Diaphragmatic Injury, Evaluation and Management of
Published 2018
Citation: J Trauma. 85(1):198-207, July 2018
Authors
McDonald, Amy A., MD; Robinson, Bryce R.H., MD; Alarcon, Louis, MD; Bosarge, Patrick L., MD; Dorion, Heath, MD; Haut, Elliott R., MD, PhD; Juern, Jeremy, MD; Madbak, Firas, MD; Reddy, Srinivas, MD; Weiss, Patricia, MLIS; Como, John J., MD
Author Information
From the Case Western Reserve University (A.A.M., J.J.C.), Cleveland, Ohio; University of Washington (B.R.H.R.), Seattle, Washington; University of Pittsburgh (L.A., P.W.), Pittsburgh, Pennsylvania; University of Alabama (P.L.B.), Birmingham, Alabama; Northeastern Ohio Medical University (H.D.), Youngstown, Ohio; Johns Hopkins University (E.R.H.), Baltimore, Maryland; Medical College of Wisconsin (J.J.), Milwaukee, Wisconsin; University of Florida Jacksonville (F.M.), Jacksonville, Florida; and Albert Einstein College of Medicine (S.R.), New York, New York.
Submitted: January 2, 2018, Accepted: January 8, 2018, Published online: April 3, 2018.
All authors are from the Department of Surgery at said institutions except for P.W. who is from Health Sciences Library System (University of Pittsburgh).
Presented at: The Eastern Association for the Surgery of Trauma 30th Annual Scientific Assembly, January 10–14, 2017, Hollywood, Florida.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Address for reprints: Amy A. McDonald, MD, Louis Stokes Cleveland VA Medical Center, 10701 East Blvd, Surgery 112(W), Cleveland, OH 44106; email: amymcdonald29@gmail.com.
Abstract
BACKGROUND Traumatic diaphragm injuries (TDI) pose both diagnostic and therapeutic challenges in both the acute and chronic phases. There are no published practice management guidelines to date for TDI. We aim to formulate a practice management guideline for TDI using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology.
METHODS The working group formulated five Patient, Intervention, Comparator, Outcome questions regarding the following topics: (1) diagnostic approach (laparoscopy vs. computed tomography); (2) nonoperative management of penetrating right-sided injuries; (3) surgical approach (abdominal or thoracic) for acute TDI, including (4) the use of laparoscopy; and (5) surgical approach (abdominal or thoracic) for delayed TDI. A systematic review was undertaken and last updated December 2016. RevMan 5 (Cochran Collaboration) and GRADEpro (Grade Working Group) software were used. Recommendations were voted on by working group members. Consensus was obtained for each recommendation.
RESULTS A total of 56 articles were used to formulate the recommendations. Most studies were retrospective case series with variable reporting of outcomes measures and outcomes frequently not stratified to intervention or comparator. The overall quality of the evidence was very low for all Patient, Intervention, Comparator, Outcomes. Therefore, only conditional recommendations could be made.
CONCLUSION Recommendations were made in favor of laparoscopy over computed tomography for diagnosis, nonoperative versus operative approach for right-sided penetrating injuries, abdominal versus thoracic approach for acute TDI, and laparoscopy (with the appropriate skill set and resources) versus open approach for isolated TDI. No recommendation could be made for the preferred operative approach for delayed TDI. Very low-quality evidence precluded any strong recommendations. Further study of the diagnostic and therapeutic approaches to TDI is warranted.
LEVEL OF EVIDENCE Guideline; Systematic review, level IV.
Traumatic diaphragm injuries (TDI) pose both diagnostic and therapeutic challenges. The diaphragm is a thoracoabdominal structure, with the thoracoabdomen generally defined as the region between the fourth intercostal space (nipple line) and costal margin. Surgically, the diaphragm can be approached through the chest or abdomen via open or minimally invasive techniques. The preferred approach is often determined by the associated injuries. The largest published series to date on the incidence of TDI is from the American College of Surgeons National Trauma Data Bank in 2012 in which 833,309 patients were analyzed. Traumatic diaphragm injury incidence was 0.46%. Sixty-seven percent were from penetrating injuries and 33% were from blunt injuries. For penetrating mechanisms, gunshot wounds (66.5%) outnumbered stab wounds (33.5%). The most common mechanism for blunt TDI was motor vehicle crash (63.4%) followed by bicycle versus automobile crash (10.1%). Higher injury severity scores (12 ± 13 vs. 8 ± 10) and higher mortality (19.8% vs. 8.8%) were found in blunt injuries compared with penetrating injuries.[1] The true incidence of TDI is likely unknown given the wide use of selective nonoperative management for abdominal injuries in recent years and unreliability of modern imaging for TDI.
Delayed recognition of TDI resulting in diaphragmatic hernia is problematic due to the associated morbidity and mortality. One of the largest contemporary case series of post-traumatic diaphragmatic hernia (TDH) was published by Murray et al.[2] In that series of 28 patients, 14 (50%) presented as surgical emergencies and the mortality was 11%.
There are several published review articles on diaphragm injuries; however, no practice management guidelines currently exist.
Objective
A working group was formed under the Eastern Association for Surgery of Trauma Guideline Committee to formulate a guideline on TDI. The Grading of Recommendations Assessment, Development and Evaluation methodology was used.[3]
Methods
Five Population, Intervention, Comparator, and Outcome (PICO) questions were generated a priori to the systematic literature review. Pertinent outcomes were identified by the working group and then voted on using a scale of 1 to 9. Outcomes receiving an average score of 7 to 9 were deemed critical outcomes, those receiving an average score of 4 to 6 were considered important, but not critical, and those receiving an average score of 1 to 3 were considered of limited importance. Only critical and important outcomes were considered in decision making for generating final recommendations.
Mortality, missed diaphragm injury, and need for delayed operation for diaphragmatic hernia or missed thoracoabdominal organ injury were identified as critical outcomes. Length of stay (LOS), empyema, surgical site infection, and procedural complications of the diagnostic or therapeutic approach were identified as important, but not critical outcomes. The outcomes were matched to appropriately fit each PICO question. In formulating the recommendations, the outcomes were considered in aggregate.
