Affordable Care Act on Trauma and Emergency General Surgery - Impact of
Published 2019
Citation: J Trauma. 87(2):491-501, August 2019
Authors
Zerhouni, Yasmin A. MD; Scott, John W. MD, MPH; Ta, Christina BA; Hsu, Paul Chiu-Hsieh PhD; Crandall, Marie MD, MPH; Gale, Stephen C. MD, MBA; Schoenfeld, Andrew J. MD, MSc; Bottiggi, Anthony J. MD; Cornwell, Edward E. III MD; Eastman, Alexander MD, MPH; Davis, Jennifer Knight MD; Joseph, Bellal MD; Robinson, Bryce R. H. MD, MS; Shafi, Shahid MD, MPH, MBA; White, Cassandra Q. MD; Williams, Brian H. MD; Haut, Elliott R. MD, PhD; Haider, Adil H. MD, MPH
Author Information
From the Center for Surgery and Public Health (Y.A.Z., C.T., A.J.S., A.H.H.), Harvard Medical School, Harvard T. Chan School of Public Health, Brigham and Women's Hospital, Boston, Massachusetts; UCSF-East Bay Department of Surgery (Y.A.Z., C.T., A.J.S., A.H.H.), Oakland, California; Harborview Medical Center (J.W.S., B.R.H.R.), University of Washington, Seattle, Washington; Department of Epidemiology and Biostatistics (P.C-H.H.), University of Arizona, Tuscon, Arizona; University of Florida College of Medicine Jacksonville (M.C., S.C.G.), Jacksonville, Florida; UT Health-East Texas (SDG), Tyler, Texas; Department of Orthopaedic Surgery (A.J.S.), Brigham and Women's Hospital, Boston, Massachusetts, University of Kentucky (A.J.B.), Louisville, Kentucky; Howard University (E.E.C.), Washington, D.C.; University of Texas Southwestern, Parkland Memorial Hospital (A.E.), Dallas, Texas; Department of Surgery, West Virginia University (J.K.D.), Morgantown, West Virginia; University of Arizona (B.J.), Tuscon, Arizona; Baylor Scott & White Health (S.S.), Dallas, Texas; Augusta University (C.Q.W.), Augusta, Georgia; Parkland Health & Hospital System (B.H.W.), Dallas, Texas; The Johns Hopkins University School of Medicine and The Johns Hopkins Bloomberg School of Public Health (E.R.H.), Baltimore, Maryland; and Department of Surgery (A.H.H.), Brigham and Women's Hospital, Boston, Massachusetts.
Submitted: September 21, 2018, Revised: March 28, 2019, Accepted: April 7, 2019, Published online: Month May 13, 2019.
Address for reprints: Marie Crandall, MD, 655 W. 8th Street, Jacksonville, FL 32209; email: marie.crandall@jax.ufl.edu.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Online date: July 12, 2019
BACKGROUND Trauma and emergency general surgery (EGS) patients who are uninsured have worse outcomes as compared with insured patients. Partially modeled after the 2006 Massachusetts Healthcare Reform (MHR), the Patient Protection and Affordable Care Act was passed in 2010 with the goal of expanding health insurance coverage, primarily through state-based Medicaid expansion (ME). We evaluated the impact of ME and MHR on outcomes for trauma patients, EGS patients, and trauma systems.
METHODS This study was approved by the Eastern Association for the Surgery of Trauma Guidelines Committee. Using Grading of Recommendations Assessment, Development and Evaluation methodology, we defined three populations of interest (trauma patients, EGS patients, and trauma systems) and identified the critical outcomes (mortality, access to care, change in insurance status, reimbursement, funding). We performed a systematic review of the literature. Random effect meta-analyses and meta-regression analyses were calculated for outcomes with sufficient data.
RESULTS From 4,593 citations, we found 18 studies addressing all seven predefined outcomes of interest for trauma patients, three studies addressing six of seven outcomes for EGS patients, and three studies addressing three of eight outcomes for trauma systems. On meta-analysis, trauma patients were less likely to be uninsured after ME or MHR (odds ratio, 0.49; 95% confidence interval, 0.37–0.66). These coverage expansion policies were not associated with a change in the odds of inpatient mortality for trauma (odds ratio, 0.96; 95% confidence interval, 0.88–1.05). Emergency general surgery patients also experienced a significant insurance coverage gains and no change in inpatient mortality. Insurance expansion was often associated with increased access to postacute care at discharge. The evidence for trauma systems was heterogeneous.
CONCLUSION Given the evidence quality, we conditionally recommend ME/MHR to improve insurance coverage and access to postacute care for trauma and EGS patients. We have no specific recommendation with respect to the impact of ME/MHR on trauma systems. Additional research into these questions is needed.
