Femur Fractures, Open Reduction and Internal Fixation, Timing of — Update
Published 2014
Citation: J Trauma. 77(5):787-795, November 2014
Authors
Gandhi, Rajesh R. MD; Overton, Tiffany L. MPH; Haut, Elliott R. MD, PhD; Lau, Brandyn MPH; Vallier, Heather A. MD; Rohs, Thomas MD; Hasenboehler, Erik MD; Lee, Jane Kayle MD; Alley, Darrell MD; Watters, Jennifer MD; Rogers, Frederick B. MD; Shafi, Shahid MD
Author Information
From the Department of Surgery (R.R.G., T.L.O., S.S.), JPS Health Network, Fort Worth; and Department of Surgery (D.A.), East Texas Medical Center, Tyler, Texas; Departments of Surgery (E.R.H., B.L.), and Orthopaedic Surgery (E.H.), The Johns Hopkins University School of Medicine, Baltimore, Maryland; Department of Orthopaedics (H.A.V.), MetroHealth, Cleveland, Ohio; Department of Surgery (T.R.), Borgess Health, Kalamazoo, Michigan; Department of Surgery (J.K.L.), Advocate Medical Group, Chicago, Illinois; Department of Surgery (J.W.), Oregon Health and Science University, Portland, Oregon; and Department of Trauma and Acute Care Surgery (F.B.R.), Lancaster General Health, Lancaster, Pennsylvania.
Submitted: June 16, 2014, Accepted: July 16, 2014.
This study was part of the podium presentation at the 2014 EAST Conference.
Address for reprints: Tiffany L. Overton, MPH, JPS Health Network, Trauma Services, 1500 S Main St, Fort Worth, TX; email: toverton@jpshealth.org.
Objectives
The objective of this guideline was to evaluate the comparative effectiveness of early (<24 hours) versus late (>24 hours) open reduction and internal fixation of an open or closed femur fracture in trauma patients, particularly in preventing mortality, infection, nonunion/malunion, amputation, and venous thromboembolism (VTE). Our PICO [Population, Intervention, Comparator, and Outcome] question is defined as follows:
- Population: trauma patients with an open or closed femur fracture
- Intervention: open reduction and internal fixation within 24 hours of injury
- Comparator: open reduction and internal fixation greater than 24 hours after injury
- Outcomes: mortality, infection, nonunion/malunion, amputation, VTE
Inclusion Criteria For This Review
Study Types
For the purpose of making recommendations, studies included randomized controlled trials (RCTs), prospective observational or retrospective studies, and case-control studies. Only studies pertaining to open reduction and internal fixation of open or closed femur fractures were included.
Participant Types
We included studies with adult patients, any sex, and with no restriction on inclusion of ethnicities or patients with comorbidities. Meta-analyses, case reports, letters, and reviews containing no original data or comments were excluded.
Intervention Type
We included studies comparing open reduction and internal fixation performed within 24 hours from the time of injury to stabilization performed greater than 24 hours after injury.
Outcome Measure Types
An initial list of all relevant outcomes (infection, nonunion/malunion, compartment syndrome, VTE, fat embolism syndrome, regional pain, neurologic impairment, arthritis, hardware failure, impaired function, mortality, or amputation) was generated and distributed to panelists. Eight panelists independently rated the relative importance of each outcome on a 9-point scale ranging from 1 (less important) to 9 (critically important for decision making). The five highest rated outcomes were selected as follows: mortality, infection, VTE, nonunion/malunion, and amputation. A systematic review of the literature was then conducted to identify relevant articles. Each article was evaluated independently by three members of the committee to extract pertinent data. We did not find any articles with data regarding the outcomes of nonunion/malunion and amputation, so these outcomes were excluded from the analysis.
Other outcomes considered were respiratory complications of fixation such as adult respiratory distress syndrome, fat embolism, pneumonia, and other pulmonary dysfunction. However, these outcomes were not included in this review.