PICO 1: In left-sided thoracoabdominal stab wound patients who are hemodynamically stable and without peritonitis (P), should laparoscopy (I) or computed tomography (C) be performed to decrease the incidence missed diaphragmatic injury (O)?
PICO 2: In penetrating thoracoabdominal trauma patients who are hemodynamically stable without peritonitis and in whom a right diaphragm injury is confirmed or suspected (P), should operative (I) or non-operative (C) management be undertaken to minimize both the need for delayed operation for diaphragmatic hernia and risk of surgical morbidity (procedural complications, LOS, surgical site infection, and empyema) (O)?
PICO 3: In hemodynamically stable trauma patients with acute diaphragm injuries (P) should the abdominal (I) or thoracic (C) approach be used to repair the diaphragm to decrease mortality, delayed herniation, missed thoracoabdominal organ injury, and surgical approach-associated morbidity (procedural complications, LOS, surgical site infection, and empyema) (O)?
PICO 4: In patients who present with delayed visceral herniation through a traumatic diaphragmatic injury (P), should the abdominal (I) or thoracic (C) approach be used to decrease mortality and surgical approach related morbidity (procedural complications, surgical site infection, LOS, empyema) (O)?
PICO 5: In patients with acute penetrating diaphragmatic injuries without concern for other intraabdominal injuries (P) should laparoscopic (I) or open (C) repair be performed to decrease mortality, delayed herniation, missed thoracoabdominal organ injury, and surgical approach-associated morbidity (procedural complications, LOS, surgical site infection, and empyema) (O)?
As it is generally accepted that penetrating injuries to the left diaphragm require repair, no PICO question was formulated to study this topic.
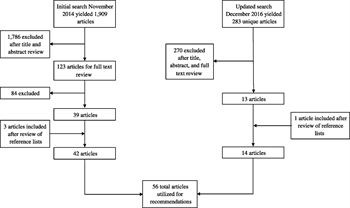
FIGURE 1. PRISMA flow diagram
A professional librarian performed an initial literature search of Ovid Medline and EMBASE in November 2014. An updated search was performed on December 8, 2016. Inclusion criteria were studies in English investigating adults. Letters, comments, single case reports, meta-analyses, or inability to locate a full text article constituted grounds for exclusion. The initial search yielded 1,909 articles. After removal of duplicates, application of the inclusion and exclusion criteria, and title and abstract review, 123 articles remained. To evaluate further for inclusion or exclusion, full text review of each article was performed by at least two members of the working group. The chairperson of the working group evaluated the full text of all articles. Discrepancies regarding inclusion or exclusion of the articles were adjudicated by the chairperson. Ultimately, 42 relevant articles were identified from this search, and this included three identified from bibliographic review. For the updated literature search, the chairperson performed the initial title, abstract, and full text review. Potentially relevant articles were identified, and the full text articles were sent to working group members for further review. Fourteen articles, which included one from bibliographic review, were deemed relevant. In total, 56 articles were used for generating recommendations. See Figure 1 (PRISMA). When appropriate, after data extraction, graphs and Forest plots were generated by RevMan 5 (Cochrane Community, London, United Kingdom). No external funding was obtained for this work.
Results
Results for Laparoscopy Versus Computed Tomography for Left-Sided Thoracoabdominal Stab Wounds (PICO 1)
No study directly compared laparoscopy to computed tomography (CT), and then to a reference standard. Twelve studies compared CT with a reference standard[4–15] and six studies[16–21] compared laparoscopy with a reference standard. There were four prospective cross-sectional cohort studies in the CT group[4][7][13][15] and eight retrospective studies.[5][6][8–12][14] In the laparoscopy group, there were five prospective cross-sectional cohort studies[16–18][20][21] and one retrospective study.[19] The Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool was used to determine risk of bias and applicability of the studies.[22] (see Figure Supplemental Digital Content 1, http://links.lww.com/TA/B135).
Sources of significant bias and applicability were found in patient selection and index test performance. Most study designs were retrospective, and in four prospective studies, it was unclear whether a consecutive or random sample was enrolled.[17][18][20][21] Furthermore, many patients did not have isolated left thoracoabdominal stab wounds. Only one study, Yucel et al.,[15] specifically evaluated isolated left thoracoabdominal stab wound patients; however, Ilhan et al.[9] did evaluate “sharp” penetrating injuries to the left thoracoabdomen. Some evaluated thoracoabdominal stab wound patients not isolated to the left side.[4][6][19] Most evaluated a mixed penetrating injury population (gunshot and stab wounds) with some isolated to the thoracoabdomen[8][12][16][20] and others not limited to the thoracoabdomen.[7][10][11][14][17][18][21] Berardoni et al.[5] evaluated anterior abdominal stab wounds and Melo et al.[13] evaluated gunshot wounds to the abdomen.
Differing CT imaging techniques were used. In the study by Abbasy et al.,[4] all patients had chest tubes and contrast was given via the chest tube. Furthermore, multidetector CT (MDCT) was not used in this study. MDCT was used in all the other studies, although the slice count ranged from four to 64.[5–15] Four studies did use 64-slice MDCT.[8–11]
Except for the Abbassy study,[4] where the patients were examined prospectively and both the radiologist and surgeon were masked to the results of the other, there was some degree of diagnostic review or partial verification bias. Differential verification bias was also present both between studies and within studies. Laparotomy, laparoscopy (used in some CT studies), thoracoscopy, and thoracotomy were all used as reference standards.