LEVEL OF EVIDENCE Review, Economic/Decision, level III
Among trauma patients, uninsured status has been associated with increased in-hospital mortality, receipt of less inpatient care, decreased access to postacute care after discharge, and worse long-term functional outcomes.[1–4] Similar associations have been identified among uninsured emergency general surgery (EGS) patients who have higher rates of complications, inpatient mortality, and failure to rescue.[5–7] Insurance coverage is of particular significance for trauma and EGS care in the United States as national estimates suggest that over one in five trauma patients and over one in ten EGS patients lacked health insurance in the latter part of the last decade.[2][5]
In 2010, Congress passed a sweeping national health reform law known as the Patient Protection and Affordable Care Act (ACA).[8] Similar to the 2006 Massachusetts health reform law,[9] the ACA aimed to increase health insurance coverage and reduce health care costs via three strategies: (1) expanding Medicaid eligibility to anyone falling under a particular income level; (2) increased affordability of health insurance through subsidies, newly created insurance markets, and health insurance mandates; and (3) promoting efforts to curb unnecessary costs while improving quality.
Though Medicaid expansion (ME) was initially intended to be rolled out nationally starting in 2014, the Supreme Court ruled in 2012 that each state had the option to expand Medicaid eligibility or not.[10] To date, 37 states (including the District of Columbia) have elected to expand Medicaid, whereas 14 states have not.[11]
In January 2017, the Eastern Association for the Surgery of Trauma (EAST) Board of Directors tasked its Practice Management Guidelines Committee to perform a systematic review to ascertain the impact of the ACA insurance expansion and similar reform efforts on trauma and EGS care to date. Specifically, this review focuses on the impact of both the ACA-related ME as well as the earlier Massachusetts Health Reform (MHR) law given its similarity to this expansion policy.
Objectives
The objective of this review was to evaluate the impact of insurance expansion policies (ME/MHR) on trauma and EGS patient care in the United States. The Population (P), Intervention (I), Comparator (C), and Outcome (O) questions are defined as follows:
- PICO 1: For adult trauma patients, should ME/MHR be enacted versus not be enacted to improve insurance coverage, access to and timeliness of care, hospital discharge disposition, mortality, complications, and cost of care?
- PICO 2: For adult EGS patients, should ME/MHR be enacted versus not be enacted to improve insurance coverage, access to and timeliness of care, hospital discharge disposition, mortality, complications, and cost of care?
- PICO 3: For regional trauma systems, should ME/MHR be enacted versus not be enacted to improve insurance coverage, access to and timeliness of care, hospital discharge disposition, mortality, complications, and cost of care?
Methods
Design
The EAST members formed a writing group to conduct this systematic review. A diverse group of members was recruited to capture representation from different political backgrounds and states with and without ME. Additional EAST members joined the writing team after an open invitation to the membership.
A systematic review was conducted following Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology, as adopted by EAST in 2012.[12] This methodology was used to evaluate the impact of ME and MHR compared with no ME/MHR for trauma patients, EGS patients, and regional trauma systems. Outcomes of interest were generated by the writing group members and then rated on a scale of 1–9 from “outcomes of limited importance” to “critical outcomes” (see Supplemental Digital Content 1, Table A, http://links.lww.com/TA/B400). Critical and important outcomes, those scoring 7 to 9 and 4 to 6 by the writing group respectively, were included in the final PICO questions as outlined above.
Search Strategy
Literature searches were initially performed by the authors with assistance of a medical librarian using PubMed, Cochrane, PsychInfo, CINAHL, Conference Papers Index, EconLit, Evidence Based Medicine Review, and Web of Science to include the dates of January 1, 1990, to June 21, 2017 (Supplemental Digital Content 2, Table B, http://links.lww.com/TA/B401). The search was initially run in Embase for the period January 1, 1990, to June 23, 2017. All queries were later updated on August 24, 2017. Articles that met inclusion criteria reported original research, were specific to ME/MHR, and measured outcomes relevant to trauma or EGS patients or trauma systems. Articles were excluded if they focused on a non-US population, pertained to a medical specialty other than trauma or EGS, or related to other aspects of health care reform other than the specific ME/MHR policies. The study was registered with PROSPERO.[13]
Study Abstraction
For each citation, two reviewers (Y.Z. and C.T.) evaluated the title and abstract to determine whether the citation met inclusion criteria for full-text review. Disagreements were reevaluated and discussed by both reviewers to achieve consensus. Reviewers extracted data per the outcomes of interest and evaluated articles utilizing GRADE methodology for their overall quality of evidence, including assessment of the risk of bias, inconsistency, indirectness, imprecision, and publication bias.[14] Articles were aggregated to assess the impact of ME and MHR on the aforementioned populations of interest.
