Alcohol-related trauma reinjury prevention with hospital-based screening in adult populations
Published 2020
Citation: J Trauma. 88(1):106-112, January 2020
Visual PMG
Authors
Kodadek, Lisa M. MD; Freeman, Jennifer J. MD; Tiwary, Devesh MD; Drake, Mack Dillon DO; Schroeder, M. Elizabeth MD; Dultz, Linda MD, MPH; White, Cassandra MD; Abdel Aziz, Hiba MD; Crandall, Marie MD, MPH; Como, John J. MD, MPH; Rattan, Rishi MD
Author Information
From the Division of Trauma and Surgical Critical Care (L.M.K.), Vanderbilt University Medical Center, Nashville, Tennessee; General Surgery, Trauma, and Surgical Critical Care (J.J.F.), Texas Health Harris Hospital, Fort Worth, Texas; Central Florida Regional Hospital (D.T.), Sanford, Florida; Trauma and Surgical Critical Care (M.D.D.), Brody School of Medicine at East Carolina University, Greenville, North Carolina; Department of Surgery (M.E.S.), Rutgers-Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Division of General and Acute Care Surgery (L.D.), University of Texas Southwestern Parkland Hospital, Dallas, Texas; Department of Surgery, Trauma and Critical Care (C.W.), Medical College of Georgia at Augusta University, Augusta, Georgia; Department of Surgery (H.A.A.), Hamad General Hospital, Doha, Qatar; College of Medicine (M.C.), University of Florida, Jacksonville, Florida; Department of Surgery (J.J.C.), MetroHealth Medical Center, Cleveland, Ohio; and Department of Surgery (R.R.), University of Miami Miller School of Medicine, Miami, Florida.
Submitted: June 17, 2019, Revised: August 15, 2019, Accepted: August 21, 2019, Published online: September 4, 2019.
This article was presented as a podium presentation during the Guidelines Plenary Session at the Thirty-Second Annual Scientific Assembly of the Eastern Association for the Surgery of Trauma, January 18, 2019 in Austin, Texas.
Address for reprints: Lisa M. Kodadek, MD, Vanderbilt University Medical Center, 1211 21st Ave, South Suite 404, Medical Arts Building Nashville, TN 37212; email: lisa.kodadek@vumc.org; lkodadek@gmail.com.
Online date: September 5, 2019
BACKGROUND
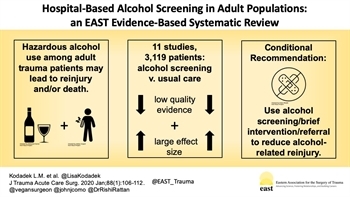
Unaddressed alcohol use among injured patients may result in recurrent injury or death. Many trauma centers incorporate alcohol screening, brief intervention, and referral to treatment for injured patients with alcohol use disorders, but systematic reviews evaluating the impact of these interventions are lacking.
METHODS An evidence-based systematic review was performed to answer the following population, intervention, comparator, outcomes question: Among adult patients presenting for acute injury, should emergency department, trauma center, or hospital-based alcohol screening with brief intervention and/or referral to treatment be instituted compared with usual care to prevent or decrease reinjury, hospital readmission, alcohol-related offenses, and/or alcohol consumption? A librarian-initiated query of PubMed, MEDLINE, and the Cochrane Library was performed. The Grading of Recommendations Assessment, Development and Evaluation methodology was used to assess the quality of the evidence and create recommendations. The study was registered with PROSPERO (registration number CRD42019122333).
RESULTS Eleven studies met criteria for inclusion, with a total of 1,897 patients who underwent hospital-based alcohol screening, brief intervention, and/or referral to treatment for appropriate patients. There was a relative paucity of data, and studies varied considerably in terms of design, interventions, and outcomes of interest. Overall evidence was assessed as low quality, but a large effect size of intervention was present.
CONCLUSION In adult trauma patients, we conditionally recommend emergency department, trauma center, or hospital-based alcohol screening with brief intervention and referral to treatment for appropriate patients in order to reduce alcohol-related reinjury.
LEVEL OF EVIDENCE
Systematic review, Level III.