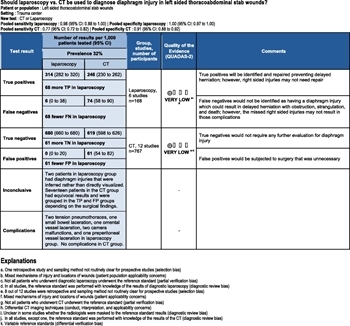
FIGURE 2. PICO 1 summary of findings table
The pooled TDI prevalence for included studies was 32%. There were a total of 168 patients in six studies in the laparoscopy group and 767 patients in 12 studies in the CT group (see Figs. 2 and 3). The pooled sensitivity for laparoscopy was 0.98 with 95% confidence interval (CI) of 0.88 to 1.00. The pooled specificity of laparoscopy was 1.00 (95% CI, 0.97–1.00). Of note, there were two patients in the Ivatury study[17] in which the TDI was not directly visualized due to blood obscuring the diaphragm. Traumatic diaphragm injury was highly suspected in both patients and laparotomy confirmed TDI. The pooled sensitivity and specificity for CT were 0.77 (95% CI, 0.72–0.82) and 0.91 (95% CI, 0.88–0.92), respectively. There was one study in the CT group, by Stein et al.[14] in which there were 17 inconclusive CT examinations. These were classified into the true-positive and false-positive categories depending on the surgical findings. We chose to classify the surgical negative findings in these 17 inconclusive examinations as false positives rather than false negatives as inconclusive results would likely result in surgery to further evaluate for TDI.
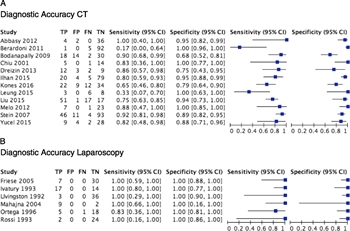
FIGURE 3. Forest plots for the sensitivity and specificity of CT (A) and laparoscopy (B) for detecting left diaphragm injuries from penetrating left thoracoabdominal stab wounds
Compared with CT, laparoscopy misses very few diaphragmatic injuries. Therefore, fewer patients would be at risk for delayed diaphragmatic hernia if laparoscopy were used as the standard method of diagnosis. This, however, needs to be weighed against the procedural risks of laparoscopy. The procedural risks of CT are essentially limited to the contrast media and long-term radiation effects. Intravenous contrast media associated adverse reactions to nonionic low or iso-osmolar agents range from 0.2% to 0.7%.[23] In the six included studies for laparoscopy, there were a total of six complications in 273 (2.2%) patients. The number of patients is higher than included for the diagnostic accuracy data because in some of the series, laparoscopy was used as a diagnostic tool beyond TDI.
Complications were not stratified by the indication for laparoscopy. Three complications were minor (camera malfunction and preperitoneal gas insufflation).[17][18][20] Three (1.1%) complications were serious and included a single patient with a tension pneumothorax requiring desufflation of the abdomen and tube thoracostomy insertion,[17] small bowel laceration,[21] and omental vessel laceration.[21] Overall, the complication rate of laparoscopy for penetrating injury evaluation is less than 3% with mortality related to the intervention of 0.1%.[24]
Given the superior diagnostic capability of laparoscopy and low risk of complications, the working group made the following recommendation:
In left thoracoabdominal stab wound patients who are hemodynamically stable and without peritonitis (P), we conditionally recommend laparoscopy (I) rather that computed tomography (C) to decrease the incidence missed diaphragmatic injury (O).
Discussion for Laparoscopy vs. CT for Left-Sided Thoracoabdominal Stab Wounds (PICO 1)
A conditional recommendation was made given the very low quality of evidence and because there may be some instances in which diagnostic laparoscopy may not be the optimal choice due to access or intraperitoneal visibility concerns. In these instances, CT might be considered with future outpatient imaging given the lower diagnostic capability and risk for missed TDI. A CT-first approach may be appropriate when trajectory in proximity to the diaphragm is questioned. If the wound tract is traversing the diaphragm or there are contiguous injuries on both sides of the diaphragm, then TDI is likely present, and surgical repair is likely indicated.[25][26]
Although this systematic review did not specifically address thoracoscopy, several studies have found thoracoscopy to be an appropriate screening tool and potentially better than laparoscopy for posterior and right-sided TDI.[27–32] If an injury is found, intra-abdominal injury still needs to be excluded. The option of thoracoscopy followed a period of observation for abdominal injuries has been reported.[31][32]
Results for Operative Versus Nonoperative Management of Hemodynamically Stable Patients with Right-Sided, Penetrating Thoracoabdominal Injury (PICO 2)
A total of six studies fulfilled criteria for inclusion in this PICO.[2][19][31][33–35] None of these studies' primary outcome was to evaluate planned nonoperative management of right-sided penetrating TDI. Five of the six studies[2][19][31][33][34] referred to a subpopulation with right-sided penetrating TDI managed with nonoperative therapy.
Nonoperative management of right-sided wounds is commonly practiced. Berg et al.,[33] in a diagnostic study of laparoscopy for TDI, reported 27 patients who had non-operative management of right-sided or posterior TDI. There was no outcome data for these 27 patients. Ertekin et al.,[34] in a diagnostic study of laparoscopy which included 22 patients with penetrating thoracoabdominal wounds reported four patients with right-sided TDI who were managed non-operatively. No major morbidity or mortality was noted with a mean follow-up of 13 months (range 5 to 20) for the entire study population. Mahajna et al.,[19] in a diagnostic study of laparoscopy which included 43 patients with thoracoabdominal penetrating wounds, reports one patient with a right-sided wound managed non-operatively, although no outcome data were reported. Wong et al.,[31] in a diagnostic and therapeutic study of thoracoscopy in trauma noted one right-sided penetrating TDI patient who was initially managed nonoperatively and then presented with bilious output from a chest tube on posttrauma day 3. That patient underwent thoracoscopy and repair.
Regarding the complication of diaphragmatic hernia from a right-sided penetrating TDI, there was one study, by Murray et al.,[2] that reported 28 patients with delayed diaphragmatic hernia from TDI. In that study, one patient presented with a right-sided diaphragmatic hernia four months after planned non-operative management of a right-sided TDI from a stab wound while all the rest were left-sided. This was the only case of delayed right-sided diaphragmatic hernia from a penetrating right TDI in our systematic review for all PICOs.
The overall quality of evidence for this PICO is very low given that all studies are case series, none were designed to evaluate planned nonoperative management of right-sided injuries, and because there was a significant lack of outcome data. Factoring the overall paucity of high quality literature and the morbidity associated with surgery to repair the injury, the working group made the following recommendation:
In penetrating thoracoabdominal trauma patients in whom a right diaphragm injury is confirmed or suspected, and who are hemodynamically stable without peritonitis (P), we conditionally recommend nonoperative (I) over operative (O) management in weighing the risks of delayed herniation, missed thoracoabdominal organ injury, and surgical morbidity (procedural complications, LOS, surgical site infection, and empyema) (O).