Analysis
Findings are presented under each individual PICO. Only PICO 1 had sufficient data for conducting meta-analyses on two outcomes of interest among trauma patients: changes in insurance coverage and mortality. For these two outcomes, we performed a random effect meta-analysis to compare the changes in the uninsured rate and the mortality rate, before and after the policy. For each outcome, we derived τ[2], I[2] and H[2] to estimate the amount of total heterogeneity across the published studies. We performed the Q test to evaluate whether there was excessive heterogeneity across the published studies and then generated forest plots to display the results. We used meta-regression to control for mean age, percent of male patients, and Injury Severity Score (ISS) while comparing the mortality rate before and after ME/MHR. All analyses used the “metafor package” in R version 3.1.0 (R Foundation for Statistical Computing, Vienna, Austria). Evidence tables were generated using GRADEpro GDT (McMaster University, Hamilton, Ontario, Canada).
Formulation of Recommendations
All writing group members reviewed the abstracted data, meta-analyses, and meta-regression results and used the following determinants to inform their recommendation: the quality of the evidence, the balance between desirable and undesirable effects, the use of resources, and patients' values and preferences.[12][14] In accordance to EAST review methodology, the writing group members voted from one of the following options: “recommend for,” “conditionally recommend for,” “recommend against,” “conditionally recommend against,” or “no specific recommendation” on ME/MHR. To align with GRADE methodology, the final writing group recommendation required 50% to be in favor with no more than 20% favoring the alternative. At least 70% of the writing group had to vote for a strong recommendation to give a final strong recommendation.
Results
The literature search, after exclusion of duplicated articles, generated 2,027 citations that were reviewed for PICO 1, 436 for PICO 2, and 1539 for PICO 3. Full text evaluations were performed on 176 articles for PICO 1, 11 for PICO 2, and 62 for PICO 3. Ultimately, 18 articles were included in the review for PICO 1, 3 for PICO 2, and 3 for PICO 3 (Supplemental Digital Content 3, Fig. A, http://links.lww.com/TA/B402).
Should ME/MHR be Implemented for Trauma Patients? (PICO 1)
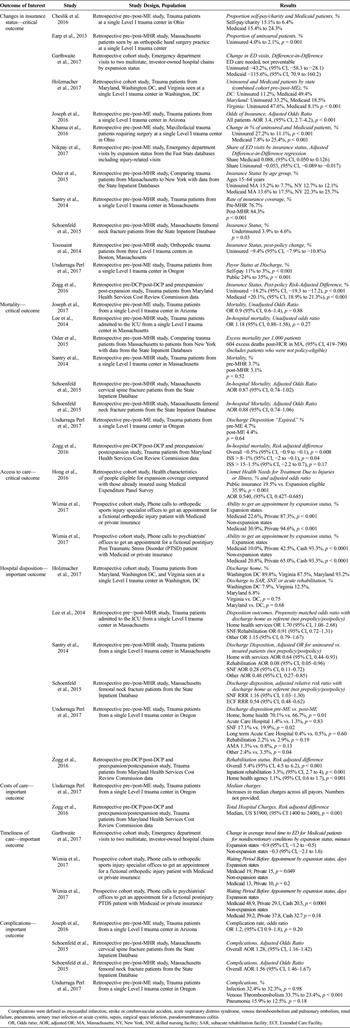
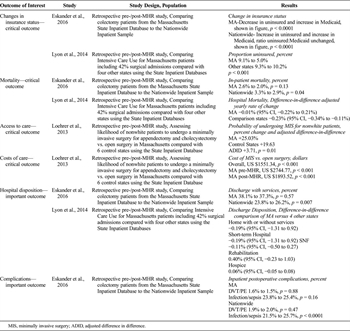
Eighteen studies were identified to answer PICO 1, and they addressed all seven of our predefined outcomes of interest (Table 1).[15–32] Seven studies evaluated the impact of MHR[16][22][24–28] while 11 evaluated the impact of ME.[15][17–20][23][29–32] Sixteen of the studies were retrospective cohort studies,[15–29][32] and two were prospective cohort studies.[30][31]
PICO 1—Insurance Coverage Analysis
A total of 13 studies evaluated changes in the number of uninsured patients and patients with Medicaid[15–18][20][21][23–25][27–29][32]; five examined insurance coverage changes after MHR[16][24][25][27][28] and eight examined ME (Table 1).[15][17][18][20][21][23][29][32] Eight studies reported data from individual trauma centers in ME states, including Massachusetts,[16][25][28] Ohio,[15][21] Arizona,[20] Oregon,[29] and the District of Columbia.[18] Two reported statewide data from Massachusetts[24][27] and one from Maryland.[32] Others were analyses of subnational samples comparing multiple states that opted ME versus those that did not.[17][23]
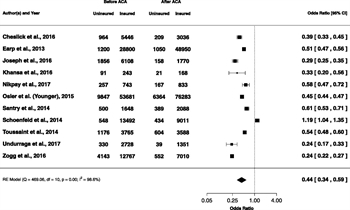
Among the studies included in the random-effects meta-analysis for our outcome of insurance,[15][16][20][21][23–25][27–29] the I[2] was 98.6% and the Q value was 469.06 (p < 0.001), suggesting a high level of heterogeneity between the studies. The odds ratio of being uninsured after ME/MHR was 0.44 (95% confidence interval [CI], 0.34–0.59) (Fig. 1).
