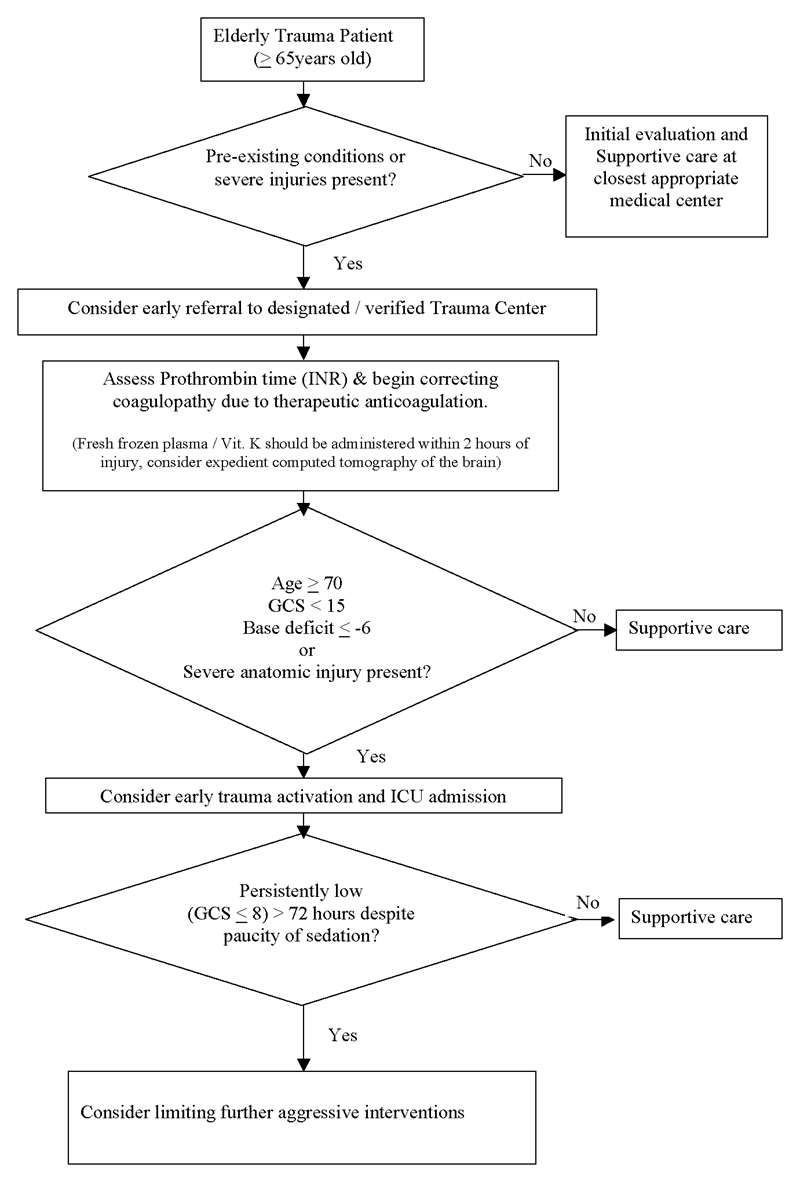
Elderly trauma patients (age >65) face an increased risk for adverse outcomes after injury. Several recommendations were carried forward from the previous version of this practice management guideline (PMG) either because of new supporting evidence, or because of an ongoing lack of published evidence to the contrary. This update asserts the following:
Triage Decisions
- Injured patients with advanced age (>65) and pre-existing medical conditions (PEC’s) should lower the threshold for field triage directly to a designated/verified trauma center. (Level 2)
- All other factors being equal, advanced patient age, in and of itself, is not predictive of poor outcomes following trauma, and therefore should NOT be used as the sole criterion for denying or limiting care in this patient population. (Level 2)
- With the exception of patients who are moribund on arrival, an initial aggressive approach should be pursued with the elderly trauma patient. (Level 2)
- A lower threshold for trauma activation should be utilized for injured patients>70 years age who are evaluated at trauma centers. (Level 3)
- Elderly patients with at least one body system with an AIS>3 should be treated in designated trauma centers, preferably in ICU’s staffed by surgeon-intensivists. (Level 3)
Managing Pre-injury Anticoagulation
- All elderly patients who receive daily therapeutic anticoagulation should have appropriate assessment of their coagulation profile as soon as possible after admission. (Level 3)
- Those with suspected head injury receiving daily anticoagulation should be evaluated with head CT as soon as possible after admission. (Level 3)
- Patients receiving warfarin with a post-traumatic intra-cranial hemorrhage should receive initiation of therapy to correct their INR toward a normal range within 2 hours of admission. (Level 3)
Critical Care
- No guidance is offered on indiscriminate use of pulmonary artery catheters based solely upon combinations of age and anatomic injury. (Level 3)
- No guidance can be offered regarding routine supraphysiologic resuscitation after injury in elderly patients. (Level 3)
- ICU admission should be considered for patients>65 with an initial base deficit>-6. (Level 3)
- In patients 65 years of age and older with a GCS < 8, if substantial improvement in GCS is not realized within 72 hours of injury, consideration should be given to limiting further aggressive therapeutic interventions. (Level 3)
Introduction
Elderly trauma patients face an increased risk for adverse outcomes after injury. As such, clinicians treating injured patients of advanced age need guidance in identifying the techniques and practices that have the proven capacity to improve outcomes. The original geriatric practice management guidelines (PMG) produced by this group (2001) addressed age-related triage criteria, resuscitation guidelines, and expectations for outcomes.[1] In the decade that has passed since its compilation, it could be argued that our understanding of these matters has not substantially changed except in the areas of supra-physiologic resuscitation, correction of medication-induced coagulopathy, and aggressiveness of initial assessment of the elderly injured patient. The recommendations promulgated by the original version of this practice management guideline not contradicted by subsequent literature have been retained within the structure of this update.
Our review confines itself to these topics and to scientific literature published after 12/31/1999, the last date of publication considered by the previous version of this PMG, except where direct comparison was required with citations from the previous version. Though independent risk for post-injury mortality may begin at a much younger age, the authors of this analysis have chosen to limit their recommendations to those patients 65 years of age or older. This threshold is consonant with what appears to be the most common assumptions and designations of existing trauma centers (TC) regarding advancing age.
I. Statement of the problem
As it pertains to the care of the injured, triage is variously defined as, “…the sorting of and allocation of treatment to patients and especially battle and disaster victims according to a system of priorities designed to maximize the number of survivors."[29] For the elderly patient, it is often difficult to accurately identify severity of injury and the degree of physiologic derangement because of age-related differences in biology, In addition, there also exists a complex interplay of social and cultural determinants that likely account for why many elderly trauma patients are not approached with the same aggressive form of evaluation afforded to younger patients.