Discussion for Operative Versus Nonoperative Management of Hemodynamically Stable Patients with Right-Sided, Penetrating Thoracoabdominal Injury (PICO 2)
A conditional recommendation could only be supported given the very limited amount of published data and poor study quality. There also may be instances in which a right-sided injury should be repaired such as when encountered incidentally during surgery or when complications related to the right-sided TDI are likely to occur (e.g., fistula, large defect). Lower lateral or lower anterior wounds may afford less protection from herniation by the liver and may warrant consideration of repair.
Results for Repair of Hemodynamically Stable, Acute Diaphragmatic Injuries by an Abdominal or Thoracic Approach (PICO 3)
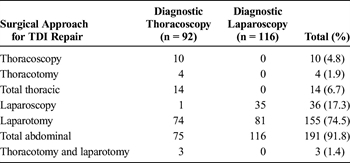
TABLE 1. Surgical Approach for Acute TDI Repair in Stable Patients Who Initially Underwent Either Diagnostic Thoracoscopy or Diagnostic Laparoscopy
Ten studies with a total of 208 patients that specifically evaluated stable patients with TDI were identified. All studies were designed to assess the diagnostic capability of either laparoscopy or thoracoscopy for TDI. No studies were specifically designed to compare the surgical approach, by cavity, for repair. Penetrating mechanisms dominated the patient population with only three of 208 (1.4%) patients having sustained blunt trauma. There were five prospective cohort designs[27][29][30][36][37] and six retrospective case series.[28][31][38–41] Six studies evaluated laparoscopy,[36–41] and five studies evaluated thoracoscopy.[27–31] In total, 191 (91.8%) of 208 of patients underwent an abdominal approach, 14 (6.7%) of 208 underwent a thoracic approach, and a combined approach was used in 3 (1.4%) of 208 patients. No mortality, missed injuries, or recurrent diaphragmatic hernias were noted in the studies; though most studies did not specifically report these outcomes. In patients who underwent laparotomy for repair, two wound infections, two intraabdominal abscesses, and one small-bowel obstruction were noted. No thoracic approach-related complications were reported. Matching of patient populations by patient characteristics and associated injuries to surgical approach was not possible; therefore, no conclusion can be made regarding the superiority of one approach over another (see Table 1).
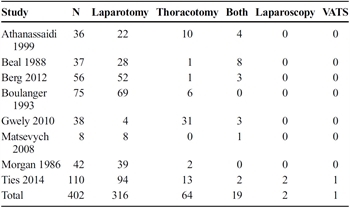
TABLE 2. Acute Blunt TDI Surgical Approach
Regarding blunt mechanisms, only Wong et al.[31] specifically addressed stable blunt TDI patients, although only three patients were included. In that study, two underwent laparotomy for repair and one underwent thoracoscopic repair. There were eight studies that evaluated blunt TDI regardless of hemodynamic stability where the surgical approach was clearly defined.[42–49] These studies were all retrospective case series. In total, 318 (79.1%) of 402 patients underwent an abdominal approach, 65 (16.2%) of 402 underwent a thoracic approach, and a combined approach was used in 19 (4.7%) of 402 patients (see Table 2).
The prevalence of intraabdominal injuries potentially requiring surgical intervention in the stable penetrating population ranges from 53% to 88.9%, as illustrated by Freeman et al, Spann et al, Uribe et al, and Yucel et al.[28–30][37] Thoracic injuries were common and found in up to 87.5% of patients.[29] These injuries were mainly hemopneumothoraces and commonly did not require more than a tube thoracostomy. Freeman et al.[28] did report 3 (5%) of 60 patients who required a thoracotomy and 9 (15%) of 60 patients who underwent thoracoscopic pericardial windows or lung resections. However, Freeman also reported that 47 (78%) of 60 patients had an associated intraabdominal injury with 33 (70%) of 47 requiring more than minimal intervention. Regarding blunt injuries, Reiff et al.[50] in a large study of the National Automotive Sampling System showed splenic injuries to have the strongest positive association with TDI (Odds Ratio, 8.4) compared with other injuries. Fair et al.,[1] in the 2012 National Trauma Data Bank study, also showed predominance of surgically amenable abdominal injuries with blunt and penetrating TDI (see Table, Supplemental Digital Content 2, http://links.lww.com/TA/B156).
Taking into consideration the available evidence for a recommendation for this PICO the working group decided on the following recommendation:
In hemodynamically stable trauma patients with acute diaphragm injuries, we conditionally recommend (P) the abdominal (I) rather than the thoracic (C) approach to repair the diaphragm to decrease mortality, delayed herniation, missed thoracoabdominal organ injury, and surgical approach-associated morbidity (procedural complications, LOS, surgical site infection, and empyema) (O).
Discussion for Evaluation of Acute Diaphragmatic Injuries by an Abdominal or Thoracic Approach (PICO 3)
This recommendation is conditional for several reasons. The quality of evidence is very low. There are no studies with matched patient populations comparing operative approaches; therefore, we rely on indirect evidence based on associated injuries and historical percentage of repairs done by each approach. There may be instances in which a thoracic approach is initially indicated to address an immediate life-threatening intrathoracic injury.
Results for Operative Approach for Delayed Visceral Herniation Repair (PICO 4)
Studies were included if the diagnosis of TDH was made after the trauma index hospitalization and the operative approach was clearly defined. Fifteen studies fulfilled these criteria, and all were retrospective case series.[2][42][45][46][51–61]There was variable reporting of patient acuity (elective vs. emergent) and outcome measures. The only study that directly compared a transabdominal (TA) to transthoracic (TT) approach for TDH was by Murray et al.[2] In this small study of 28 patients, 19 underwent a TA approach and nine underwent a TT approach. However, 13 of the 19 TA patients and only one of the nine TT patients presented emergently (p = 0.01). Mortality, ventilator days, ICU, and hospital LOS were not different. Regarding procedural and post-operative complications only the incidence of pneumonia was statistically different between the two groups with a higher incidence in the TT group (p = 0.03) (see Table, Supplemental Digital Content 3, http://links.lww.com/TA/B157).