Nearly 28 million patients with nonfatal injuries are seen annually in emergency departments (EDs) and trauma centers across the United States (US).[1] Injured patients are at high risk for recurrent injury and pose a significant financial burden on the healthcare system, which spends US $80 billion per year for acute care of injured patients.[1][2] Alcohol continues to be a major risk factor for traumatic injuries. Almost 50% of patients seen in Level I trauma centers screen positive for hazardous alcohol use, defined as alcohol use which puts them at risk for future alcohol-related problems.[3] Current literature suggests that alcohol use contributes to 41% of trauma reinjury cases.[4] This public health burden has led organizations such as The American College of Surgeons Committee on Trauma to recommend that all trauma centers incorporate alcohol screening, brief intervention, and referral to treatment (SBIRT) as part of trauma care.[4] Since 2006, the Committee on Trauma has required all trauma centers to have a mechanism to identify patients with hazardous alcohol use; Level I and II centers must provide an intervention by trained staff.[5] This strategy aims to reach a population beyond those with a diagnosis of alcohol dependence; for every one adult in the US who is dependent on alcohol, more than six other adults who are not dependent on alcohol are still at risk of injuring themselves or others from hazardous alcohol use behaviors.[6–8]
The SBIRT begins with screening patients to identify whether a patient's use of alcohol places them and others at risk and therefore warrants a brief intervention. A number of different screening tools are available including Alcohol Use Disorders Identification Test (AUDIT), Michigan Alcoholism Screening Test, and the CAGE questionnaire which is named as an acronym for its four questions about alcohol-related behaviors and feelings (Cut down, Annoyed, Guilty, Eye opener).[8][9] The presence of intoxication at the time of presentation to the hospital may be measured objectively by the weight of alcohol present by blood volume (BAC). Brief intervention for patients who screen positive for hazardous alcohol use may be performed by anyone capable of showing respect and concern for the patient, such as a physician, nurse, or any other staff member; relatively little training is required and may be accomplished with online materials. This intervention typically includes feedback about a patient's hazardous alcohol use as well as a discussion to understand the patient's perspective and encourage behavior change.
While recommendations for SBIRT have been in place for well over a decade, no evidence-based guidelines for routine clinical practice exist.[5] The Eastern Association for the Surgery of Trauma Guidelines Committee Injury Prevention Task Force conducted a systematic review of the literature to assess the impact of SBIRT programs as compared with usual trauma care in terms of preventing or reducing reinjury, readmission, alcohol-related offenses, and alcohol consumption.
Objectives
The objective of this systematic review was to evaluate the preventive efficacy of SBIRT in adult patients treated for injury in the ED, trauma center, or hospital setting. We utilized the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology, which has been previously validated.[10–12] The GRADE approach utilizes a priori creation of questions in the Population, Intervention, Comparator, Outcome (PICO) format. A modified Delphi approach was used to revise the PICO question. Critical outcomes of interest were related to recurrent injury and included incidence of reinjury and hospital readmission. Important outcomes of interest were behavior-related including alcohol-related offenses and alcohol consumption. Given the complex multitude of transnational variables pertaining to hazardous alcohol use including legislation, social and cultural aspects of alcohol consumption, and attribution of injury to behavior, this review's objective was restricted to the US.[13] No funding was obtained for this work. This study was registered with the International Prospective Register of Systematic Reviews (PROSPERO registration number CRD42019122333).
PICO Question
- Population: adult trauma patients
- Intervention: any ED, trauma center, or hospital-based alcohol screening with brief intervention and/or referral to treatment (SBIRT) for appropriate patients
- Comparator: usual trauma care
- Outcomes: reinjury, hospital readmission, alcohol-related offenses, alcohol consumption
Among adult patients presenting for acute injury, should ED, trauma center, or hospital-based SBIRT be instituted compared with usual care to prevent or decrease reinjury, hospital readmission, alcohol-related offenses, and/or alcohol consumption? (PICO 1)
Patients and Methods
Inclusion Criteria for This Review
Study Types
Studies for review included randomized controlled trials (RCTs), prospective and retrospective observational studies, and case-control studies. Case reports and reviews containing no original data or analyses, editorials, letters, and opinion articles were excluded. Studies were limited to those written in English and conducted in the US. No limitations were placed on year of publication.
Participant Types
All relevant studies of adult trauma patients were eligible inclusive of race, ethnicity, sex, and other demographic characteristics.
Intervention Types
All studies evaluating the impact of SBIRT in an ED, trauma center, or hospital setting were included.
Outcome Measure Types
All studies were included if outcomes of interest included reinjury, hospital readmission, alcohol-related offenses, and/or alcohol consumption.