Before a trauma system can influence the care of a population, the system must have access to those patients. Among academic trauma surgeons, a substantial difference of opinion appears to exist on whether falls from standing or hip fractures qualify as a “geriatric trauma” worthy of admission to a dedicated trauma service. This ambivalence seems to extend into the community where there exists substantial evidence that elderly patients are less likely to be referred to trauma centers – perhaps because of conflicting experimental evidence on survival of the elderly injured patient when treated at designated trauma centers.[2-6] For those aged patients who do reach the trauma center, there seems to be no emerging evidence against most of the fundamental tenets of the previous version of this PMG:
1) Advanced age is sufficient as the sole criteria for early evaluation of an elderly patient at a designated trauma center.
2) Elevated base deficit is an independent risk factor for adverse outcome in the elderly.
3) Despite its predictive capacity, age should not be used as the sole criteria for limiting or withdrawing care.
4) Pre-existing conditions and complications negatively influence outcomes.
5) An initial aggressive approach is appropriate for elderly patients with multi-system injury.
More specific guidance is needed, however, regarding triage issues, correction of medication-induced bleeding risk, and end-points for resuscitation.
Specific questions addressed by this update
1) Is there justification for advanced age as sole criteria for trauma team activation?
2) How should medication-induced coagulopathy be addressed during the early post-injury period?
3) Given the emergence of recent data pointing to complications and lack of benefit from supra-physiologic resuscitation after injury, is indiscriminate invasive cardiovascular monitoring with pulmonary artery catheters and supra-normal resuscitation still justified after injury in older patients?
The above items are the issues addressed by this update. One additional issue with particular relevance to the elderly not addressed by this update is the use of epidural catheters after blunt thoracic trauma, as it is adequately covered elsewhere by a separate guideline.
II. Process
An initial database query was undertaken using Medline with citations published between the years of 2000 and 2008. Using the search words “geriatric,” “trauma,” “elderly,” and “injury,” and by limiting the search to citations dealing with human subjects and published in the English language, > 400 citations were identified. Letters to the editor, case reports, reviews, and articles dealing with minor injury mechanisms, particularly hip fractures from slip-and-falls, were then excluded. The abstracts of the remaining citations were each reviewed, and those articles that did not address the issues pertinent to the three aims of this review and patient age criteria,>65, were further excluded. This yielded a total of 64 articles that comprised the initial evidentiary table. The bibliographies of these 64 articles were then further reviewed and 26 additional articles meeting the above-mentioned criteria were added for a total of 90 references within the evidentiary table. Each reference was then reviewed by two trauma surgeons, and consensus reached regarding appropriate classification of each reference according to the EAST primer on evidence based medicine. Seventeen articles were subsequently excluded from the evidentiary table after being identified as pure review articles with no new synthesis of information.
Criteria for achieving a specific classification in the final evidentiary table and the number of articles for each class are shown below:
Class I: Prospective randomized controlled trials - the gold standard of clinical trials. Some may be poorly designed, have inadequate numbers, or suffer from other methodological inadequacies. (0 references)
Class II: Clinical studies in which data was collected prospectively, and retrospective analyses that were based on clearly reliable data. Types of studies so classified include observational studies, cohort studies, prevalence studies, and case control studies. (38 references)
Class III: Studies based on retrospectively collected data. Evidence used in this class indicate clinical series, database or registry review, large series of case reviews, and expert opinion. (35 references)
The EAST Primer on Utilizing Evidence-based outcome measures to develop practice management guidelines suggest the following definitions (below) for levels of recommendation, which will be used to generate the summary recommendations or this committee:[30]
Level 1
The recommendation is convincingly justifiable based on the available scientific information alone. This recommendation is usually based on Class I data, however, strong Class II evidence may form the basis for a level 1 recommendation, especially if the issue does not lend itself to testing in a randomized format. Conversely, low quality or contradictory Class I data may not be able to support a level 1 recommendation.
Level 2
The recommendation is reasonably justifiable by available scientific evidence and strongly supported by expert opinion. This recommendation is usually supported by Class II data or a preponderance of Class III evidence.
Level 3
The recommendation is supported by available data but adequate scientific evidence is lacking. This recommendation is generally supported by Class III data. This type of recommendation is useful for educational purposes and in guiding future clinical research.
III. Recommendations
Question 1:
Should age be an independent determinant of whether trauma patients receive care as a trauma team “alert” at a designated trauma center?
A. Level I
- There are insufficient Class I and Class II data to support any standards regarding any of the questions posed by this query.
B. Level II
- Injured patients with advanced age (>65) and pre-existing medical conditions (PEC’s) should lower the threshold for field triage directly to a designated/verified trauma center.
- All other factors being equal, advanced patient age, in and of itself, is not predictive of poor outcomes following trauma, and therefore should NOT be used as the sole criterion for denying or limiting care in this patient population.
- With the exception of patients who are moribund on arrival, an initial aggressive approach should be pursued with the elderly trauma patient.
C. Level III
- A lower threshold for trauma activation should be utilized for injured patients>70 years age who are evaluated at trauma centers.
- Elderly patients with at least one body system with an AIS>3 should be treated in designated trauma centers, preferably in ICU’s staffed by surgeon-intensivists.
Question 2:
How should medication-induced coagulopathy be addressed during the early post-injury period?
A. Level I
- There are insufficient Class I and Class II data to support any standards regarding any of the questions posed by this query.
B. Level II
- There are insufficient Class I and Class II data to support any standards regarding any of the questions posed by this query.
C. Level III
- All elderly patients who receive daily therapeutic anticoagulation should have appropriate assessment of their coagulation profile as soon as possible after admission.
- All elderly patients with suspected head injury receiving daily anticoagulation should be evaluated with head CT as soon as possible after admission.
- Patients receiving warfarin with a post-traumatic intra-cranial hemorrhage should receive initiation of therapy to correct their INR toward a normal range within 2 hours of admission.
Question 3:
Is indiscriminate invasive cardiovascular monitoring with pulmonary artery catheters and supra-normal resuscitation still justified after injury in older patients?
A. Level I
- There are insufficient Class I and Class II data to support any standards regarding any of the questions posed by this query.
B. Level II
- There are insufficient Class I and Class II data to support any standards regarding any of the questions posed by this query.
C. Level III
- Elderly patients with at least one body system AIS>3 should be treated in designated trauma centers, preferably in ICU’s staffed by surgeon-intensivists.
- In patients 65 years of age and older with a GCS < 8, if substantial improvement in GCS is not realized within 72 hours of injury, consideration should be given to limiting further aggressive therapeutic interventions.
- Base deficit measurements may provide useful information in determining status of initial resuscitation and risk of mortality for geriatric patients. As such, ICU admission should be considered for patients>65 with an initial base deficit>-6.
IV. Scientific foundation
Triage and advanced age
One of the main topics addressed by this PMG is the manner in which elderly patients are triaged to trauma centers, and, if triaged to a trauma center, whether they should routinely receive a “trauma activation” level of initial care and what is an appropriate threshold for admitting them to an intensive care unit. Ample evidence demonstrates that injured elderly patients are less likely to receive care at trauma centers despite an increased risk for adverse outcomes.[8-15] A retrospective analysis of 10 years (1995-2004) of the Maryland Ambulance Information System by Chang et al, in 2008, found that among 26,565 patients, the risk for under-triage was significantly higher among those greater than 65 years of age (49.9% v 17.8%, p < 0.001).[15] Further, on multivariate analysis (controlling for year, sex, physiology, injury, mechanism, transport reasons, EMS provider level training, presence/absence of specific injuries, and jurisdictional region), age 65 or older emerged as an independent risk factor for under-triage (OR: 0.48 [0.3-0.76]) with inadequate training, unfamiliarity with protocol, and possible age bias listed by survey respondents as common reasons for not bringing elderly patients to trauma centers.
