Colonic Obstruction Surgery or Stenting
Published 2016
Citation: J Trauma. 80(4):659–664, April 2016
Authors
Ferrada, Paula MD; Patel, Mayur B. MD, MPH; Poylin, Vitaliy MD; Bruns, Brandon R. MD; Leichtle, Stefan W. MD; Wydo, Salina MD; Sultan, Shahnaz MD; Haut, Elliott R. MD, PhD; Robinson, Bryce MD, MS
Author Information
From the Virginia Commonwealth University (P.F.), Richmond Virginia; Vanderbilt University Medical Center, Departments of Surgery and Neurosurgery; Nashville VA Medical Center, Tennessee Valley Healthcare System (M.B.P.), Nashville, Tennessee; Beth Israel Deaconess Medical Center (V.P.), Boston Massachusetts; Division of Acute Care Surgery, University of Maryland Medical Center (B.R.B.); and Johns Hopkins (E.R.H.), University Bloomberg School of Public Health, Baltimore, Maryland; LAC+USC Medical Center (S.W.L.), University of Southern California, Los Angeles, California; Cooper University Hospital (S.W.), Philadelphia, Pennsylvania; University of Florida (S.S.), Gainesville, Florida; and University of Washington (B.R.), Harborview Medical Center, Seattle, Washington.
Submitted: December 11, 2015, Accepted: December 16, 2015, Published online: January 21, 2016.
Address for reprints: Paula Ferrada, MD, 1 VCU Surgery Trauma, Critical Care and Emergency Surgery, PO Box 980454, West Hospital, 15th Floor, East Wing 1200 E Broad St, Richmond, VA 23298; email: pferrada@mcvh-vcu.edu.
Objectives
Our Population, Intervention, Comparator, and Outcome (PICO) questions are defined as follows:
- Population: initial therapy in adult patients with colonic obstruction (malignant or benign).
- Intervention: surgery.
- Comparator: endoscopic stenting.
- Outcomes: mortality and complications resulting in emergency unplanned procedure.
- PICO Question 1: In adult patients with colonic obstruction (malignant or benign) (P), should surgery (I) or endoscopic stenting (C) be performed to decrease mortality (O)?
- PICO Question 2: In adult patients with colonic obstruction (malignant or benign) (P), should surgery (I) or endoscopic stenting (C) be performed to decrease emergency, nonplanned procedures (O)?
Patients and Methods
Study Eligibility
Inclusion criteria consisted of articles published in the English language reporting adult patients 18 years or older, who required hospitalization for the management of colonic obstruction with surgery or endoscopic stenting. We excluded meta-analyses, case reports, letters, and reviews lacking original data.
Intervention and Comparators
We only included studies directly comparing stenting with emergency, nonplanned surgery.
Critical Outcome
As per GRADE methodology, outcomes were chosen by the team and rated in importance from 1 to 9, with scores of 7 to 9 representing critical outcomes after intervention for colonic obstruction. The critical outcome was mortality, rated a score of 9.
Secondary Outcome
Emergency, nonplanned procedures were selected as a secondary outcome because of a rated score of 7. Other outcomes considered but excluded were renal failure, length of stay, and hospital cost because of ratings of lower than 7.
Information Sources
Two professional librarians conducted a systematic search using the , EMBASE, and the Cochrane Library databases of published studies. The search was last run on January 2, 2015, and used the following Medical Subject Headings (MeSH) terms: ((“Stents”[Mesh] OR stent*[tiab]) OR (“surgery”[tiab] OR surgical*[tiab] OR “surgery” [Subheading:NoExp] OR “Digestive System Surgical Procedures”[Mesh])) AND ((“Colon”[Majr] OR “colon”[tiab] OR “colonic”[tiab]) AND (“Intestinal Obstruction”[Mesh:NoExp] OR obstruct*[tiab])) AND (“mortality” [Subheading] OR “mortality”[tiab] OR death*[tiab] OR survival[tiab]) AND (“Comparative Study” [Publication Type] OR compare*[tiab] OR compari*[tiab]). In addition to the electronic search, we hand-searched the bibliographies of recent reviews and articles accepted for this study and reviewed the ClinicalTrials.gov registry. All studies found from 1990 until the last date of the search were considered. The last search was performed in January 2015.