Review Methods
Search Strategy
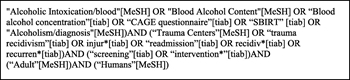
A research librarian aided our systematic search of PubMed, MEDLINE, and the Cochrane Library. After preliminary queries, we chose to apply the following Medical Subject Headings (MeSH) terms: alcoholic intoxication/blood, blood alcohol content, alcoholism/diagnosis, trauma centers, adult, and humans, along with the following title and abstract terms: blood alcohol concentration, CAGE questionnaire, SBIRT, trauma recidivism, injury/injuries, readmission, recidivism/recidivist, recurrent/recurrences, screening, and intervention. Figure 1 contains the string used for the initial search. This systematic search was completed in October 2018. In addition to the electronic search, manual review of bibliographies of articles was led by the lead author (L.M.K.). Four additional studies were identified for inclusion in November 2018 after manual review. In total, 148 abstracts, published between 1986 and 2017, were identified for review.
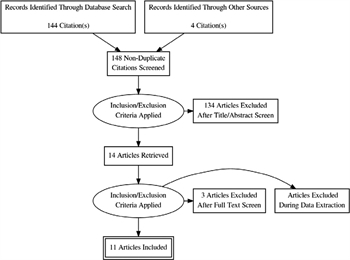
Study Selection
Each of the 148 titles and abstracts was screened by the lead author (L.M.K.) in addition to a second independent reviewer (D.T., M.D., J.F.) using the aforementioned inclusion criteria. Any disagreement was adjudicated by a third GRADE-trained researcher (R.R.) with experience performing systematic reviews. Following title and abstract screen, 14 studies were selected for possible inclusion and full text review. The lead author (L.M.K.) reviewed each full text in addition to a second independent reviewer (D.T., J.F.) A third researcher (R.R.) adjudicated any discrepancies. Three studies were excluded at this stage because, upon further review, they were not conducted in trauma patients in the correct setting, or there was no SBIRT intervention. Eleven studies were included in the evidence-based review.[3][14–23]Figure 2 demonstrates the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram outlining the study selection process.
Data Extraction and Management
All articles, GRADE resources, and instructions were electronically available to all members of the writing team. Each individual reviewer independently assessed the quality of the data gathered through the comprehensive search. Independent interpretations of the data were then shared through group email and conference calls. No major reviewer discrepancies in data interpretation and extraction occurred.
Methodological Quality Assessment
We used the validated GRADE methodology protocol for this study.[10–12] The PICO question was predetermined, and each reviewer independently evaluated the data in aggregate with respect to the quality of the evidence to answer the PICO question. Each individual reviewer graded each article for effect size, risk of bias, inconsistency, indirectness, precision, and publication bias. These independent assessments were then shared with the entire group in an anonymous fashion. Overall recommendations were based on the aggregate quality of the evidence as voted on by the entire group. The GRADE methodology suggests that quality of evidence determine the strength of recommendations; strong recommendations are phrased as “we recommend” and weak recommendations are phrased as “we conditionally recommend.”
Results
Eleven studies were included which provided a total of 3,119 patients comprised of 1,897 patients who received SBIRT and 1,222 patients who received usual trauma care.[3][14–23] After applying validated GRADE methods, the quality of evidence proved too weak to warrant a separate assessment of efficacy for each outcome. There was a relative paucity of data, and studies varied considerably in terms of design, interventions, and outcomes of interest. A qualitative synthesis was performed, but a quantitative meta-analysis was not completed secondary to the heterogeneity of outcomes among the included studies. Overall, the evidence was assessed as low quality, but a large effect size of intervention was present.
All 11 studies included in our synthesis were published in English and were representative of all major geographic areas in the US. With the exception of one study which was completed at two Level I trauma centers, all were single center studies.[17] Ten of the studies were completed at Level I trauma centers and one study was completed at a Level II trauma community hospital.[23] Of the 11 studies, five were RCTs and six were observational studies: one retrospective cohort, one prospective cohort, and four nonrandomized studies. Measured outcomes and frequency of measurement in the identified articles were as follows: alcohol consumption (7), alcohol-related offenses (3), and reinjury/hospital or ED readmission for new injury (3). One study included alcohol abuse/dependence by Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria as an outcome.[14] One study included the proportion of patients who underwent alcohol screening as an outcome following introduction of a screening protocol.[23]
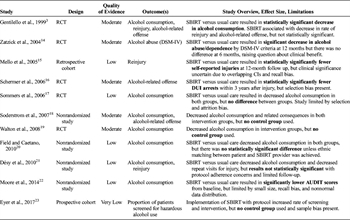
Table 1. Summary of Evidence for Preventive Efficacy of Alcohol Screening, Brief Intervention, and Referral to Treatment for Injured Patients With Alcohol Use Disorders Seen in the ED, Trauma Center, or Hospital Setting.