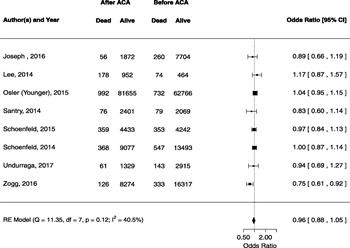
PICO 1—Mortality Analysis
With respect to our analysis related to the effect of ME/MHR on mortality in trauma patients, a total of eight studies were included (Table 1).[20][22][24–27][29][32] Seven of the eight studies did not find a statistically significant reduction in mortality rates after ME/MHR. One study using state-level data from Maryland found a reduction in mortality rate of −0.5% (95% CI −0.9% to −0.1%, p = 0.008) among all trauma patients; however, the finding was no longer statistically significant when the sample was limited to only those patients with ISS greater than 15 (p = 0.1, respectively).[32] Conversely, another study found mixed results, which the authors ultimately did not attribute to MHR policies.[24] For the mortality meta-analysis, the I[2] was 40.5% (95% CI, 0–88.2%) and the Q value was 11.4 (p = 0.12), suggesting a moderate but not significant amount of heterogeneity between the studies. Based on the random-effects meta-analysis, the overall odds ratio of death after implementation of ME/MHR was 0.96 (95% CI, 0.88–1.05) (Fig. 2). In the meta-regression, controlling for mean age, percent of male patients, and mean ISS, the model did not converge.
PICO 1—Additional Outcomes
Three studies of variable quality addressed access to care related to ME (Table 1), and there was insufficient evidence to make a recommendation.[19][30][31] Multiple studies commented on changes in disposition for trauma patients, but aggregation of findings is difficult due to variability in the methods of reporting adjusted outcomes. Overall, findings common to multiple studies included increased discharge to inpatient rehabilitation,[25][32] increased discharge to skill nursing facilities,[25][26][29] increased rate of being discharge home with services,[22][25] and a decreased rate of being discharge home without services.[25][26][29] These findings, however, were not uniformly reported across all studies.
Four studies evaluated complication rates before and after ME and MHR (Table 1), and no statistically significant reductions in complication rates were identified.[20][26][27][29] Interpretation of findings regarding complications was complicated by the lack of adjustment for secular trends impacting the surveillance of complications due to concurrent, and perhaps unrelated, quality control programs during the postpolicy period. Regarding timely access to care as a result of ME, there were few studies that focused on this outcome in the trauma population, and no consistent policy effects were identified.[17][30][31] Only two studies addressed changes in costs of care after implementation of ME among trauma patients, both of which found increases in charges across multiple payers (Table 1).[29][32]
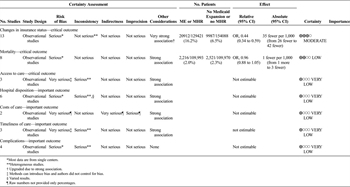
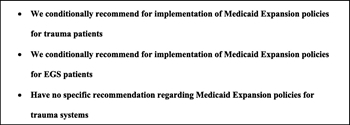
To aid in the development of a recommendation for PICO 1, a GRADE evidence table was compiled (Table 2). All of these articles were limited in that they were observational studies and had heterogeneous methods, therefore, the quality of the data. As such, the rating was initially stated to be “very low.” The meta-analysis findings on changes in insurance status and mortality allowed us to upgrade our rating for those two outcomes to “moderate” and “low,” respectively. After considering the findings of these articles, the quality of the evidence, the risks and benefits of this policy, and the patient preferences, we conditionally recommend for insurance expansion polices, such as ME/MHR for trauma patients.