Selection of Studies
After completing the electronic literature search, two independent reviewers screened titles and abstracts, applying the a priori PICO inclusion criteria. Any disagreement on inclusion was resolved by consensus. The resulting studies then underwent full-text review, again by two independent reviewers, to determine appropriateness for inclusion.
Data Extraction and Management
Two independent reviewers extracted the desired variables from the studies into Microsoft Excel. For two meta-analyses, we used Review Manager X.6 (RevMan a program developed for The Cochrane Collaboration to assist authors in preparing Cochrane reviews for publication in The Cochrane Database of Systematic Reviews).
Measures of Treatment Effect
We reported the dichotomous outcomes of mortality and need for emergency, nonplanned operation as an odds ratio, with associated 95% confidence intervals and p values. The unit of analysis was individual patients.
Assessment of Heterogeneity
Potential heterogeneity exists because of population differences, different types of surgery performed, and how obstruction was defined. We examined these differences across studies to assess the clinical and methodological heterogeneity. For the meta-analyses, we used RevMan to calculate the Q statistic, and then, the I2 statistic (%) was used to determine the proportion of variation between studies attributable to heterogeneity and categorized as low (25–49%), moderate (50–74%), or high (74–100%). We also used the χ2 test for heterogeneity and examined the confidence intervals for overlap, with decreasing overlap representing increasing heterogeneity. If heterogeneity was moderate to high, we did not consider pooling the data to be appropriate, and we performed a qualitative narrative summary of results. Based on the methodological and clinical similarity, we performed meta-analysis for each outcome.
Results
Qualitative Analysis
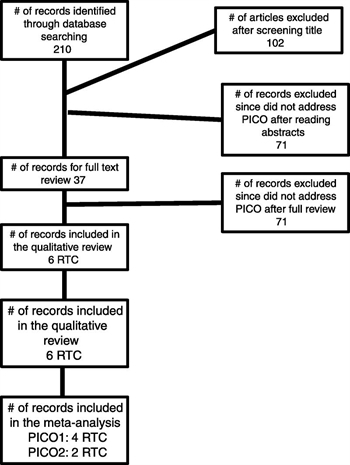
Figure 1. CONSORT diagram detailing the search and included articles in the review.
Initially, the search yielded 210 studies. Title-only review excluded 102 articles. Abstract review excluded another 71 articles, leaving 37 articles for full-text review. Of those 37 articles, 6 were randomized controlled trials (RCTs). These RCTs were included in the final qualitative review[8–13] (Fig. 1, CONSORT diagram). We were unable to find literature that addressed stent use in benign disease; however, we included two articles focusing on benign disease for the qualitative review.[3][14]
Four RCTs compared mortality between the two interventions, representing a total of 206 patients, where 94 were treated with operation and 112 were treated with endoscopic stenting. None of the articles addressed timing of intervention or benign disease indications.
Finally, we identified four studies that were appropriate for quantitative synthesis for PICO Question 1[8][11–13] and two studies for PICO Question 2[8][11] (Fig. 2).
Results Obtained for PICO Question 1
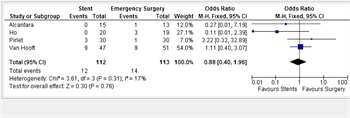
Figure 2. Forest plot for PICO Question 1.
PICO Question 1: In adult patients with colonic obstruction (malignant or benign) (P), should surgery (I) or endoscopic stenting (C) be performed to decrease mortality (O)?
Our search yielded no results addressing mortality regarding the use of stents versus emergency, nonplanned surgery for benign disease. Four RCTs compared mortality between the two interventions.[8][11–13] Alcantara et al.[8] have shown no statistically significant difference in mortality between the two groups; in their trial, there were no deaths in the stent group, and there was one death in the patients who received emergency surgery;[8] however, this was a small sample (stent, 15; surgery, 13). Van Hooft et al.[13] had a larger sample size (stent with 47 vs. surgery with 51) without a difference in mortality being detected (30-day mortality, five patients in each group). Ho et al.[11]reported an 18% increase in mortality in the emergency surgery group (three patients died in the surgery group vs. none in the patients who received a stent). Pirlet et al.[12] reported four in-hospital deaths during their study period. One patient in the surgery group died on the same day of surgery as a consequence of end-organ failure, and three patients died in the stent group as a result of the procedure (one from rapid progression of his neoplastic illness, one from mesenteric infarction, and one from septic shock and multivisceral failure after anastomotic leakage). A total of 32 patients underwent emergency surgery, and 35 received a stent in this trial. In all the RCTs, implicit is that colonic obstruction is a surgical emergency that requires prompt treatment and decompression. None of the articles addressed increased mortality by delayed therapy, either in stenting or emergency, nonplanned surgery since prompt treatment before perforation is considered in all studies as the standard of care.