Seven studies included alcohol consumption as an outcome: two found a statistically significant decrease in alcohol consumption following brief intervention as compared with usual care, one found lower alcohol consumption following brief intervention compared with usual care but results were not statistically significant, and two found lower alcohol consumption in both the control and intervention groups.[3][17–22] Two studies found decreased alcohol consumption in the intervention group, but did not include a control group.[18][19] Three studies reported rates of reinjury or ED/hospital readmission for new injury: all reported lower rates of reinjury for patients receiving brief intervention, but results were only statistically significant in one of the three studies.[3][15][21] Three studies reported rates of alcohol-related offenses: one study found a significant reduction in arrest for driving under the influence of alcohol (DUI) after brief intervention; the remaining two found fewer alcohol-related offenses after intervention but results did not meet statistical significance or had no control group for comparison.[3][16][18] Overall, the evidence was assessed as low quality, but a large effect size of intervention was present. Table 1 provides a summary of the salient findings, effect size, and limitations of each study included in the analysis.
Several studies demonstrated statistically significant evidence to support SBIRT for trauma patients to prevent alcohol-related offenses and alcohol consumption. Gentilello published the largest trial to date among trauma patients admitted to a Level I trauma center.[3] Of 2,524 patients screened in a 2-year period, 46% screened positive for hazardous alcohol use and were randomized to either brief intervention or usual care. At 12-month follow up, patients who received brief intervention had a statistically significant decrease in alcohol consumption compared to the usual care cohort (21.8 versus 6.7 drinks/week reduction; p = 0.03). Schermer performed a prospective RCT including 126 patients injured by motor vehicle collision with a primary outcome measure of DUI arrest.[16] Among patients receiving usual care, 21.9% had a DUI arrest within 3 years of discharge versus 11.3% in the brief intervention group. By multivariate analysis, brief intervention was the strongest protective factor against DUI arrest (odds ratio, 0.32; 95% confidence interval [CI], 0.11–0.96). Moore conducted a study among adult patients diagnosed with mild traumatic brain injury.[22] All participants in the intervention group underwent a battery of tests such as AUDIT and other non–alcohol-related questionnaires. Patients in the intervention group had a significantly lower score on AUDIT at 3 months consistent with reduced hazardous alcohol use (5.2 vs. 9.6 at baseline; p = 0.01) compared with the usual care group.
No studies overtly demonstrated harm or worse outcomes associated with SBIRT for adult trauma patients. However, many studies demonstrated equivocal results that limit our ability to understand the preventive efficacy of SBIRT as it relates to reinjury, hospital readmission, and alcohol consumption/related offenses. Zatzick enrolled and randomly assigned trauma patients to usual care or an intervention including motivational interviews.[14] At 12 months after the injury, statistically significant reductions in alcohol abuse were apparent for patients receiving the intervention versus usual care using DSM-IV criteria; however, at 6 months, no difference was noted, which raises question about the clinical benefit of this intervention. Mello performed a study which randomized trauma patients to standard care or brief ED intervention with or without follow up.[15] Patients who were in a motor vehicle crash group and received brief ED intervention plus follow up had statistically significantly fewer recurrent injuries in comparison to motor vehicle crash patients receiving standard care, however, the CIs overlapped to such an extent that the clinical significance of these results is uncertain (0.35; 95% CI, 0–1.97 vs. 1.14; 95% CI, 0–2.56).