In comparisons of care at acute care hospitals (versus care at designated trauma centers) elderly patients appear to be less likely to experience preventable adverse events and are more likely to have a lower risk-adjusted mortality if treated at trauma centers and/or hospitals with dedicated surgeon-intensivists.[5-6] One large study of risk-adjusted outcomes found that patients < 55 years treated at trauma centers were at significantly decreased risk for post-injury mortality (>25% lower) whereas those who were > 55 years of age experienced no such apparent benefit.[5] Mackenzie and her coauthors admitted that this study may not be well-suited to answering the questions as to whether typical “elderly” injured patients should be treated at trauma centers because of the non-standard age cutoff and the low numbers of severely injured elderly patients in their sample. One piece of evidence supporting the benefit of triage to designated trauma centers was published by Meldon in 2002 and included risk-adjusted assessment of outcomes for a population of patients aged 80 years and older.[4] In this evaluation, outcomes varied between designated trauma centers and other non-designated acute-care settings. Not surprisingly, head injury, injury severity, and lack of TC verification are associated with hospital mortality in very elderly trauma patients.
Data from a well-executed single center study demonstrated a > 30% increase in risk-adjusted survival for elderly patients after initiating age >70 as an indicator for trauma alert in a busy urban trauma center.[11] Patients in this sample also were reported to have received liberal application of intensive care unit care and invasive monitoring. As such, we cannot yet determine which of these three interventions yielded the improved survival; it would seem prudent, however, to have a lower threshold for early aggressive evaluation and treatment until multi-center controlled trial data become available.
This update group is not able to carry forward the previous versions’ recommendations regarding the need to prevent complications because it seems nearly impossible to implement given that traumatologists’ preexisting universal imperative to prevent complications. Likewise, previous assertions that elderly patients with low revised trauma scores , Glasgow coma scores and respiratory rate upon presentation have a 100% mortality no longer seem relevant in an era when many more patients are receiving pre-hospital sedation, muscle relaxants, and intubation.
Correction of anticoagulation
Increasing numbers of elderly Americans take anticoagulants and anti-platelet agents for a variety of indications. Though these agents have proven overall benefit for patients at risk for thrombotic or embolic events, these medications increase the risk for post-injury hemorrhage. Ivascu, et al, demonstrated a > 75% decrease in mortality related to post-traumatic intra-cranial hemorrhage in elderly patients with coumadin-related coagulopathy after implementation of a protocol to ensure rapid head CT, initiation of INR-correcting therapy within 1.9 hrs and full correction of coagulopathy within 4 hours of admission.[16] The same authors suggested that reversal of INR is not necessary in the abscess of intracranial bleeding. The degree of correction indicated in elderly patients with intracranial bleeding is not completely clear, but one group of authors has concluded that INR should be rapidly corrected to a value of < 1.6 with FFP (15 mg/kg or approx 4 units) and Vit K IV.[17]
Little is known regarding the optimal means for correcting iatrogenic platelet dysfunction in injured patients, though it seems clear that patients taking anti-platelet agents are at increased risk for post-injury hemorrhage.[18-22]
End points of resuscitation
The previous version of this guideline advocated for near-ubiquitous use of swan-ganz catheters in moderately to severely injured elderly patients followed by optimization of cardiac output and oxygen delivery variables to supratherapeutic values.[1] Whereas it remains clear that younger patients progressively increase their cardiac index (CI) and oxygen delivery (DO[2]) following multiple trauma; elderly patients begin with low levels that often fail to increase.[23]
In one large multi-center examination of “dry” vs. “wet” classes of resuscitation in critically ill patients (not exclusively in elderly or injured patients), there was no difference in survival.[24] There was a marginal increase in ventilator free days in conservative fluid group without increased risk for dialysis. In other well-performed retrospective analysis not performed in elderly patients, multiple authors have described augmentation of post-injury DO[2] (to > 500) yielding an increased risk for intra-abdominal hypertension, compartment syndrome, and death and no survival benefit OR 0.86 (0.6 - 1.2).[25-26] Base deficit (≤ 6) is a marker of severe injury and significant mortality in all trauma patients, especially those patients > 55 years of age.[27]
V. Summary
In the relative absence of data to the contrary, our elderly patients should receive care at centers that have devoted specific resources to attaining excellence in the care of the injured using similar criteria to those employed in younger patients.. Pre-existing conditions (PEC’s) or Abbreviated Injury Severity Scores of > 3 in any single organ system > 3 dramatically increase the risk of poor outcome in elderly patients.
Age and Anticoagulants and anti-platelet agents increase the risk for post-injury hemorrhage and require assessment of coagulation profile swiftly following admission. Base deficit (≤ 6) is a marker of severe injury and significant mortality in all trauma patients, especially those patients > 55 years of age, and should be utilized in consideration for ICU admission. GCS<8, remaining low after 72 hours, provides important information regarding long term prognosis.
VI. Future investigations
Potentially uself areas for future study identified by this guideline include the following items:
- Creation of robust predictive models to facilitate quality / performance improvement in elderly populations, especially as such efforts pertain to triage decisions regarding invasive monitoring and aggressiveness of care.
- Acquisition of a deeper understanding as to when exactly “elderly” status begins physiologically.
- Whether medication-induced platelet dysfunction requires correction with the same urgency as warfarin induced coagulopathy.
- Finally, how can we accommodate the ever-increasing volume of elderly patients coming to our trauma centers in addition to our current patient volumes while maintaining high standards of care and avoiding mercenary triage decisions.
VII. References
- Jacobs DG, Plaisier BR, Barie PS, et al. Practice management guidelines for geriatric trauma: the EAST Practice Management Guidelines Work Group. J Trauma. Feb 2003;54(2):391-416.
- Rzepka SG, Malangoni MA, Rimm AA. Geriatric trauma hospitalization in the United States: a population-based study. J Clin Epidemiol. Jun 2001;54(6):627-633.
- Tepas JJ, 3rd, Veldenz HC, Lottenberg L, et al. Elderly injury: a profile of trauma experience in the Sunshine (Retirement) State. J Trauma. Apr 2000;48(4):581-584; discussion 584-586.
- Meldon SW, Reilly M, Drew BL, Mancuso C, Fallon W, Jr. Trauma in the very elderly: a community-based study of outcomes at trauma and nontrauma centers. J Trauma. Jan 2002;52(1):79-84.
- MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. Jan 26 2006;354(4):366-378.
- Nathens AB, Rivara FP, MacKenzie EJ, et al. The impact of an intensivist-model ICU on trauma-related mortality. Ann Surg. Oct 2006;244(4):545-554.