Should ME/MHR be Implemented for EGS Patients? (PICO 2)
At the time of this review, there were no known studies published evaluating the impact of the 2014 ME on EGS care. However, a total of three articles focused on MHR addressed six of the seven outcomes of interest for PICO 2 (Table 3).[33–35] One study evaluated a cohort of patients undergoing inpatient colectomy, both elective and emergency, before and after MHR.[33] Another study evaluated 259,240 hospital admissions in Massachusetts that included a stay in the intensive care unit (ICU)—83% of which were urgent/emergency admissions and 54% of which were surgical admissions.[35] Finally, a third study evaluated racial/ethnic minority patients undergoing appendectomy or cholecystectomy.[34] All three studies used the Massachusetts State Inpatient Database to study the impact of MHR on the outcomes of interest.
For the change in insurance status, both studies reporting changes in insurance coverage found significant reductions in the uninsured rate after MHR.[33][35] Two studies evaluated for postpolicy changes in mortality and neither study demonstrated a statistically significant change in mortality after MHR[34][35] One study investigated the relationship of MHR and the development of postoperative complications with mixed results.[33] One study evaluating access to care found that MRH was associated with an increased likelihood of receiving laparoscopic (as opposed to open) EGS operations.[34] This change was associated with lower overall inpatient costs (Table 3).[34] Two studies reported hospital disposition related to EGS patients in the setting of MHR, but found no significant differences.[34][35]
After considering the findings of these articles, the quality of the evidence, the risks and benefits of this policy, and the patient preferences, we conditionally recommend for the implementation of policies such as ME/MHR for EGS patients.
Should ME/MHR be Implemented for Regional Trauma Systems? (PICO 3)
Three retrospective studies addressed three of our eight outcomes of interest for PICO 3 (see Supplemental Digital Content 1, Table A, http://links.lww.com/TA/B400).[15][20][36] Two studies used data from their respective Level I trauma centers in Ohio and Arizona, respectively.[15][20] One compared emergency department (ED) closures—without mention of trauma center designation—during the pre-ME period 2006 to 2013 throughout multiple states dichotomized by ME status (see Supplemental Digital Content 1, Table A, http://links.lww.com/TA/B400).[36] Two studies identified fewer charges for uninsured patients and increased charges for Medicaid patients.[15][20] The ultimate impact of these changes on trauma center funding is difficult to interpret as one study noted that total hospital supplemental payments from multiple sources, including Disproportionate Share Hospital payments, decreased after ME[15]; while another study noted that the overall reimbursement rate for the trauma increased after ME.[20]
Given the limited number of studies, variable quality of the evidence, and heterogeneous findings for PICO 3, we have no specific recommendation for ME/MHR compared with no ME/MHR for regional trauma systems.
Discussion
This is the first systematic review to employ the GRADE methodology to evaluate the impact of the most notable health insurance expansion policy in recent history on trauma and EGS patients as well as the regional trauma systems that care for them. Overall, we found that ME and MHR were associated with significant reductions in the uninsured rate for both trauma and EGS patients. However, there were no consistent associations between increased insurance coverage and inpatient outcomes.
For trauma patients, ME and MHR led to large gains in insurance coverage, with many studies demonstrating a decrease of nearly 50% in uninsured rate. Though prior data suggest a strong association between lack of insurance and increased mortality for trauma patients, these ME/MHR-related gains in coverage were not associated with a consistent or significant reduction in inpatient mortality in our meta-analysis. The inpatient mortality odds ratio of 0.96 (Fig. 2) should be interpreted in light of the 95% CI that effectively excludes a reduction in mortality greater than 12% and an increase in mortality greater than 5%. Available data cannot rule out smaller mortality changes which could still be clinically meaningful. It is also possible that increased insurance coverage may lead to a delayed, but not immediate, improvement in clinical outcomes as increased reimbursement may lead to a better financial situation for the hospital and subsequent investments in quality improvement. Finally, it is possible that the well-described association between insurance status and inpatient trauma mortality is a not directly causal, but rather points to a complex interplay of host, prehospital, hospital, or provider factors across the continuum of trauma care.[2]
Notably, the large insurance coverage gains were associated with increased access to postdischarge care for trauma patients,[26][29][32] which is critical to recovery after injury. Prior work has demonstrated that rehabilitation after trauma is associated with improved functional status, improved quality of life, and even decreased mortality at 1 year.[4] Ongoing research regarding the impact of insurance coverage on postdischarge outcomes for trauma is needed to evaluate whether or not insurance coverage protects against short-term or longer-term mortality and long-term disability.