Several studies demonstrated similar findings in both intervention and control cohorts, which suggest that factors other than brief intervention, for example, the injury itself or hospitalization, may contribute to behavior change following injury. Sommers tested the effectiveness of hospital-based brief intervention strategies to reduce alcohol consumption and alcohol-related offenses following alcohol-related vehicular injury.[17] All participants had decreased alcohol consumption and decreased alcohol-related offenses compared with baseline at 1 year after injury. The presence of selection bias (61% refusal rate), attrition bias, and a small sample size limited the quality of these findings. Studies by Soderstrom, Walton, and Eyer lacked a control group, which limits the clinical relevance of the results since the trauma event itself may have caused the change in at-risk behavior.[18][19][23] Of interest, among patients that attributed their injury to their alcohol use, those that received brief intervention had lower consumption of alcohol at 12-month follow up which suggests that assessment of patient's perceptions of their alcohol use may play an important role in determining predictive success of brief interventions.[19] Désy et al.[21] demonstrated no statistically significant difference in rates of reinjury among patients assigned to brief intervention versus usual care. Field showed both treatment as usual or brief intervention resulted in overall decrease in alcohol consumption, but an ethnic match between the patient and SBIRT provider was associated with a statistically significant decrease in alcohol consumption compared with a nonmatch. This study was limited by poor follow-up but demonstrated that culturally tailored interventions in the patient's native language may enhance treatment outcomes.[20]
Recommendations
Among adult patients presenting for acute injury, should ED, trauma center, or hospital-based alcohol screening with brief intervention and/or referral to treatment be instituted compared with usual care to prevent or decrease reinjury, hospital readmission, alcohol-related offenses, and/or alcohol consumption? (PICO 1) Recommendation: In adult trauma patients, we conditionally recommend ED, trauma center, or hospital-based alcohol screening with brief intervention and referral to treatment for appropriate patients in order to reduce alcohol-related reinjury (Fig. 3). This recommendation is based on an overall assessment of the evidence, which was considered low quality, but recognizes a large effect size of intervention.
Discussion
The purpose of this evidence-based review was to assess the quality of literature and make recommendations regarding the preventive efficacy of ED, trauma center, or hospital-based alcohol screening with brief intervention and/or referral to treatment for adult trauma patients. By applying validated GRADE methodology, the quality of evidence proved too weak to warrant assessment of efficacy for each separate outcome. Furthermore, a quantitative analysis could not be performed as the studies included were too heterogenous in terms of design, outcomes, and intervention. However, even with overall low-quality data, a large effect size of intervention was present. Thus, we make a conditional recommendation for ED, trauma center, or hospital-based alcohol screening with brief intervention and referral to treatment for appropriate adult trauma patients. This recommendation is bound by several limitations of the current evidence-based review including bias associated with use of alcohol consumption as a proxy outcome, lack of cost efficacy data, and lack of patient and healthcare provider perceptions concerning feasibility and acceptability.
Alcohol consumption was the most frequently reported outcome and recurrent injury/readmission for new injury was the least frequently reported outcome in the studies included in this review. Injury prevention research often uses proxy outcomes because the most severe consequences of injury—fatalities and injuries producing disability—are less frequent and more difficult to measure than other less important outcomes.[24] Alcohol consumption is a proxy outcome which is more frequent and easily measured than alcohol-related fatalities and injury, but is a less desirable outcome of interest as it relates to injury prevention. Furthermore, alcohol consumption as an injury prevention self-reported outcome is subject to recall bias as well as the Hawthorne effect. Some participants may have inaccurately reported their alcohol consumption if they were aware that this was the study subject of interest and others truly may have changed their alcohol consumption behavior because they were part of a study where this behavior was being measured and reported.
Using These Guidelines in Clinical Practice
In clinical practice, introduction of an SBIRT program requires resources, support from patients, providers, and leadership, as well as training. Resources must be invested to perform alcohol screening and brief interventions in real time at a busy trauma center. Prior work has demonstrated the feasibility of organizing an SBIRT program with a relatively small investment including the efforts of one part-time employee.[25][26] Alcohol screening and brief intervention programs should be implemented in a manner that is both feasible and acceptable to patients and healthcare providers. Most patients (94%) feel that a member of the trauma team should speak with them about alcohol use if they are hospitalized in a trauma unit.[26] Most surgeons (88%) support alcohol screening for injured patients and brief interventions (72%) for those identified as having hazardous alcohol use.[25] Providers may be concerned about the implications of SBIRT on possible reimbursement for services. A survey of 383 trauma surgeon members of the American Association for the Surgery of Trauma and the Western Trauma Association reported that 27% of surgeons perceive alcohol screening to be a threat to reimbursement.[27] At least 38 of the 50 states have statutes in place which may allow insurance carriers to deny payment for medical bills associated with injuries sustained while intoxicated or under the influence of illegal substances.[28] Trauma centers may find that screening with patient-reported questionnaires such as AUDIT or CAGE may mitigate reimbursement concerns associated with measuring BAC at time of admission. The Centers for Medicaid and Medicare Services, however, has recognized the merit of intervention programs and created a specific billing code to enable reimbursement.[29] One barrier to implementation may be the lack of training for surgeons concerning the various alcohol screening tools available. However, trauma surgeons can be taught the cognitive skills needed to screen patients for hazardous alcohol use and provide brief interventions.[30] Multidisciplinary partnership may also be an effective strategy since social workers, addiction medicine specialists, and other staff may also be prepared to offer brief intervention and treatment resources.