In total, 79 (54.5%) of 145 patients underwent an abdominal approach, 51 (35.2%) of 145 patients underwent a thoracic approach, and 15 (10.3%) of 145 patients underwent a combined approach. Of the combined approach, eight laparotomies were converted to thoracotomy, and one thoracotomy was converted to laparotomy.
Both approaches (thoracic and abdominal) can be used, and it is difficult to draw any conclusions regarding the preferred approach based on the studies analyzed due to patient and author biases. Those with emergent presentations with ischemic or gangrenous viscera are generally approached through the abdomen and by nature of the presentation may face worse overall outcomes. As demonstrated in several studies, preparation and anticipation of the need for a second cavity approach (thoracotomy or laparotomy) due to potential difficulties reducing hernia contents from the initial approach is wise. Based on the available data for this PICO, the working group could not make a formal recommendation favoring one approach over the other; therefore:
In patients who present with delayed visceral herniation through a traumatic diaphragmatic injury (P), we make no recommendation in regard to the routine surgical approach, abdominal (I) or thoracic (O) to decrease mortality and surgical approach-related morbidity (procedural complications, surgical site infection, LOS, empyema) (O).
Discussion for Operative Approach for Delayed Visceral Herniation Repair (PICO 4)
This decision should be made on a case by case basis and dictated by the acuity of presentation, concerns for visceral ischemia, and anticipated difficulties of reducing the hernia contents. Surgeon training and specialization should also be considered.
Results for Open Versus Laparoscopic Approach for Acute, Penetrating Diaphragmatic Injuries (PICO 5)
Included studies required more than one patient in each of the laparoscopic and open groups, along with outcome comparisons between these groups. Only four studies fulfilled these criteria.[36][37][41][56] Two were prospective cohort studies[36][37] and two were retrospective case series.[56] Combining these studies, there were 30 patients in the laparoscopic group and 37 patients in the open group. All patients in the open group had laparotomy. Three of the four studies included only penetrating TDI.[36][37][41] Matthews et al.[56] included both blunt and penetrating injuries as well as several chronic diaphragmatic hernias (nine out of the total 17). Furthermore, all repairs were initially attempted laparoscopically. The four open repairs were conversions due to operative difficulty. Operative difficulty in the four patients was related to the size of diaphragmatic laceration (>10 cm) or location of the laceration (anterior to the esophageal hiatus, adjacent to the pericardium, or communicating with the esophageal hiatus).
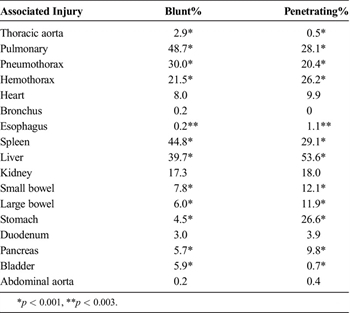
TABLE 3. Percentage of Associated Injuries With TDI Based on Mechanism of Injury (Fair et al.1)
In the prospective penetrating TDI study by Murray et al.,[36] all patients were observed for six hours prior to attempted laparoscopic repair. It was unclear after that time frame how patients were selected for laparoscopic or open repair. In the prospective penetrating TDI study by Yucel et al.,[37] it was unclear how patients were selected for laparoscopic or open repair; however, all four patients who had laparotomy had hollow viscus injuries. There were two patients with spleen injuries and one with a liver injury that required no further therapy in the laparoscopic repair group, and all patients with the repair completed laparoscopically were observed for 48 hours postoperatively. The patient selection criteria for the retrospective study by Cooper et al.[41] was isolated diaphragm injuries, though it was unclear how patients were initially selected for each operative approach. All four studies showed a decrease in LOS with laparoscopic repair compared to open repair. No study addressed mortality. Only Yucel et al.[37] specifically stated that there were no missed diagnoses in their study, and this was the only study to include long-term follow-up data (mean, 2.44 years; range, 1–4) with no evidence of recurrent hernias in the laparoscopic group (see Table 3).
The overall quality of evidence for this PICO is very low. This is attributed to multiple factors including: small number of studies and low number of participants in each group, research design flaws with significant patient selection bias, and inconsistent/variable outcome reporting. Publication bias may also be present as positive experience with laparoscopic repair of TDI might be submitted to journals for publication and published. However, the feasibility and safety of laparoscopic repair has been demonstrated in the above studies in appropriately selected populations, and we limited this PICO to patients with a very low concern for other intraabdominal injuries.
There have been several other case series published along with the systematic review by O'Malley et al. recognizing the feasibility and safety of laparoscopy for TDI and trauma in general.[24][33][34][48][62–64] Also, Zafar et al.[65] examined the NTDB from 2007 to 2010 which included 4,755 patients who underwent diagnostic laparoscopy and of those patients, 916 underwent a laparoscopic therapeutic procedure. The most common therapeutic procedure was TDI repair (176 [19.2%] of 916 therapeutic procedures). For the entire cohort of 4,755 patients, the missed injury rate was 0.5%. Of patients with isolated abdominal injuries undergoing a therapeutic laparoscopic procedure (n = 382) not limited to TDI repair, there was one mortality (0.26%). This mortality rate was also compared with 331 patients who had isolated abdominal injuries and underwent diagnostic laparoscopy followed by open repair of injuries. In this group of patients, three (0.91%) died. The hospital LOS was also compared with the two groups and the therapeutic laparoscopy group LOS was 5 days (interquartile range, 3–7 days) compared to 6 days (interquartile range, 4–8 days) in the therapeutic open group. This was statistically significant (p < 0.001). This very large study adds robust data to the feasibility, safety, and potential benefit of laparoscopic repair. Therefore, the working group made the following recommendation:
In patients with acute penetrating diaphragmatic injuries without concern for other intraabdominal injuries (P) we conditionally recommend laparoscopic (I) over open (C) repair in weighing the risks of mortality, delayed herniation, missed thoracoabdominal organ, and surgical approach-associated morbidity (procedural complications, LOS, surgical site infection, and empyema) (O).