For EGS patients, there are limited data on the impact of ME/MHR on our outcomes of interest. The uninsured rate among EGS patients decreased after MHR; however, there were no robust findings regarding postoperative mortality or complications for patients undergoing EGS procedures. However, given that poor outcomes for EGS patients are mediated by late presentation and unmanaged or unknown comorbidities at presentation,[37] future research should focus on assessing the impact of insurance expansion on timeliness of presentation, management of other comorbidities, and subsequent impact on cost and outcomes for EGS patients. Early analyses of private insurance expansion among young adults through the ACA's 2010 Dependent Coverage Provision are suggestive of earlier care seeking and less complex disease at time of presentation for acute appendicitis.[37] Future work extending these ideas to ME and a wider range of EGS patients is necessary.
Similarly, there were relatively few studies evaluating the impact of ME/MHR on regional trauma systems, and it was not possible to make a definitive recommendation given the heterogeneity of their quality and findings. In general, however, delivering excellent trauma and EGS care is dependent on multiple factors including regional emergency care systems. We did not find any studies that evaluated prehospital care or evaluated state level funding of trauma systems. Single-center data suggest that ME/MHR was associated with increased reimbursement, but that DSH and supplemental payments also decreased. The net impact of these competing financial changes is not yet known. This is especially important as prior work has suggested that nearly two thirds of trauma centers had a negative profit margin on trauma care prior to the ACA.[38] Future research should evaluate the impact of these insurance expansion policies on the entire trauma system, including prehospital, inpatient, and postdischarge care to aid the formulation of future recommendations.
Finally, in addition to evaluating the evidence, GRADE methodology recommends incorporating patient preferences into the final recommendation. There are no current data regarding the preferences of trauma and/or EGS patients toward the ACA. However, as a proxy, the Kaiser Family Foundation has been tracking attitudes toward the ACA and recently found that a majority of respondents had a favorable impression of the ACA and nearly 75% of respondents held a favorable view of Medicaid which they believe is working well for low-income Americans.[39]
Limitations
These findings must be interpreted in light of the study's limitation. First, this systematic review is only a snapshot of the evidence in a quickly evolving field. Medicaid expansion is still a relatively new policy and continues to evolve, thus ongoing analysis will be critically important to evaluate the effects of these policies as more data continues to become available. Second, while we attempted to assemble a writing group from broad political positions and from ME and nonexpansion states, our study is still subject to bias as ME and the ACA remains a controversial topic. However, we aimed to mitigate this potential bias by adhering to the GRADE methodology. Finally, we focused our review on insurance expansion efforts from the 2006 MHR and the 2010 ACA ME policy; however, there are additional insurance expansion efforts that may have a significant impact on trauma and EGS care in the United States. For example, the 2008 Oregon Medicaid health experiment and the 2010 Dependent Coverage Provision have shown that these expansion efforts have impacted access to care, use of preventative health services, improved self-reported health and improved financial security among patients, which may translate into benefits to trauma and EGS patients that were not captured in this systematic review.[37][40][41]
Future Investigations
As there is increasing interest to study the impact of health reform on various patient populations and over a longer time course, we anticipate a growing number of studies on this subject. As individual states continually evaluate their position to enact unique variations of different health reform policies, state-level policy variation can be leveraged to better understand the specific mechanisms which underlie the relationships between insurance coverage and access, quality, and costs of trauma and EGS care in the United States. An important gap in the literature that must be resolved through future work is assessing the impact of insurance expansion on both prehospital care and trauma systems. Rigorous evaluation will be required to best understand which policies have the biggest impact on the care of the acutely ill and injured.
Conclusion
This systematic review is the first known study to offer a meta-analysis of the impact of major insurance expansion policies on trauma and EGS patients. Recent health reform policies have led to large reductions in the uninsured rate among these populations. These insurance coverage gains, however, were not associated with a significant reduction in inpatient mortality, but many studies highlight improved access to valuable postacute care. The quantity and quality of evidence for trauma systems is not currently sufficient to make a recommendation. Given these findings and the quality of the evidence, we conditionally recommend for ME/MHR for trauma and EGS patients (Fig. 3).
References
- Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–949. View Full Text| PubMed| CrossRef
- Haider AH, Weygandt PL, Bentley JM, Monn MF, Rehman KA, Zarzaur BL, Crandall ML, Cornwell EE, Cooper LA. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74(5):1195–1205.
- Sacks GD, Hill CC, Rogers SO Jr. Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care. J Trauma Acute Care Surg. 2011;71(4):1011–1015.
- Nehra D, Nixon ZA, Lengenfelder C, Bulger EM, Cuschieri J, Maier RV. Acute rehabilitation after trauma: does it really matter? J Am Coll Surg. 2016;223(6):755–763. PubMed| CrossRef
- Shah AA, Haider AH, Zogg CK, Schwartz DA, Haut ER, Zafar SN, Schneider EB, Velopulos CG, Shafi S, Zafar H, Efron DT. National estimates of predictors of outcomes for emergency general surgery. J Trauma Acute Care Surg. 2015;78(3):482–490.