Review Methods
Search Strategy
We conducted our literature search and appraisal based on guidelines for systematic reviews. A MEDLINE and Cochrane search was conducted to identify English language human subjects prospective RCTs, non-RCTs, existing systematic reviews, guidelines, case-control, and observational studies published before November 2013. Search terms included (1) femoral fractures, (2) long bone stabilization, (3) timing fixation, (4) delayed fixation, (5) early fixation, (6) immediate fixation, (7) fracture fixation, (8) timing fracture, and (9) timing osteosynthesis, alone or in combination. In addition to the electronic search, the bibliographies of relevant articles and systematic reviews were hand searched to find additional potentially appropriate publications to be included in this review.
Study Selection
A single panelist conducted the literature search and assessed the titles and abstracts to identify relevant publications, applying inclusion criteria. We excluded case reports and review articles. The resulting studies then underwent full-text review by three independent reviewers to determine appropriateness for inclusion.
Data Extraction and Management
Data were extracted by a single reviewer, confirmed by two other reviewers, and entered into Review Manager X.6 (RevMan). Information included authorship, publication year, methodology of the study, population, intervention, and relevant outcome measures.
Methodological Quality Assessment
The articles were evaluated using the GRADE system.[27–40] The quality of evidence was classified as high, moderate, low, or insufficient for each outcome. The quality of evidence is reflected as the extent to which one can be confident that an estimate of effect is correct and includes an explicit consideration of the following domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias.[31–36] Recommendations were developed based on the results of the meta-analysis as well as the quality of evidence, and per the GRADE approach, they were classified as either “strong” or “weak”.[41] A strong recommendation, prefaced by the statement “we strongly recommend,” indicates that the panel is certain the desirable consequences of a course of action outweigh the undesirable effects in most patients. A weak recommendation, prefaced by the statement “we conditionally recommend,” indicates that the panel concludes the desirable effects of adherence to a recommendation probably outweighed the undesirable effects but it was not as confident. These recommendations were based on the quality of evidence and the risk-versus-benefit ratio.
Measures of Treatment Effect
We created a detailed set of evidence tables containing all abstracted information. Clinical outcomes, including mortality, infection, and VTE reported in each included study, were individually pooled for meta-analysis. The relative risk (RR) and 95% confidence interval (CI) were calculated for each study using a random-effects model.[42] A p < 0.05 was considered significant for all analyses. STATA 12.1 (College Station, TX) statistical analysis software was used for all statistical analyses.[43] There were not enough data to undertake meta-analysis for the other two outcomes (nonunion/malunion and amputations).
Assessment of Heterogeneity
Potential heterogeneity existed because of population differences, different types of surgery, and how patients were defined. We examined these differences across studies to assess clinical and methodological heterogeneity. For the meta-analysis, we used RevMan to calculate the I[2] statistic to determine the proportion of variation between studies attributable to heterogeneity, and variation was categorized as “low” (I[2] = 25–49%), “moderate” (I[2] = 50–74%), or “high” (I[2] = 74–100%).
Results

Figure 1: Flow diagram of included and excluded studies.
We retrieved 9,091 articles during the first phase of the literature search, of which 9,032 were excluded by duplicate removal and title review (Fig. 1). Fifty-nine articles addressing optimal timing of long bone fracture stabilization underwent a full review to identify 11 studies comparing early (<24 hours) versus late (>24 hours) open reduction and internal fixation of femur fractures in trauma patients (Table 1). Of the 11 studies, 1 was a prospective randomized study[5] and 10 were retrospective cohort studies.[11][15][19][21–23][44–47] Across all studies, 7,189 patients were included, with 5,064 receiving early stabilization and 2,125 receiving late stabilization.
Participant Characteristics
The range of the mean ages in the studies reviewed was 18 years to 43 years. Most of the patients were men (61–78%). The mean Injury Severity Score (ISS) for patients receiving early stabilization ranged from 12 to 27, while patients receiving late stabilization ranged from 12 to 34 (Table 1).