- Eastern Association for the Surgery of Trauma. Pain Management in Blunt Thoracic Trauma (BTT): An Evidence-Based Outcome Evaluation. 2nd Review. http://www.east.org/tpg/painchest.pdf.
- Grant PT, Henry JM, McNaughton GW. The management of elderly blunt trauma victims in Scotland: evidence of ageism? Injury. Sep 2000;31(7):519-528.
- Ma MH, MacKenzie EJ, Alcorta R, Kelen GD. Compliance with prehospital triage protocols for major trauma patients. J Trauma. Jan 1999;46(1):168-175.
- Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma. Oct 2001;51(4):754-756; discussion 756-757.
- Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. Oct 2002;89(10):1319-1322.
- Bergeron E, Clement J, Lavoie A, et al. A simple fall in the elderly: not so simple. J Trauma. Feb 2006;60(2):268-273.
- Pracht EE, Langland-Orban B, Tepas JJ, 3rd, Celso BG, Flint L. Analysis of trends in the Florida Trauma System (1991-2003): changes in mortality after establishment of new centers.Surgery. Jul 2006;140(1):34-43.
- Sharma OP, Oswanski MF, Sharma V, Stringfellow K, Raj SS. An appraisal of trauma in the elderly. Am Surg. Apr 2007;73(4):354-358.
- Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. Aug 2008;143(8):776-781; discussion 782.
- Ivascu FA, Howells GA, Junn FS, Bair HA, Bendick PJ, Janczyk RJ. Rapid warfarin reversal in anticoagulated patients with traumatic intracranial hemorrhage reduces hemorrhage progression and mortality. J Trauma. Nov 2005;59(5):1131-1137; discussion 1137-1139.
- McMillian WD, Rogers FB. Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review. J Trauma. Mar 2009;66(3):942-950.
- Williams TM, Sadjadi J, Harken AH, Victorino GP. The necessity to assess anticoagulation status in elderly injured patients. J Trauma. Oct 2008;65(4):772-776; discussion 776-777.
- Pieracci FM, Eachempati SR, Shou J, Hydo LJ, Barie PS. Degree of anticoagulation, but not warfarin use itself, predicts adverse outcomes after traumatic brain injury in elderly trauma patients. J Trauma. Sep 2007;63(3):525-530.
- Lavoie A, Ratte S, Clas D, et al. Preinjury warfarin use among elderly patients with closed head injuries in a trauma center. J Trauma. Apr 2004;56(4):802-807.
- Karni A, Holtzman R, Bass T, et al. Traumatic head injury in the anticoagulated elderly patient: a lethal combination. Am Surg. Nov 2001;67(11):1098-1100.
- Mina AA, Knipfer JF, Park DY, Bair HA, Howells GA, Bendick PJ. Intracranial complications of preinjury anticoagulation in trauma patients with head injury. J Trauma. Oct 2002;53(4):668-672.
- Epstein CD, Peerless J, Martin J, Malangoni M. Oxygen transport and organ dysfunction in the older trauma patient. Heart Lung. Sep-Oct 2002;31(5):315-326.
- Stewart RM, Park PK, Hunt JP, et al. Less is more: improved outcomes in surgical patients with conservative fluid administration and central venous catheter monitoring. J Am Coll Surg.May 2009;208(5):725-735; discussion 735-727.
- Balogh Z, McKinley BA, Cocanour CS, et al. Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg. Jun 2003;138(6):637-642; discussion 642-633.
- Heyland DK, Cook DJ, King D, Kernerman P, Brun-Buisson C. Maximizing oxygen delivery in critically ill patients: a methodologic appraisal of the evidence. Crit Care Med. Mar 1996;24(3):517-524.
- Davis JW, Kaups KL. Base deficit in the elderly: a marker of severe injury and death. J Trauma.Nov 1998;45(5):873-877.
- Bouras T, Stranjalis G, Korfias S. Head injury mortality in a geriatric population differentiating an “edge” age group with better potential for benefit than older poor-prognosis patients. Journal of NeurotraumaAug2007; 24(8):1355-61.
- Triage. (2010). In Merriam-Webster Online Dictionary. Retrieved May 18, 2010, from http://www.merriam-webster.com/dictionary/triage
- Eastern Association for the Surgery of Trauma (EAST) Ad Hoc Committee on Practice Management Guideline Development. Utilizing Evidence Based Outcome Measures to Develop Practice Management Guidelines: A Primer. 2000.
Tables
|
EVIDENTIARY TABLE: Age as an Indicator for Triage in Geriatric Trauma |
||||
|
First Author |
Year |
Reference |
Data Class |
Notes |
|
Chang DC |
2008 |
Undertriage of elderly trauma patients to state-designated trauma centers.Arch Surg;143(8):776-81; discussion 782. |
II |
Retrospective analysis of 10 ys (1995-2004) of Maryland Ambulance Information System followed by surveys of EMS and trauma centers at regional EMS conferences and Level I trauma centers. Among 26,565 pts, undertriage was significantly higher among those >= 65 yo (49.9% v 17.8%, p < 0.001). On multivariate analysis (cotnrolling for year, sex, physiology, injury, or mechanism, transport reasons, EMS provider level training, presence/absence of specific injuries, and jurisdictional region), age 65 or older (OR: 0.48 [0.3-0.76]). Among surveys, top 3 causal factors: inadequate training, unfamiliarity with protocol, possible age bias. |
|
Mitra B |
2008 |
Management and hospital outcome of the severely head injured elderly patient. ANZ J Surg;78(7):588-92. |
II |
Retrospective review of pt > 64 yp with GCS =< 8 with confirmed intracranial pathology or skull fx over July 2001 to Sept 2005 in the Victoria State Trauma Outcome Registry and Monitoring group. N= 96; 1/3 to each palliation, support without surgery, surgery; overall mort: 70.68% (n= 68); independent predictors of mort: age and brainstem injuries; all pts >= 85 died |
|
Damadi AA |
2008 |
Cervical spine fractures in patients 65 years or older: a 3-year experience at a level I trauma center. J Trauma; 64(3):745-8. |
II |
single institution review of 2000-2003 data, among 58 pts with ICD9 code 805.x 24% died; 7/12 with quad or paraplegia died; mostly treated with rigid collars and halo brace; 18 out of the 45 living at home pre-injury returned home. |
|
Gowing R |
2007 |
Injury patterns and outcomes associated with elderly trauma victims in Kingston, Ontario. Can J Surg;50(6):437-44. |
II |
retrospective chart review of 125 pts > 65 yrs old admitted to academic center in Ontario over 3 yrs with ISS > 12 (total trauma admissions= 460 over 3 yrs); complete data on 99 pts; 32/99 died while in house; 41 pts experienced a total of 97 complications; of pts who suffered complication, 41% died. |
|
Bouras T |
2007 |
Head injury mortality in a geriatric population: differentiating an "edge" age group with better potential for benefit than older poor-prognosis patients. J Neurotrauma;24(8):1355-61. |
II |
Retrospective cohort analysis of 1926 consecutive patients with head injury - patients > 65 yo and 75 yo had incrementally higher mortality than younger cohorts, especially with incrementally lower GCS. Patients > 65 and < 75 yo with GCS 5-8 had a 71% mortality rate, whereas all patients >65 yo with gcs of 3-4 had a 92-94% mortality rate. |
|
Mohindra S |
2008 |
Continuation of poor surgical outcome after elderly brain injury. Surg Neurol;69(5):474-7. |
II |
Retrospective analysis of 45 patients >70 yo treated operatively for head injury were retrospectively analyzed - 1 out of 7 patients with gcs 9-12 had a reasonably favorable outcome, while only 1 out of 33 with gcs 3-8 had a reasonably favorable outcome. |
|
Sharma OP |