- Schwartz DA, Hui X, Schneider EB, Ali MT, Canner JK, Leeper WR, Efron DT, Haut E, Velopulos CG, Pawlik TM, Haider AH. Worse outcomes among uninsured general surgery patients: does the need for an emergency operation explain these disparities? Surgery. 2014;156(2):345–351. View Full Text| PubMed| CrossRef
- Metcalfe D, Castillo-Angeles M, Olufajo OA, Rios-Diaz AJ, Salim A, Haider AH, Havens JM. Failure to rescue and disparities in emergency general surgery. J Surg Res. 2018;231:62–68. PubMed| CrossRef
- Patient Protection and Affordable Care Act, 42 U.S.C. § 18001 (2010).
- Roy A. How Mitt Romney's Health-Care Experts Helped Design Obamacare. Available at https://www.forbes.com/sites/aroy/2011/10/11/how-mitt-romneys-health-care-experts-helped-design-obamacare/#76924a66fb5a. Accessed 15 Jan 2019.
- National Federation of Independent Business v. Sebelius, 567 U.S. 519 (2012).
- Kaiser Family Foundation. Status of State Medicaid Expansion Decisions. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/Accessed 15 Jan 2019.
- Kerwin AJ, Haut ER, Burns JB, et al. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S283–S287.
- PROSPERO International prospective register of systematic reviews. National Institute for Health Research. Available at: https://www.crd.york.ac.uk/prospero/. Published March 26, 2014. Accessed 15 Jan 2019.
- Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B, Raskob G, Lewis SZ, Schünemann H. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians Task Force. Chest. 2006;129(1):174–181. View Full Text| PubMed| CrossRef
- Cheslik TG, Bukkapatnam C, Markert RJ, Dabbs CH, Ekeh AP, McCarthy MC. Initial impact of the affordable care act on an Ohio level 1 trauma center. J Trauma Acute Care Surg. 2016;80(6):1010–1014.
- Earp BE, Louie D, Blazar P. The Impact of Massachusetts Health Care Reform on an Orthopedic Hand Service. J Hand Surg Am. 2013;38(11):2212–2217. PubMed| CrossRef
- Garthwaite C, Gross T, Notowidigdo M, Graves JA. Insurance expansion and hospital emergency department access: evidence from the Affordable Care Act. Ann Intern Med. 2017;166(3):172–179. View Full Text| PubMed| CrossRef
- Holzmacher JL, Townsend K, Seavey C, Gannon S, Schroeder M, Gondek S, Collins L, Amdur RL, Sarani B. Association of expanded Medicaid coverage with hospital length of stay after injury. JAMA Surg. 2017;152(10):960–966. View Full Text| PubMed| CrossRef
- Hong YR, Holcomb D, Bhandari M, Larkin L. Affordable care act: comparison of healthcare indicators among different insurance beneficiaries with new coverage eligibility. BMC Health Serv Res. 2016;16(1):114. PubMed| CrossRef
- Joseph B, Haider AA, Azim A, Kulvatunyou N, Tang A, O'Keeffe T, Latifi R, Green DJ, Friese RS, Rhee P. The impact of patient protection and Affordable Care Act on trauma care: a step in the right direction. J Trauma Acute Care Surg. 2016;81(3):427–434.
- Khansa I, Khansa L, Pearson GD. Professional reimbursements in maxillofacial trauma surgery: effect of the affordable Care Act. Plast Reconstr Surg. 2015;136(4S):138–139. View Full Text| PubMed| CrossRef
- Lee J, Sudarshan M, Kurth T, Kaafarani H, Klein E, Yeh DD, deMoya MA, Eikermann M, Shah K, Velmahos G, Raja AS. Mandatory health care insurance is associated with shorter hospital length of stay among critically injured trauma patients. J Trauma Acute Care Surg. 2014;77(2):298–303.