Future Directions
Hazardous alcohol use is common among patients presenting for acute care after injury. Further research efforts are needed to understand the most efficacious methods for prevention of recurrent alcohol-related injury. Furthermore, efforts must also focus on primary prevention strategies for patients with hazardous drinking behaviors. No cost-efficacy analyses were included in the studies reviewed and this represents a significant limitation. Implementation of an SBIRT program requires not only support from providers and patients, but also training, staff, and infrastructure. The cost of implementation is unknown nor is the impact on reimbursements fully recognized. Future research should focus on the cost-benefit of SBIRT in terms of prevention of trauma reinjury.
Conclusion
Alcohol use among injured patients may result in recurrent injury or death. In adult trauma patients, we conditionally recommend ED, trauma center, or hospital-based alcohol screening with brief intervention and referral to treatment for appropriate patients in order to reduce alcohol-related reinjury. However, further research is needed to understand the impact and preventive efficacy of SBIRT, as well as resource allocation, feasibility, and acceptability of this injury prevention strategy.
Authorship
Each of the authors listed fulfilled authorship criteria by participating in analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, and giving final approval of the version to be published. R.R., J.J.C., M.C. and L.M.K. were responsible for study design. R.R. provided expertise in GRADE methodology as well as overall supervision of the study. L.M.K. collected data, facilitated the GRADE process, and drafted the article. All authors contributed substantially to the revision of the article. All authors take full responsibility for the article as a whole.
Disclosure
No industry or pharmaceutical support was received for this work. The authors report no financial conflicts of interest pertaining to this work.
No funding was obtained for this systematic review.
References
- National Center for Injury Prevention and Control. CDC Acute Injury Care Research Agenda: Guiding Research for the Future. Atlanta (GA): Centers for Disease Control and Prevention; 2005.
- McCoy AM, Como JJ, Greene G, Laskey SL, Claridge JA. A novel prospective approach to evaluate trauma recidivism: the concept of the past trauma history. J Trauma Acute Care Surg. 2013;75:116–121.
- Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, Villaveces A, Copass M, Ries RR. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230(4):473–480. View Full Text | PubMed | CrossRef
- Nunn J, Erdogan M, Green RS. The prevalence of alcohol-related trauma recidivism: a systematic review. Injury. 2016;47(3):551–558. PubMed | CrossRef
- Resources for Optimal Care of the Injured Patient, American College of Surgeons, 2014, Available at: https://www.facs.org/~/media/files/quality%20programs/trauma/vrc%20resources/resources%20for%20optimal%20care.ashx, Accessed March 24, 2019.
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. PubMed | CrossRef
- Dawson DA, Grant BF, Stinson FS, Chou PS. Toward the attainment of low-risk drinking goals: a 10-year Progress report. Alcohol Clin Exp Res. 2004;28:1371–1378. View Full Text | PubMed | CrossRef
- Alcohol Screening and Brief Intervention (SBI) for Trauma Patients. American College of Surgeons Committee on Trauma. Available at: https://www.facs.org/~/media/files/quality%20programs/trauma/publications/sbirtguide.ashx. Accessed June 15, 2018.
- Maisto SA, Connors GJ, Allen JP. Contrasting self-report screens for alcohol problems: a review. Alcohol Clin Exp Res. 1995;19(6):1510–1516. PubMed | CrossRef
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJGRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. View Full Text | PubMed | CrossRef
- Jaeschke R, Guyatt GH, Dellinger P, Schünemann H, Levy MM, Kunz R, Norris S, Bion JGRADE Working Group. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008;337:a744. PubMed | CrossRef
- Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, Stassen N, Dahm PEastern Association for the Surgery of Trauma Practice Management Guidelines Ad Hoc Committee. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73(5 suppl 4):S283–S287.