Quantitative Analysis (Meta-analysis)
Comparisons between the use of stents and emergency, nonplanned surgery evaluating mortality as an outcome were found in four RCTs. Analysis of the pooled data revealed that colonic stenting trended lower mortality rates than emergency, unplanned surgery (Fig. 2). However, a mild amount of heterogeneity was found (I2 = 17%).
Results Obtained for PICO Question 2
In adult patients with colonic obstruction (malignant or benign) (P), should surgery (I) or endoscopic stenting (C) be performed to decrease emergency, nonplanned procedures (O)?
Qualitative Analysis
Regarding benign disease, two articles mentioned morbidity after stenting or surgery.[3][14] Köhler et al.[14] described their experience with stenting strictures secondary to inflammatory bowel disease but without mentioning strictures for diverticulitis. Immediate surgery was required in three patients secondary to perforation with stent placement, 11 patients had elective surgery after stent placement because of stent dislocation or recurrent stenosis, and 6 patients had successful placement without need for surgery.[14] This article described a series of 14 patients with anastomotic stricture, of which 9 had long-term cure with stenting. This article did not compare emergency, nonplanned surgery versus stenting for begin disease but merely described the authors’ experience with stenting. Small et al.[3] described successful stent placement in 23 patients with benign disease. In this series, complications occurred in 38% of the patients including migration (n = 2), reobstruction (n = 4), and perforation (n = 2). Of these major complications, 87% occurred after 7 days. Fifteen of these patients had diverticulitis as the main reason for obstruction, two patients had strictures secondary to radiation, three patients had anastomotic strictures, two had an inflammatory stricture (etiology unknown), and one patient had Crohn’s disease. This article also failed to compare emergency, nonplanned surgery with stents.
Two RCTs compared emergency, nonplanned procedures or reoperation in patients with acute colonic obstruction but only included malignant disease.[8][11] Alcantara et al.[8] showed a statistically significant difference between the stent and emergency surgery group, favoring stent placement (reoperation stent, 0 of 15; emergency surgery, 4 of 13), while Ho et al.[11] failed to support this finding (stent with 2 of 20 vs. emergency surgery with 2 of 19). However, in this study, overall complication rates were higher in the emergency surgery group (stent, 305 vs. emergency surgery, 58%). All RCTs assumed that colonic obstruction is a surgical emergency that requires prompt treatment. None of the articles addressed increased nonplanned operative interventions by delayed therapy, either in stenting or in emergency surgery.
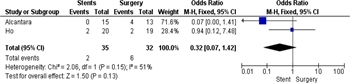
Figure 3. Forest plot for PICO Question 2.
Quantitative Analysis (Meta-analysis)
Comparisons between the use of stents and emergency surgery evaluating the necessity for reoperation or unplanned procedures as an outcome were found in two RCTs (please include the references). Analysis of the pooled data revealed that colonic stenting trended lower rates of unplanned procedures or reoperation compared with emergency surgery (Fig. 3). However, heterogeneity was at a moderate level (I2 = 51%).
Grading the Evidence
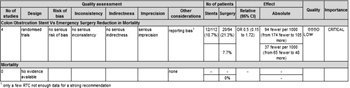
Figure 4. GRADE evidence table for PICO Question 1.
Applying the GRADE framework to the outcome of reduced mortality rates and for unplanned procedures or reoperations found no serious risk of bias, inconsistency, indirectness, or publication bias. However, studies comparing the rate of mortality for stent use versus surgery in patients with colonic obstruction included patients with only a malignant etiology for obstruction. No articles compared these techniques as applied to benign disease. All included studies were RCTs; however, the overall quality of evidence was downgraded to low secondary to the small number of studies fulfilling criteria, serious imprecision, and the large variation in outcomes. (Figs. 4 and 5, Evidence GRADE Profiles).