2007 |
An appraisal of trauma in the elderly. Am Surg;73(4):354-8. |
II |
Retrospective registry analysis of n=2783 Elderly patients (> 65 yo) and n=45868 younger blunt trauma patients. There was a linear increase in mortality with advanced age and higher ISS. |
|
LeBlanc J |
2006 |
Comparison of functional outcome following acute care in young, middle-aged and elderly patients with traumatic brain injury.Brain Inj;20(8):779-90. |
II |
Retrospective analysis of n-2327 consecutive single-center patients with TBI with comparisons of functional outcome and mortality after TBI stratified for adults>60 and those < 60 yo. In general, the injuries experienced by older patients were similar to those experienced by younger patients and yet were more likely to experience lower FIM and GOSE scores after discharge. |
|
Nathens AB |
2006 |
The impact of an intensivist-model ICU on trauma-related mortality. Ann Surg;244(4):545-54. |
II |
Multicenter analysis on the effect of an intensivist-led ICU on the outcomes of trauma patients. The benefits were most pronounced for elderly trauma patients, ICU's with surgeon-intensivists, and in designated trauma centers. |
|
Yilmaz S |
2006 |
The impact of associated diseases on the etiology, course and mortality in geriatric trauma patients. Eur J Emerg Med;13(5):295-8. |
II |
Single center analysis of 55 consecutive patients >65 yo with ISS>20 comparing outcomes of those < 80 yo and those >80 yo. Patients with COPD were at increased risk for mortality. |
|
Bergeron E |
2006 |
A simple fall in the elderly: Not so simple. J Trauma; 60(2):268-273. |
II |
Compared outcomes in low velocity falls (LVF, defined as fall on same level, fall to the ground from standing or sitting or fall less than 1m) between those greater and less than 65 years old. Found those over 65 had increase length of stay, admission to long-term care facility, and mortality. Done in single Level 1 trauma center in Canada. |
|
Etienne Pracht |
2006 |
Analysis of trends in the Florida Trauma System (1991-2003): Changes in mortality after establishment of new centers.Surgery;140(1):34-43. |
II |
Showed despite increasing the number of trauma centers, elderly were still less likely to be treated at a designated trauma center (DTC). In addition, while hospitalizations for peds went down, adults stayed the same, but elderly increased, and they experienced a strong upward trend in the mortality rate per 1,000 people. Also that more established DTCs did not have a different mortality rate than more recently designated centers, which differed from peds and adults. Elderly also exhibited the smallest increases in the rate of triage to DTCs and were less likely to be transported to a DTC, suggesting undertriage is occurring. |
|
Scheetz LJ |
2003 |
Effectiveness of Prehospital Trauma Triage Guidelines for the Identification of Major Trauma in Elderly Motor Vehicle Crash Victims. J Emerg Nurs;29(2):109-15. |
III |
Prehospital triage systems should include age as a criterion for triage of trauma victims to a trauma center. |
|
Bergeron E |
2003 |
Elderly Trauma Patients with Rib Fractures Are at Greater Risk of Death and Pneumonia. J Trauma;60(2):268-73. |
II |
Elderly patients >65 with rib fractures due to blunt trauma are at increased risk of mortality compared to patients <65. These patients should receive special attention and should probably be observed even for minor trauma, particularly if multiple rib fractures are detected. |
|
Gallager SF |
2003 |
The role of cardiac morbidity in short- and long-term mortality in injured older patients who survive initial resuscitation.Am J Surg; 185(2):131-4. |
III |
Elderly patients who survive initial resuscitation are as likely to survive to discharge as younger patients, but long-term survival is significantly lower as age increases. Cardiac morbidity is predictable using a scoring system and may be useful to develop strategies to prevent the frequency of cardiac complications. |
|
O'Brien DP |
2002 |
Pelvic fracture in the elderly is associated with increased mortality.Surgery;132(4):710-4; discussion 714-5. |
II |
In patients with a pelvic fracture, the only predictor of mortality was age (12.3% age >=55, 2.3% age <55) despite aggressive resuscitation. |
|
Taylor MD |
2002 |
Trauma in the Elderly: Intensive Care Unit Resource Use and Outcome. J Trauma;53(3):407-14. |
II |
Age >65 is associated with a 2 - 3 fold increase in mortality risk in all degrees of trauma compared to age <65. Elderly patients had a significantly longer hospital LOS. Elderly patients with ISS >30 had significantly less ICU LOS due to increased mortality rates. The development of complications (pneumonia, sepsis and renal failure) is associated with worse outcome in elderly trauma victims. Further investigation should target parameters for appropriate triage and treatment protocols to optimize elderly trauma patient outcomes. |
|
Demetriades D |
2002 |
Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg;89(10):1319-22. |
II |
Using age 70 as a trauma team activation criteria and early intensive monitoring, evaluation and resuscitation of geriatric trauma patients improves survival. |
|
Susman M |
2002 |
Traumatic brain injury in the elderly: increased mortality and worse functional outcome at discharge despite lower injury severity.J Trauma;53(2):219-23; discussion 223-4. |
III |
Elderly (65 and over) traumatic brain injury patients have a worse mortality and functional outcome than nonelderly patients who present with head injury even though their head injury and overall injuries are seemingly less severe. Comparisons were made w |
|
Lawes D |
2002 |
A retrospective review of emergency admission for head injury in the over 75s.Injury;33(4):349-51. |
III |
Elderly patients (65 and over) with head injuries rarely require or are suitable for surgical intervention, the majority requiring management of their medical and social problems. This study suggests that elderly patients with head injuries should be assessed |
|
Mosenthal AC |
2002 |
Isolated traumatic brain injury: age is an independent predictor of mortality and early outcome. J Trauma;52(5):907-11. |
III |
The mortality from TBI is higher in the geriatric (65 and over) population at all levels of head injury. In addition, functional outcome at hospital discharge is worse. Although some of this increased mortality may be explained by complications or type of |
|
Albrecht RM |
2002 |
Nonoperative management of blunt splenic injuries: factors influencing success in age >55 years. Am Surg;68(3):227-30; discussion 230-1. |
III |
There were no deaths related to complications from failed nonoperative management. We conclude that nonoperative management of blunt splenic injuries in patients over 55 may be attempted. Patients with higher-grade injuries and pelvic free fluid are at gr |
|
Meldon SW |
2002 |
Trauma in the very elderly: a community-based study of outcomes at trauma and nontrauma centers. J Trauma;52(1):79-84. |
III |
Risk-adjusted outcomes, in this population age 80 and over, differed between TC and AC settings. Head injury, injury severity, and lack of TC verification are associated with hospital mortality in very elderly trauma patients. |