Discussion for Open Versus Laparoscopic Approach for Acute, Penetrating Diaphragmatic Injuries (PICO 5)
This recommendation is conditional for several reasons beyond the quality of the evidence. We feel patients selected for laparoscopic repair should be hemodynamically stable, have no other contraindications to laparoscopy, and not have significant associated intraabdominal injuries. In addressing this issue, some studies have incorporated a period of observation to allow for other injuries to manifest if present prior to attempted laparoscopic repair.[33][36][62][64] These periods of observation have ranged from 6 hours to 24 hours. For this approach to succeed, the operating room must have the appropriate staffing and equipment along with a surgeon who possesses the necessary laparoscopic skill set and has a low threshold for conversion to an open procedure.
Future Investigations
All recommendations were supported by very low quality evidence with a predominance of descriptive, retrospective case series. The diagnostic and therapeutic aspects of TDI would benefit from further higher quality research. This may become even more pertinent as CT imaging technology advances, therapeutic minimally invasive techniques are employed more frequently in trauma, and patients continue to be managed non-operatively with penetrating right TDI. Both the strength and direction of the recommendation may change as additional research becomes available.
Using these Guidelines in Clinical Practice
We advocate for individual institutions to establish trauma care algorithms/protocols that address both screening for and treatment of TDI. Those patients screened for TDI with CT only and those patients managed non-operatively with penetrating right sided TDI should have longer term outpatient follow-up. As minimally invasive surgery continues to expand in trauma, maintenance of competency in these techniques can be considered a necessity for trauma surgeons.
Conclusion
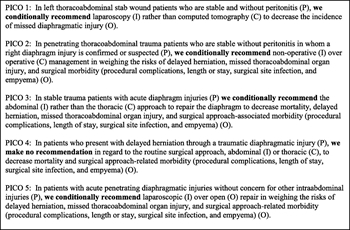
FIGURE 4. Summary of recommendations
In summary, the superior diagnostic capability of laparoscopy to CT along with its relative safety and feasibility make it the preferred choice for most patients needing evaluation for penetrating TDI. Not only that, laparoscopy may be the preferred surgical approach over open repair in those patients with isolated TDI in stable patients. The surgical repair approach (abdominal vs. thoracic) in acutely injured patients with associated injuries will be determined by the life-threatening nature and surgical amenability of those associated injuries. In general, the abdominal approach will dominate based on those factors. Chronic diaphragmatic hernias from missed TDI can be approached through the chest or abdomen and the choice of approach will depend on the acuity of presentation (emergent vs. elective), concern for difficulties reducing the hernia back into the abdomen, and surgical specialization of the surgeon. Preparation for two cavity incisions is advisable (see Figure 4).
Authorship
J.J.C. participated in study inception. A.A.M., L.A., P.L.B., H.D., E.R.H., J.J., F.M., S.R., J.J.C. participated in PICO questions and outcomes. A.A.M., L.A., P.W. participated in literature search. A.A.M., L.A., P.L.B., H.D., E.R.H., J.J., F.M., S.R., J.J.C. participated in abstract and title review. A.A.M., L.A., P.L.B., H.D., E.R.H., J.J., F.M., S.R., J.J.C. participated in full text review. A.A.M., B.R.H.R., L.A., P.L.B., H.D., E.R.H., J.J., F.M., S.R., P.W., J.J.C. participated in data collection, analysis, and interpretation. A.A.M. participated in manuscript preparation. A.A.M., B.R.H.R., L.A., P.L.B., H.D., E.R.H., J.J., F.M., S.R., P.W., J.J.C. participated in critical revision. A.A.M., B.R.H.R., L.A., P.L.B., H.D., E.R.H., J.J., F.M., S.R., P.W., J.J.C. participated in final review and responsibility for content.
Disclosure
No conflicts of interest to disclose.
Source of funding: None.
References
- Fair KA, Gordon NT, Barbosa RR, Rowell SE, Watters JM, Schreiber MA. Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank: a new examination of a rare diagnosis. Am J Surg. 2015;209:864–868; discussion 868–9.
- Murray JA, Weng J, Velmahos GC, Demetriades D. Abdominal approach to chronic diaphragmatic hernias: is it safe? Am Surg. 2004;70:897–900.
- Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, Stassen N, Dahm P. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73:S283–S287.
- Abbasy HR, Panahi F, Sefidbakht S, Akrami M, Paydar S, Mirhashemi S, Bolandparvaz S, Asaadi K, Salahi R. Evaluation of intrapleural contrast-enhanced abdominal pelvic CT-scan in detecting diaphragm injury in stable patients with thoraco-abdominal stab wound: a preliminary study. Injury. 2012;43:1466–1469.
- Berardoni NE, Kopelman TR, O'Neill PJ, August DL, Vail SJ, Pieri PG, Singer Pressman MA. Use of computed tomography in the initial evaluation of anterior abdominal stab wounds. Am J Surg. 2011;202:690–695; discussion 695–6.
- Bodanapally UK, Shanmuganathan K, Mirvis SE, Sliker CW, Fleiter TR, Sarada K, Miller LA, Stein DM, Alexander M. MDCT diagnosis of penetrating diaphragm injury. Eur Radiol. 2009;19:1875–1881.
- Chiu WC, Shanmuganathan K, Mirvis SE, Scalea TM. Determining the need for laparotomy in penetrating torso trauma: a prospective study using triple-contrast enhanced abdominopelvic computed tomography. J Trauma. 2001;51:860–868; discussion 8–9.
- Dreizin D, Borja MJ, Danton GH, Kadakia K, Caban K, Rivas LA, Munera F. Penetrating diaphragmatic injury: accuracy of 64-section multidetector CT with trajectography. Radiology. 2013;268:729–737.
- Ilhan M, Bulakçi M, Bademler S, Gök AF, Azamat IF, Ertekin C. The diagnostic efficacy of computed tomography in detecting diaphragmatic injury secondary to thoracoabdominal penetrating traumas: a comparison with diagnostic laparoscopy. Ulus Travma Acil Cerrahi Derg. 2015;21:484–490.