- Nikpay S, Freedman S, Levy H, Buchmueller T. Effect of the Affordable Care Act Medicaid Expansion on emergency department visits: evidence from state-level emergency department databases. Ann Emerg Med. 2017;70(2):215–225.e216. View Full Text| PubMed| CrossRef
- Osler T, Glance LG, Li W, Buzas JS, Hosmer DW. Survival rates in trauma patients following Health Care Reform in Massachusetts. JAMA Surg. 2015;150(7):609–615. View Full Text| PubMed| CrossRef
- Santry HP, Collins CE, Wiseman JT, Psoinos CM, Flahive JM, Kiefe CI. Rates of insurance for injured patients before and after health care reform in Massachusetts: a possible case of double jeopardy. Am J Public Health. 2014;104(6):1066–1072. View Full Text| PubMed| CrossRef
- Schoenfeld AJ, Wahlquist TC, Bono CM, Lehrich JL, Power RK, Harris MB. Changes in the care of patients with cervical spine fractures following health reform in Massachusetts. Injury. 2015;46(8):1545–1550. PubMed| CrossRef
- Schoenfeld AJ, Weaver MJ, Power RK, Harris MB. Does Health Reform change femoral neck fracture care? A natural experiment in the state of Massachusetts. J Orthop Trauma. 2015;29(11):494–499. View Full Text| PubMed| CrossRef
- Toussaint RJ, Bergeron SG, Weaver MJ, Tornetta P, Vrahas MS, Harris MB. The effect of the Massachusetts Healthcare Reform on the uninsured rate of the orthopaedic trauma population. J Bone Joint Surg Am. 2014;96(16):e141. View Full Text| PubMed| CrossRef
- Undurraga Perl VJ, Dodgion C, Hart K, Ham B, Schreiber M, Martin DT, Zonies D. The Affordable Care Act and its association with length of stay and payer status for trauma patients at a level I trauma center. Am J Surg. 2017;213(5):870–873. PubMed| CrossRef
- Wiznia DH, Maisano J, Kim C-Y, Zaki T, Lee HB, Leslie MP. The effect of insurance type on trauma patient access to psychiatric care under the Affordable Care Act. Gen Hosp Psychiatry. 2017;45:19–24. PubMed| CrossRef
- Wiznia DH, Nwachuku E, Roth A, Kim CY, Save A, Anandasivam NS, Medvecky M, Pelker R. The influence of medical insurance on patient access to orthopaedic surgery sports medicine appointments under the Affordable Care Act. Orthop J Sports Med. 2017;5(7):2325967117714140.
- Zogg CK, Payró Chew F, Scott JW, Wolf LL, Tsai TC, Najjar P, Olufajo OA, Schneider EB, Haut ER, Haider AH, Canner JK. Implications of the patient protection and Affordable Care Act on insurance coverage and rehabilitation use among young adult trauma patients. JAMA Surg. 2016;151(12):e163609. View Full Text| PubMed
- Eskander MF, Bliss LA, McCarthy EP, de Geus SW, Chau Ng S, Nagle D, Rodrigue JR, Tseng JF. Massachusetts Healthcare Reform and trends in emergent colon resection. Dis Colon Rectum. 2016;59(11):1063–1072. View Full Text| PubMed| CrossRef
- Loehrer AP, Song Z, Auchincloss HG, Hutter MM. Massachusetts Health Care Reform and reduced racial disparities in minimally invasive surgery. JAMA Surg. 2013;148(12):1116–1122. View Full Text| PubMed| CrossRef
- Lyon SM, Wunsch H, Asch DA, Carr BG, Kahn JM, Cooke CR. Use of intensive care services and associated hospital mortality after Massachusetts Healthcare Reform*. Crit Care Med. 2014;42(4):763–770. View Full Text| PubMed| CrossRef
- Friedman AB, Owen DD, Perez VE. Trends in hospital emergency department closures nationwide and across Medicaid Expansion, 2006–2013. Am J Emerg Med. 2016;34(7):1262–1264. View Full Text| PubMed| CrossRef
- Scott JW, Rose JA, Tsai TC, Zogg CK, Shrime MG, Sommers BD, Salim A, Haider AH. Impact of ACA insurance coverage expansion on perforated appendix rates among young adults. Med Care. 2016;54(9):818–826. View Full Text| PubMed| CrossRef
- Scott JW, Neiman PU, Najjar PA, Tsai TC, Scott KW, Shrime MG, Cutler DM, Salim A, Haider AH. Potential impact of ACA-related insurance expansion on trauma care reimbursement. J Trauma Acute Care Surg. 2017;82(5):887–895.
- Kaiser Health Tracking Poll—June 2017: ACA, Replacement Plan, and Medicaid. Available at https://www.kff.org/health-reform/poll-finding/kaiser-health-tracking-poll-june-2017-aca-replacement-plan-and-medicaid/Accessed 15 Jan 2019.
- Sommers BD, Gawande AA, Baicker K. Health insurance coverage and health—what the recent evidence tells us. N Engl J Med. 2017;377(6):586–593. View Full Text| PubMed| CrossRef
- Baicker K, Finkelstein A. The effects of Medicaid coverage—learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–685. View Full Text| PubMed| CrossRef
Keywords:
Health care reform; trauma patients; emergency general surgery; trauma systems; practice management guideline