|
Demetriades D |
2001 |
Old age as a criterion for trauma team activation. J Trauma;51(4):754-6; discussion 756-7. |
III |
Sixty-three percent of patients with severe injuries (Injury Severity Score > 15) and 25% of patients with critical injuries (Injury Severity Score > 30) did not have any of the standard hemodynamic criteria for TTA. CONCLUSION: Elderly trauma patients have a high mortality, even with fairly minor or moderately severe injuries. A significant number of elderly patients with severe injuries do not meet the standard criteria for TTA. It is suggested that age > or = 70 years alone should be a criterion for TTA. |
|
Roth BJ |
2001 |
Penetrating trauma in patients older than 55 years: a case-control study. Injury;32(7):551-4. |
III |
Following penetrating trauma, older patients arriving alive and admitted to the hospital are as likely to survive as younger patients who have injuries of similar severity, but at the expense of longer ICU and hospital stays. |
|
Rzepka SG |
2001 |
Geriatric trauma hospitalization in the United States: a population-based study. J Clin Epidemiol;54(6):627-33. |
III |
There were 577,193 geriatric trauma patients admitted to 5227 short-stay U.S. hospitals. Risk of inpatient death increased with age, male gender, black race, and severity of injury. Although demonstrating higher inpatient mortality rates, Level one trauma centers admit a decidedly different patient population than other hospitals, which is disproportionately younger, black and male and includes the most severely injured geriatric patients. |
|
Sterling DA |
2001 |
Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma;50(1):116-9. |
II |
Falls in the elderly (>65) as compared to age <65, have statistically higher ISS score & mortality. AIS scores for head, chest, pelvis/extremity are also statistically higher in the >65 group. These findings held fast when comparing all falls and also "same level" falls |
|
McGwin G |
2001 |
Recurrent trauma in elderly patients.Arch Surg;136(2):197-203. |
II |
Elderly (>70) patients who had experienced trauma are 3.25 times more likely to suffer from a future trauma that elderly who never experienced trauma. Functional limitations in ADL were much more prevalent in the trauma group. |
|
Ferrera PC |
2000 |
Outcomes of admitted geriatric trauma victims. Am J Emerg Med;18(5):575-80. |
II |
Age >65. Low mechanism falls most common. Extremity fx/dislocation most common followed by facial lac, spine fx, hip fx, then CHI. Functional outcomes are possible after traumatic injury. |
|
Alexander JQ |
2000 |
Blunt chest trauma in the elderly patient: how cardiopulmonary disease affects outcome. Am Surg;66(9):855-7. |
II |
Elderly patients (>65) with rib fx are at significant risk for complications including pneumonia and death. Having a h/o cardiac disease compounded this problem significantly with increases in ICU care & overall LOS. |
|
Bulger EM |
2000 |
Rib fractures in the elderly. J Trauma;48(6):1040-6; discussion 1046-7. |
II |
Cohort study rib fx patients of age >65 vs less than 65, looking at differences in morbidity and mortality. Groups had similar AIS and ISS but differed in vent days, ICU and overall LOS. Pneumonia was significantly more common in elderly (31 vs 17%). In elderly group, pneumonia incidence increased with # of rib fx |
|
Tepas JJ |
2000 |
Elderly injury: a profile of trauma experience in the Sunshine (Retirement) State. J Trauma;48(4):581-4; discussion 584-6. |
II |
Review of all 1996 trauma patients in the state of Florida comparing care at trauma centers vs non. Most age >50 are Rxed at non TC. Most common injury is femur fx by fall. TC have significantly less "potentially preventable" deaths than non (23 vs 35% of deaths). Better trauma system management is needed for elderly patients. |
|
McGwin G |
2000 |
Long-term survival in the elderly after trauma. J Trauma;49(3):470-6. |
II |
Elderly (>70) patients s/p trauma have decreased LT survival, especially when initial trauma is followed by a decrease in functional status. |
|
Mann NC |
2001 |
Survival among injured geriatric patients during construction of a statewide trauma system.J Trauma;50:111-116. |
II |
Compared risk-adjusted survival before and after implementation of Washington State trauma system ('88-'92 vs '93-'95) with cox proportional hazard models that assessed survival to 60 days from hospital admission; among 77,136 no difference in survival pre- vs post; among ISS>15, survival increased by 5.1% compared with pre-system years (p=0.03) |
|
Sharma OP |
2008 |
Perils of Rib Fractures. Am Surg; 74(4):310-4. |
III |
Rib fractures were more prevalent and associated with higher mortality in the elderly. Increasing age and number of rib fractures were linearly related to mortality and inversely related to number of patients discharged home. Rib fracture patients, when high risk, should be admitted for observation and treatment. |
|
Camilloni L |
2008 |
Mortality in elderly injured patients: the role of comorbidities.Int J Inj Contr Saf Promot;15(1):25-31. |
III |
In the cohort of elderly injured, chronic conditions are strong determinants of mortality, especially in patients with mild or moderate injuries. Pre-injury conditions should be considered in triage decision making. |
|
Bulger EM |
2000 |
Rib fractures in the elderly. J Trauma;48(6):1040-6; discussion 1046-7. |
II |
Cohort study rib fx patients of age >65 vs less than 65, looking at differences in morbidity and mortality. Groups had similar AIS and ISS but differed in vent days, ICU and overall LOS. Pneumonia was significantly more common in elderly (31 vs 17%). In elderly group, pneumonia incidence increased with # of rib fx |
|
Tepas JJ |
2000 |
Elderly injury: a profile of trauma experience in the Sunshine (Retirement) State. J Trauma;48(4):581-4; discussion 584-6. |
II |
Review of all 1996 trauma patients in the state of Florida comparing care at trauma centers vs non. Most age >50 are Rxed at non TC. Most common injury is femur fx by fall. TC have significantly less "potentially preventable" deaths than non (23 vs 35% of deaths). Better trauma system management is needed for elderly patients. |
|
Ma MH |
1999 |
Compliance with prehospital triage protocols for major trauma patients.J Trauma; 46(1):168-75. |
II |
Retrospective analysis of the state of Maryland's pre-hospital triage criteria adherence to directing trauma center transport. Found that elderly patients with only physiologic signs of injury (not injury or mechanism) were taken to trauma centers less frequently |
|
Grossman MD |
2002 |
When is an Elder Old? Effect of Preexisting Conditions on Mortality in Geriatric Trauma. J Trauma; 52(2): 242-246. |
II |
Large Retrospective Review. 33,781 patients > 65. Found pre-existing conditions were independent predictors of mortality with the strongest association with hepatic, renal and cancer. Interestingly no effect of Coumadin therapy. |
|
Grant PT |
2000 |
The management of elderly blunt trauma victims in Scotland: evidence of ageism? Injury;31(7):519-28. |
II |