- Kones O, Akarsu C, Dogan H, Okuturlar Y, Dural AC, Karabulut M, Gemici E, Alis H. Is non-operative approach applicable for penetrating injuries of the left thoraco-abdominal region? Turk J Emerg Med. 2016;16:22–25.
- Leung VA, Patlas MN, Reid S, Coates A, Nicolaou S. Imaging of traumatic diaphragmatic rupture: evaluation of diagnostic accuracy at a level 1 trauma centre. Can Assoc Radiol J. 2015;66:310–317.
- Liu J, Yue WD, Du DY. Multi-slice computed tomography for diagnosis of combined thoracoabdominal injury. Chin J Traumatol. 2015;18:27–32.
- Melo EL, de Menezes MR, Cerri GG. Abdominal gunshot wounds: multi-detector-row CT findings compared with laparotomy: a prospective study. Emerg Radiol. 2012;19:35–41.
- Stein DM, York GB, Boswell S, Shanmuganathan K, Haan JM, Scalea TM. Accuracy of computed tomography (CT) scan in the detection of penetrating diaphragm injury. J Trauma. 2007;63:538–543.
- Yucel M, Bas G, Kulali F, Unal E, Ozpek A, Basak F, Sisik A, Acar A, Alimoglu O. Evaluation of diaphragm in penetrating left thoracoabdominal stab injuries: the role of multislice computed tomography. Injury. 2015;46:1734–1737.
- Friese RS, Coln CE, Gentilello LM. Laparoscopy is sufficient to exclude occult diaphragm injury after penetrating abdominal trauma. J Trauma. 2005;58:789–792.
- Ivatury RR, Simon RJ, Stahl WM. A critical evaluation of laparoscopy in penetrating abdominal trauma. J Trauma. 1993;34:822–827; discussion 827–8.
- Livingston DH, Tortella BJ, Blackwood J, Machiedo GW, Rush BF Jr. The role of laparoscopy in abdominal trauma. J Trauma. 1992;33:471–475.
- Mahajna A, Mitkal S, Bahuth H, Krausz MM. Diagnostic laparoscopy for penetrating injuries in the thoracoabdominal region. Surg Endosc. 2004;18:1485–1487.
- Ortega AE, Tang E, Froes ET, Asensio JA, Katkhouda N, Demetriades D. Laparoscopic evaluation of penetrating thoracoabdominal traumatic injuries. Surg Endosc. 1996;10:19–22.
- Rossi P, Mullins D, Thal E. Role of laparoscopy in the evaluation of abdominal trauma. Am J Surg. 1993;166:707–710; discussion 710–1.
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
- Beckett KR, Moriarity AK, Langer JM. Safe use of contrast media: what the radiologist needs to know. Radiographics. 2015;35:1738–1750.
- O'Malley E, Boyle E, O'Callaghan A, Coffey JC, Walsh SR. Role of laparoscopy in penetrating abdominal trauma: a systematic review. World J Surg. 2013;37:113–122.
- Hammer MM, Flagg E, Mellnick VM, Cummings KW, Bhalla S, Raptis CA. Computed tomography of blunt and penetrating diaphragmatic injury: sensitivity and inter-observer agreement of CT Signs. Emerg Radiol. 2014;21:143–149.
- Panda A, Kumar A, Gamanagatti S, Patil A, Kumar S, Gupta A. Traumatic diaphragmatic injury: a review of CT signs and the difference between blunt and penetrating injury. Diagn Interv Radiol. 2014;20:121–128.
- Bagheri R, Tavassoli A, Sadrizadeh A, Mashhadi MR, Shahri F, Shojaeian R. The role of thoracoscopy for the diagnosis of hidden diaphragmatic injuries in penetrating thoracoabdominal trauma. Interact Cardiovasc Thorac Surg. 2009;9:195–197; discussion 7–8.
- Freeman RK, Al-Dossari G, Hutcheson KA, Huber L, Jessen ME, Meyer DM, Wait MA, DiMaio JM. Indications for using video-assisted thoracoscopic surgery to diagnose diaphragmatic injuries after penetrating chest trauma. Ann Thorac Surg. 2001;72:342–347.
- Spann JC, Nwariaku FE, Wait M. Evaluation of video-assisted thoracoscopic surgery in the diagnosis of diaphragmatic injuries. Am J Surg. 1995;170:628–630; discussion 30–1.
- Uribe RA, Pachon CE, Frame SB, Enderson BL, Escobar F, Garcia GA. A prospective evaluation of thoracoscopy for the diagnosis of penetrating thoracoabdominal trauma. J Trauma. 1994;37:650–654.
- Wong MS, Tsoi EK, Henderson VJ, Hirvela ER, Forest CT, Smith RS, Fry WR, Organ CH Jr. Videothoracoscopy an effective method for evaluating and managing thoracic trauma patients. Surg Endosc. 1996;10:118–121.
- Martinez M, Briz JE, Carillo EH. Video thoracoscopy expedites the diagnosis and treatment of penetrating diaphragmatic injuries. Surg Endosc. 2001;15:28–32; discussion 33.
- Berg RJ, Karamanos E, Inaba K, Okoye O, Teixeira PG, Demetriades D. The persistent diagnostic challenge of thoracoabdominal stab wounds. J Trauma Acute Care Surg. 2014;76:418–423.
- Ertekin C, Onaran Y, Güloglu R, Günay K, Taviloglu K. The use of laparoscopy as a primary diagnostic and therapeutic method in penetrating wounds of lower thoracal region. Surg Laparosc Endosc. 1998;8:26–29.
- Feliciano DV, Cruse PA, Mattox KL, Bitondo CG, Burch JM, Noon GP, Beall AC Jr. Delayed diagnosis of injuries to the diaphragm after penetrating wounds. J Trauma. 1988;28:1135–1144.
- Murray JA, Demetriades D, Asensio JA, Cornwell EE 3rd, Velmahos GC, Belzberg H, Berne TV. Occult injuries to the diaphragm: prospective evaluation of laparoscopy in penetrating injuries to the left lower chest. J Am Coll Surg. 1998;187:626–630.
- Yucel T, Gonullu D, Matur R, Akinci H, Ozkan SG, Kuroglu E, Ilgun S, Koksoy FN. Laparoscopic management of left thoracoabdominal stab wounds: a prospective study. Surg Laparosc Endosc Percutan Tech. 2010;20:42–45.