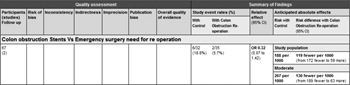
Figure 5. GRADE evidence table for PICO Question 2.
Recommendations
PICO Question 1: In adult patients with colonic obstruction (malignant or benign) (P), should surgery (I) or endoscopic stenting (C) be performed to decrease mortality (O)?
PICO Question 2: In adult patients with colonic obstruction (malignant or benign) (P), should surgery (I) or endoscopic stenting (C) be performed to decrease emergency, nonplanned procedures (O)?
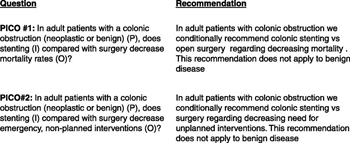
Figure 6. Summary of recommendations.
We conditionally recommend endoscopic, colonic stenting (if available) as the initial therapy for colonic obstruction. In our review, stent use was associated with decreased mortality and rates for emergency, nonplanned procedures to include reoperations. This conditional recommendation is limited to those with malignancy because of the lack of literature supporting this practice in benign colonic disease. Moreover, our review supports expedient intervention when the diagnosis of colonic obstruction is made because of the high complication and mortality rates associated with ischemic perforation (Fig. 6).
Authorship
P.F., M.B.P., V.Y.P., B.B., S.L., and S.W. reviewed the articles in detail and extracted the data initially. P.F. extracted the data individually and produced the forest plots independently. P.F., M.B.P., V.Y.P., B.B., S.L., S.W., S.S., and E.H. voted on the outcomes and recommendations and participated in the writing and critical correction of the manuscript. Finally, B.R. reviewed the manuscript and data, provided critical review of the writing, performed statistical review, and provided recommendations.
Acknowledgment
We thank Karen H. Gau and Barbara A Wright, two professional research and education librarians, for performing the search using the MeSH terms independently and for subsequently refining the search as well as helping to screen the articles. MBP was supported by the Vanderbilt Faculty Scholars Program.
Disclosure
The authors declare no conflicts of interest.
References
- Tekkis PP, Kinsman R, Thompson MR, Stamatakis JD. The Association of Coloproctology of Great Britain and Ireland study of large bowel obstruction caused by colorectal cancer. Ann Surg. 2004; 240: 76–81.
- Leitman IM, Sullivan JD, Brams D, DeCosse JJ. Multivariate analysis of morbidity and mortality from the initial surgical management of obstructing carcinoma of the colon. Surg Gynecol Obstet. 1992; 174: 513–518.
- Small AJ, Young-Fadok TM, Baron TH. Expandable metal stent placement for benign colorectal obstruction: outcomes for 23 cases. Surg Endosc. 2008; 22: 454–462.
- Kim JS, Hur H, Min BS, Sohn SK, Cho CH, Kim NK. Oncologic outcomes of self-expanding metallic stent insertion as a bridge to surgery in the management of left-sided colon cancer obstruction: comparison with nonobstructing elective surgery. World J Surg. 2009; 33: 1281–1286.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J. 2008; 336: 924–926.
- Guyatt GH, Thorlund K, Oxman AD, Walter SD, Patrick D, Furukawa TA, Johnston BC, Karanicolas P, Akl EA, Vist G, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol. 2013; 66: 173–183.
- Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, Stassen N, Dahm P. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012; 73: S283–S287.
- Alcantara M, Serra-Aracil X, Falco J, Mora L, Bombardo J, Navarro S. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg. 2011; 35: 1904–1910.
- Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK. Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg. 2009; 144: 1127–1132.
- Ghazal AH, El-Shazly WG, Bessa SS, El-Riwini MT, Hussein AM. Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg. 2013; 17: 1123–1129.
- Ho KS, Quah HM, Lim JF, Tang CL, Eu KW. Endoscopic stenting and elective surgery versus emergency surgery for left-sided malignant colonic obstruction: a prospective randomized trial. Int J Colorectal Dis. 2012; 27: 355–362.
- Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL. Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc. 2011; 25: 1814–1821.
- van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P. Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol. 2011; 12: 344–352.
- Köhler G, Antoniou SA, Lechner M, Mayer F, Mair J, Emmanuel K. Stenting for emergency colorectal obstruction: an analysis of 204 patients in relation to predictors of failure and complications. Scand J Surg. 2015; 104(3): 146–153.