Three institution Scottish study, retrospective, looking at outcomes of the elderly. Elderly were less likely to be evaluated in a "resuscitation room" and less likely to be upgraded to a higher level of care hospital when presenting with similar injuries. Mortality was also higher. |
|
MacKenzie EJ |
2006 |
A National Evaluation of the Effect of Trauma Center Care on Mortality.NEJMl; 354:366-378. |
II |
Multicenter analysis on the effect of trauma center care at TC's vs. AC Hospitals in injured patients. Patients>55 years of age were not at risk-adjusted increased risk for mortality compared to those <55 who experienced a significantly decreased risk for mortality. |
|
EVIDENTIARY TABLE: Correction of Coagulopathy in Geriatric Trauma |
||||
|
First Author |
Year |
Reference |
Data Class |
Notes |
|
Ivascu FA |
2008 |
Predictors of mortality in trauma patients with intracranial hemorrhage on preinjury aspirin or clopidogrel. J Trauma;65(4):785-8. |
II |
Retrospective review of single institution trauma registry from 8/1999 to 11/2004; => 50 y/o pts taking ASA, clopidogrel or both with CT documented ICH; among those who died and were taking antiplatelet agent (18%; 20 pts out of 109), demographics and type of agent were not significantly different while gcs and ct grade of hemorrhage predicted outcome. |
|
Williams TM |
2008 |
The necessity to assess anticoagulation status in elderly injured patients.J Trauma;65(4):772-6; discussion 776-7. |
II |
Retrospective review (single institution data from 11/00 to 11/05)) of 1,251 trauma pts aged => 50 y/o with admission INR available (1,988 pts did not have inr available); mort with elevated INR (> 1.5) 22.6% vs 8.2% (P < 0.0001); adjusted for age, gender and ISS, giving adjusted odds of death of 30% for 1 unit increase in INR (OR 1.3 [ 1.1-1.5]; p value 0.002) and 150% increase for INR > 1.5 (OR: 2.5 [1.2-4.2]; p value 0.0014). |
|
Pieracci FM |
2007 |
Degree of anticoagulation, but not warfarin use itself, predicts adverse outcomes after traumatic brain injury in elderly trauma patients.J Trauma; 63(3):525-30. |
II |
Retrospective review (2004-2006) elderly trauma pts (>=65) at Level I TC and had CT of head; divided pts into 3 groups: 1) on warafarin and INR>=2, 2) on warfarin and INR<2, and 3) not on warfarin; 225 pts; therapeutic pts as compared to nonuser had increased likelihood of GCS =< 13 (OR: 5.13 [1.97-13.39]), ICH (OR: 2.59 [0.92-7.32]), overall mortality (OR 4.48 [1.60-12.5]), and morality after ICH (OR: 3.42 [1.09-10.76]); no difference in non-user and non-therapeutic |
|
Hackam DG |
2005 |
Prognostic Implications of Warfarin Cessation After Major Trauma: A Population Based Cohort Analysis.Circulation;111:2250-2256. |
II |
Studied elderly patients in Canada who survived > 6 months after trauma looking at outcomes based on whether they stayed on their coumadin or not. They found no increase in stroke or MI in these patients but did find those who discontinued coumadin were at lower risk for major hemorrhage, but increased risk for venous thromboembolism. |
|
Cohen DB |
2006 |
Traumatic Brain Injury in Anticoagulated Patients. J Trauma;60(3):553-557. |
II |
This was not specifically in the elderly but average age was > 65. Rec all patients on warfarin have an INR (duh), and a CT done in all anticoagulated pts with a GCS < 15 (duh), and those supratherapeutic even with a GCS of 15. Also suggests reversal of supratherapeutic levels and routine repeat CT scans. But this was based on very poor data. They didn't even specifically know if the patients were on coumadin, just that their INR was elevated. |
|
Lavoie A |
2004 |
Preinjury warfarin use among elderly patients with closed head injuries in a trauma center. J Trauma;56(4):802-7. |
II |
Looked at 55 and older. Found warfarin use preinjury associated with higher frequency of isolated head trauma, more severe injury and higher likelihood of death, despite less severe MOI. They don't suggest any specific recommendations (appropriately) but maintain high suspicion. |
|
Mina AA |
2003 |
Complications of preinjury warfarin use in the trauma patient. J Trauma; 54(5):842-7. |
II |
Preinjury warfarin use does not predict mortality. Intracranial hemorrhage on CT scan was a strong predictor of mortality with significantly higher mortality rate in patients on warfarin compared to those with head injury not on warfarin (48% vs 5%). Patients presenting on warfarin with head trauma should be expedited from triage to appropriate evaluation including CT. In the presence of intracranial blood, all efforts to rapidly reverse the warfarin effect with FFP should be undertaken. Reversal is not necessary in the abscess of intracranial bleeding. |
|
Karni A |
2001 |
Traumatic head injury in the anticoagulated elderly patient: a lethal combination.Am Surg; 67(11):1098-100. |
III |
The risk of intracranial hemorrhage with relatively minor head injury is increased dramatically in the anticoagulated patient. A mortality rate of 50 per cent far exceeds the mortality rate in patients with similar head injuries who are not anticoagulated |
|
Kennedy DM |
2000 |
Impact of preinjury warfarin use in elderly trauma patients. J Trauma;48(3):451-3. |
II |
Elderly patients on warfarin before admission to trauma center are not at increased risk for mortality. |
|
Mina AA |
2003 |
Intracranial complications of pre-injury anticoagulation and trauma patients with head injury. J Trauma;53:668-672. |
II |
380 patients at a level I trauma center admitted between 1/97-19/98 who were taking on admission an anticoagulant (warfarin, LMWH, aspirin, NSAID, copidogrel, dipyridamole, pentoxifyilline or naproxen); matched 37 pts with intracranial injury to 37 controls (by age, gender, mechanism, and severity); 4-5 fold higher risk of death in anticoagulated pts |
|
Kirsch MJ |
2004 |
Preinjury Warfarin and geriatric orthopedic trauma patients: a case-matched study. J Trauma;57:1230-1233. |
II |
patients with orthopedic injuries taking warfarin on admission (pts with head injury and pts with INR < 1.5 excluded) admitted to a level I TC from 1/97-6/02; controls matched based on orthopedic injury, need for operation, ISS, age, race, and sex; 53 pts; pts on anticoagulation had increased delay from admission to surgery, hospital LOS, total blood transfusion; no difference in no of ICU days, complications or mortality |
|
Ivascu FA |
2005 |
Rapid Warfarin Reversal in Anticoagulated Patients with Traumatic Intracranial Hemorrhage Reduces Hemorrhage Progression and Mortality. J Trauma;59:1131-7; discussion 1137-9. |
II |
A low threshold for obtaining a head CT in trauma patients on coumadin should be considered. Rapid reversal (within 4 hours) of anticoagulated patients with documented ICH with FFP minimizes the risk of progression and reduces mortality to level of patients not anticoagulated. |
|
Wojcik R |
2001 |
Preinjury Warfirin Does Not Impact Outcome in Trauma Patients. J Trauma;51(6):1147-51; discussion 1151-2. |
II |
Preinjury warfarin use does not adversely impact 28-day mortality, ICU-LOS, Hospital-LOS and functional discharge status in both the head and non-head injured populations. The warfarin cohort was less likely to be discharged to home. |