- D'Souza N, Bruce JL, Clarke DL, Laing GL. Laparoscopy for occult left-sided diaphragm injury following penetrating thoracoabdominal trauma is both diagnostic and therapeutic. Surg Laparosc Endosc Percutan Tech. 2016;26:e5–e8.
- McQuay N Jr, Britt LD. Laparoscopy in the evaluation of penetrating thoracoabdominal trauma. Am Surg. 2003;69:788–791.
- Powell BS, Magnotti LJ, Schroeppel TJ, Finnell CW, Savage SA, Fischer PE, Fabian TC, Croce MA. Diagnostic laparoscopyfor the evaluation of occult diaphragmatic injury following penetrating thoracoabdominal trauma. Injury. 2008;39:530–534.
- Cooper CA, Brewer JJ. A comparison of laparoscopic and open repair of acute penetrating diaphragm injury. Am Surg. 2016;82:e128–129.
- Athanassiadi K, Kalavrouziotis G, Athanassiou M, Vernikos P, Skrekas G, Poultsidi A, Bellenis I. Blunt diaphragmatic rupture. Eur J Cardiothorac Surg. 1999;15:469–474.
- Beal SL, McKennan M. Blunt diaphragm rupture. A morbid injury. Arch Surg. 1988;123:828–832.
- Boulanger BR, Milzman DP, Rosati C, Rodriguez A. A comparison of right and left blunt traumatic diaphragmatic rupture. J Trauma. 1993;35:255–260.
- Gwely NN. Outcome of blunt diaphragmatic rupture. Analysis of 44 cases. Asian Cardiovasc Thorac Ann. 2010;18:240–243.
- Matsevych OY. Blunt diaphragmatic rupture: four year's experience. Hernia. 2008;12:73–78.
- Morgan AS, Flancbaum L, Esposito T, Cox EF. Blunt injury to the diaphragm: an analysis of 44 patients. J Trauma. 1986;26:565–568.
- Ties JS, Peschman JR, Moreno A, Mathiason MA, Kallies KJ, Martin RF, Brasel KJ, Cogbill TH. Evolution in the management of traumatic diaphragmatic injuries: a multicenter review. J Trauma Acute Care Surg. 2014;76:1024–1028.
- Berg RJ, Okoye O, Teixeira PG, Inaba K, Demetriades D. The double jeopardy of blunt thoracoabdominal trauma. Arch Surg. 2012;147:498–504.
- Reiff DA, McGwin G Jr, Metzger J, Windham ST, Doss M, Rue LW 3rd. Identifying injuries and motor vehicle collision characteristics that together are suggestive of diaphragmatic rupture. J Trauma. 2002;53:1139–1145.
- de Nadai TR, Lopes JC, Inaco Cirino CC, Godinho M, Rodrigues AJ, Scarpelini S. Diaphragmatic hernia repair more than four years after severe trauma: four case reports. Int J Surg Case Rep. 2015;14:72–76.
- Dinc T, Kayilioglu SI, Coskun F. Late onset traumatic diaphragmatic herniation leading to intestinal obstruction and pancreatitis: two separate cases. Case Rep Emerg Med. 2015;2015:549013.
- Hegarty MM, Bryer JV, Angorn IB, Baker LW. Delayed presentation of traumatic diaphragmatic hernia. Ann Surg. 1978;188:229–233.
- Hofmann S, Kornmann M, Henne-Bruns D, Formentini A. Traumatic diaphragmatic ruptures: clinical presentation, diagnosis and surgical approach in adults. GMS Interdiscip Plast Reconstr Surg DGPW. 2012;1:Doc02.
- Lu J, Wang B, Che X, Li X, Qiu G, He S, Fan L. Delayed traumatic diaphragmatic hernia: a case-series report and literature review. Medicine (Baltimore). 2016;95:e4362.
- Matthews BD, Bui H, Harold KL, Kercher KW, Adrales G, Park A, Sing RF, Heniford BT. Laparoscopic repair of traumatic diaphragmatic injuries. Surg Endosc. 2003;17:254–258.
- Ozpolat B, Kaya O, Yazkan R, Osmanoglu G. Diaphragmatic injuries: a surgical challenge. Report of forty-one cases. Thorac Cardiovasc Surg. 2009;57:358–362.
- Payne JH Jr, Yellin AE. Traumatic diaphragmatic hernia. Arch Surg. 1982;117:18–24.
- Reber PU, Schmied B, Seiler CA, Baer HU, Patel AG, Buchler MW. Missed diaphragmatic injuries and their long-term sequelae. J Trauma. 1998;44:183–188.
- Adamthwaite DN. Penetrating injuries of the diaphragm. Injury. 1982;14:151–158.
- Sattler S, Canty TG Jr, Mulligan MS, Wood DE, Scully JM, Vallieres E, Pohlman T, Karmy-Jones R. Chronic traumatic and congenital diaphragmatic hernias: presentation and surgical management. Can Respir J. 2002;9:135–139.
- Shaw JM, Navsaria PH, Nicol AJ. Laparoscopy-assisted repair of diaphragm injuries. World J Surg. 2003;27:671–674.
- Zantut LF, Ivatury RR, Smith RS, Kawahara NT, Porter JM, Fry WR, Poggetti R, Birolini D, Organ CH Jr. Diagnostic and therapeutic laparoscopy for penetrating abdominal trauma: a multicenter experience. J Trauma. 1997;42:825–829; discussion 829–31.
- Mjoli M, Oosthuizen G, Clarke D, Madiba T. Laparoscopy in the diagnosis and repair of diaphragmatic injuries in left-sided penetrating thoracoabdominal trauma: laparoscopy in trauma. Surg Endosc. 2015;29:747–752.
- Zafar SN, Onwugbufor MT, Hughes K, Greene WR, Cornwell EE 3rd, Fullum TM, Tran DD. Laparoscopic surgery for trauma: the realm of therapeutic management. Am J Surg. 2015;209:627–632.
Keywords:
Diaphragm injuries; practice management guidelines; laparoscopy; thoracoscopy; diaphragm hernia