- Affinati S, Patton D, Hansen L, Ranney M, Christmas AB, Violano P, Sodhi A, Robinson B, Crandall Mfrom the Eastern Association for the Surgery of Trauma Injury Control and Violence Prevention Section and Guidelines Section. Hospital-based violence intervention programs targeting adult populations: an Eastern Association for the Surgery of Trauma evidence-based review. Trauma Surg Acute Care Open. 2016;1:1–7.
- Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, Dunn C, Jurkovich G, Uehara E, Katon W. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry. 2004;61:498–506. View Full Text | PubMed | CrossRef
- Mello MJ, Nirenberg TD, Longabaugh R, Woolard R, Minugh A, Becker B, Baird J, Stein L. Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Ann Emerg Med. 2005;45:620–625. View Full Text | PubMed | CrossRef
- Schermer CR, Moyers TB, Miller WR, Bloomfield LA. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. J Trauma. 2006;60:29–34. View Full Text | PubMed | CrossRef
- Sommers MS, Dyehouse JM, Howe SR, Fleming M, Fargo JD, Schafer JC. Effectiveness of brief interventions after alcohol-related vehicular injury: a randomized controlled trial. J Trauma. 2006;61:523–533. View Full Text | PubMed | CrossRef
- Soderstrom CA, DiClemente CC, Dischinger PC, Hebel JR, McDuff DR, Auman KM, Kufera JA. A controlled trial of brief intervention versus brief advice for at-risk drinking trauma center patients. J Trauma. 2007;62:1102–1112. View Full Text | PubMed | CrossRef
- Walton MA, Goldstein AL, Chermack ST, McCammon RJ, Cunningham RM, Barry KL, Blow FC. Brief alcohol intervention in the emergency department: moderators of effectiveness. J Stud Alcohol Drugs. 2008;69(4):550–560. PubMed | CrossRef
- Field C, Caetano R. The role of ethnic matching between patient and provider on the effectiveness of brief alcohol interventions with Hispanics. Alcohol Clin Exp Res. 2010;34(2):262–271. View Full Text | PubMed | CrossRef
- Désy PM, Howard PK, Perhats C, Li S. Alcohol screening, brief intervention, and referral to treatment conducted by emergency nurses: an impact evaluation. J Emerg Nurs. 2010;36(6):538–545. View Full Text | PubMed | CrossRef
- Moore M, Winkelman A, Kwong S, Segal SP, Manley GT, Shumway M. The emergency department social work intervention for mild traumatic brain injury (SWIFT-acute): a pilot study. Brain Inj. 2014;28(4):448–455. PubMed | CrossRef
- Eyer MM, Renier CM, Woehrle TA, Vogel LE, Conway PG, McCarty CA. Alcohol use at the time of traumatic brain injury: screening and brief intervention in a community hospital. J Trauma Nurs. 2017;24(2):116–124. View Full Text | PubMed | CrossRef
- Maier RV, Mock C. Chapter 3 Injury Prevention. In: Mattox KL, Feliciano DV, Moore EE, eds. Trauma Seventh Edition. New York: Appleton & Lange:36–53.
- Schermer CR. Feasibility of alcohol screening and brief intervention. J Trauma. 2005;59:S119–S123. View Full Text | PubMed | CrossRef
- Schermer CR, Bloomfield LA, Lu SW, Demarest GB. Trauma patient willingness to participate in alcohol screening and intervention. J Trauma. 2003;54:701–706. View Full Text | PubMed | CrossRef
- Schermer CR, Gentilello LM, Hoyt DB, Moore EE, Moore JB, Rozycki GS, Feliciano DV. National Survey of Trauma Surgeons' use of alcohol screening and brief intervention. J Trauma. 2003;55:849–456. View Full Text | PubMed | CrossRef
- Rivara FP, Tollefson S, Tesh E, Gentilello LM. Screening trauma patients for alcohol problems: are insurance companies barriers? J Trauma. 2000;48:115–118. View Full Text | PubMed | CrossRef
- Screening, Brief Intervention, and Referral to Treatment (SBIRT) Services, Centers for Medicaid and Medicare Services. Available at: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/SBIRT_Factsheet_ICN904084.pdf, accessed 25 March 2019.
- Danielsson PE, Rivara FP, Gentilello LM, Maier RV. Reasons why trauma surgeons fail to screen for alcohol problems. Arch Surg. 1999;134:564–568. View Full Text | PubMed | CrossRef
Keywords:
Injury prevention; trauma; alcohol screening; SBIRT; guideline; evidence-based medicine