|
Coimbra R |
2005 |
Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma;59(2):375-82. |
III |
Survey sent to 100 trauma surgeons with questions on habits of coumadin reversal. Reversal strategies & thresholds varied; as did when to restart anticoagulation |
|
Ivascu FA |
2006 |
Treatment of trauma patients with intracranial hemorrhage on preinjury warfarin. J Trauma;61(2):318-21. |
II |
Reviewed a coumadin reveral protocol with a small n post implementation (n=35). Failed to show improved mortality. |
|
McMillan WD |
2009 |
Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: A review. J Trauma;66(3):942-50. |
III |
For anti-platelet limited data suggest increased morbidity and mortality, no guidance on reversal or platelet transfusion. For warfarin data mixed but most feel it is associated with increased mortality. They have a Table 2 summarizing 8 studies. Final recommendations are rapid correction of INR to < 1.6 with FFP (15 mg/kg or approx 4 units) and Vit K IV. |
|
Wong DK |
2008 |
The Effects of Clopidogrel on Elderly Traumatic Brain Injured Patients.J Trauma;65(6): 1303-1308. |
II |
Retrospective review. Only had 131 patients, only 21 on clopidogrel, compared to matched control group. Found increase odds ratio of mortality and discharge to inpatient long-term facility for those on clopidogrel. Mean age was 71.5 years. They didn't show effect of Coumadin since only had 20 patients and none of them died. |
|
Ohn C |
2005 |
Effects of anti-platelet agents on Outcomes for elderly patients with traumatic intracranial hemorrhage. J Trauma; 58(3):518-522. |
II |
Retrospective study 90 patients versus 89 controls. Looked at those taking ASA, clopidogrel or any combination. Small numbers but increased number of deaths in the study patients who also had more co-morbid conditions. |
|
Franko J |
2006 |
Advanced Age and Pre-injury Warfarin Anticoagulation Increase the Risk of Mortality after Head Trauma. J Trauma;61(1):107-110. |
II |
Retrospective review. Only had an n of 159 anticoagulated patients. No surprise found mortality worse for anticoagulated patients and older patient (> 70). Also found mortality increases as INR goes up. Pre-injury warfarin and age predictive of survival. |
|
Gage BF |
2005 |
Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med;118(6):612-7. |
II |
National registry for the "national stroke project". Found that patients with afib, on coumadin, who are falls risk, have higher rates of ICH that non falls risk. Warfarin prescription was associated with intracranial hemorrhage mortality but not with intracranial hemorrhage occurrence. There is still a benefit of anticoag in those with high risk of stroke. |
|
Bouras T |
2007 |
Head injury mortality in a geriatric population differentiating an “edge” age group with better potential for benefit than older poor-prognosis patients. J NeurotraumaAug 2007; 24(8):1355-61 |
II |
Pts 65-74 separated from 75+ in treatment/mortality with GCS<8: 75+ less likely to survive surgical intervention, 65-74 may benefit from ICU/surgical intervention |
|
EVIDENTIARY TABLE: Resuscitation |
||||
|
First Author |
Year |
Reference |
Data Class |
Notes |
|
Belzberg H |
2007 |
Effects of age and obesity on hemodynamics, tissue oxygenation, and outcome after trauma. J Trauma;62(5):1192-200. |
II |
Prospective analysis of 625 trauma patients non-invasively monitored for coetaneous oxygen / CO2 tension, HR, BP, and CI - nonsurvivors and elderly patients had lower DO2 |
|
Jacobs DG |
2003 |
Special considerations in geriatric injury. Curr Opin Crit Care;9:535-539. |
III |
Undertriage to trauma centers in geriatric trauma patients is well documented. Data suggest the standard physiologic and anatomic triage criteria frequently failed to identify the severely injured geriatric trauma patient. The studies did not, however, allow any conclusions to be drawn regarding the true impact of age as a criterion for trauma team activation (the Demetriades papers). They suggested severely injured elderly patients should get a PA catheter (level 2) and be resuscitated to defined endpoints (level 3), but felt the question of whether aggressive hemodynamic management benefits the geriatric trauma patient remains unanswered. |
|
Epstein CD |
2002 |
Oxygen transport and organ dysfunction in the older trauma patient Heart Lung;31(5):315-26. |
III |
Younger patients progressively increase CI and DO2 following multiple trauma; elderly patients begin with low levels that fail to increase. Elderly patients are more vulnerable to poor outcome following major trauma. Age predicted failure of patients to achieve target levels of oxygen transport. |
|
Stewart RM |
2009 |
Less is more: improved outcomes in surgical patients with conservative fluid administration and central venous catheter monitoring.JACS;208(5):725-35; discussion 735-7. |
II |
No difference in survival, perhaps increase in vent free days in conservative fluid group without increased risk for dialysis. |
|
Balogh Z |
2003 |
Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome.Arch Surg;138:637–643. |
II |
Retrospective database analysis demonstrating DIo2 > 500 = more IAH, Comp Syndrome, Death. |
|
Heyland DK |
1996 |
Maximizing oxygen delivery in critically ill patients: a methodological appraisal of the evidence. Crit Care Med;24:517–524. |
II |
Metanalysis of supranormal physiologic goals of increased D02 and VO2 = no survival benefit OR 0.86 (o.6 - 1.2) |
|
Mckinley BA |
2000 |
Blunt Trauma Resuscitation the old can respond. Arch Surg; 135:688-695. |
III |
Elderly can achieve D02 > 500 – 600 |
|
Gallager SF |
2003 |
The role of cardiac morbidity in short- and long-term mortality in injured older patients who survive initial resuscitation.Am J Surg;185(2):131-4. |
III |
Elderly patients who survive initial resuscitation are as likely to survive to discharge as younger patients, but long-term survival is significantly lower as age increases. Cardiac morbidity is predictable using a scoring system and may be useful to develop strategies to prevent the frequency of cardiac complications. |
|
Scalea JM |
1990 |
Geriatric multiple blunt trauma, improved survival with early invasive monitoring. J trauma;30:129-136. |
II |
Pts with ped-motor vehicle mechanism, initial bp < 150, acidosis, multiple fx, and head injury got invasive monitoring; compared pre- and post- years of invasive monitoring; utilizing early invasive monitoring in selected patients has led to decreases in mortality; |
|
Davis JW |
1998 |
Base deficit in the elderly: a marker of severe injury and death. J Trauma;45:873-877. |
II |
Base deficit (<= 6) is a marker of severe injury and significant mortality in all trauma patients, especially patients > 55 years old |
|
Brown CVR |
2003 |
Is Noninvasive Hemodynamic Monitoring Appropriate for the Elderly Critically Injured Patient?J Trauma;58(1):102-7. |
III |
The noninvasive bioimpedance method of obtaining cardiac index correlates with the standard thermodilution technique in elderly critically injured patients. The results are unbiased and may be appropriate to use in clinical decision making. |
Figure