Results By Outcome
Mortality
Eight studies reported the incidence of mortality,[5][11][19][21–23][44][45] one of which was a prospective randomized study (Fig. 2).[5] These studies included 6,930 patients (sample size range, 22–3,069). A meta-analysis of these eight studies showed no difference in mortality among patients with early stabilization compared with those undergoing late stabilization (RR, 0.74; 95% CI, 0.50–1.08; p = 0.313). Of note, the I[2] statistic was 15%, falling into the “low” heterogeneity category, indicating that the studies were comparable. In the only RCT, early internal fixation, there were only three total deaths (two in the early and one in the late cohort), which was not statistically significantly different.[5]
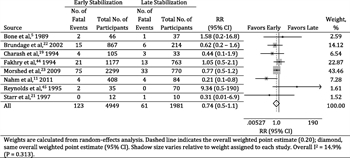
Figure 2: Forest plot of RR of mortality with early (<24 hours) versus late (>24 hours) femur fracture stabilization in trauma patients.
Infection
We included three studies reporting on infection and included 667 patients (sample size range, 68–492) (Fig. 3).[11][15][46] A meta-analysis of these three studies showed no difference in infection between patients undergoing early surgery compared with those undergoing late surgery (RR, 0.40; 95% CI, 0.10–1.60; p = 0.888). The I[2] statistic was “low” at 0%, although this is likely caused by the wide CIs of each study rather than a true homogeneity between the studies.
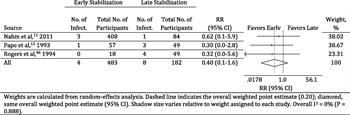
Figure 3: Forest plot of RR of infection with early (<24 hours) versus late (>24 hours) femur fracture stabilization in trauma patients.
Venous Thromboembolism
We included six studies reporting on VTE and included 1967 patients (sample size range, 67–1,081),[5][11][15][19][22][46] including the previously mentioned prospective randomized study (Fig. 4).[5] A meta-analysis of these six studies showed no difference in VTE between patients undergoing early surgery compared with those undergoing late surgery (RR, 0.63; 95% CI, 0.37–1.07; p = 0.896). The I2 statistic was “low” at 0%, although this is likely caused by the wide CIs of each study rather than a true homogeneity between the studies.
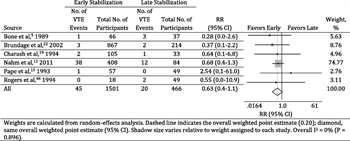
Figure 4: Forest plot of RR of VTE with early (<24 hours) versus late (>24 hours) femur fracture stabilization in trauma patients.
Nonunion/Malunion
Only one study reported nonunion/malunion outcomes, resulting in insufficient evidence to perform a meta-analysis for this outcome.[47] This study compared patients treated within 24 hours of their injury at their hospital with patients from another hospital who were treated greater than 24 hours after injury. They found delayed fixation resulted in more callus and more frequent secondary bone healing. In both patient groups, however, there were no nonunions or malunions reported.
Amputation
Only one study reported amputation outcomes, resulting in insufficient evidence to perform a meta-analysis for this outcome.[15] This study retrospectively reviewed outcomes for multiple trauma patients with femoral shaft fractures based on the presence of additional severe thoracic injuries. Only two patients in each stabilization group (early vs. late) required amputation (early, 3.4%; late, 4.1%).
Grading the Evidence
With the use of the GRADE framework for assessing all relevant outcomes, no serious risk of inconsistency or indirectness was found. However, moderate imprecision was noted since the studies were small and CIs were large. We rated the prospective randomized study as having a moderate risk of bias, primarily based on study design.[5] Among the retrospective studies, we rated only one study as having a moderate risk of bias[23] and the remainder as having a high risk of bias. Starting from observational studies (which are considered low quality), we did not rate up for the quality of evidence.
We rated the strength of evidence as low to support a reduction in mortality, infection, and VTE in trauma patients treated with early stabilization relative to late stabilization (Table 2). We rated the strength of evidence as insufficient to support any increase or decrease in nonunion/malunion or amputation in trauma patients treated with early stabilization relative to late stabilization (Table 3).
Discussion
The findings of this study indicate that internal fixation of femur fractures in less than 24 hours after injury may be associated with a reduction in mortality, infection, and VTE. There was insufficient evidence to comment on the outcomes of amputation or nonunion/malunion. The studies reviewed did not separate outcomes of open from closed fractures. Hence, this recommendation applies to all femur fractures. Unlike the previous EAST PMG on long bone fractures, all other long bones, including tibia, were excluded from this analysis.
A major implication of this study is that early fracture fixation should be considered in all patients with femur fractures. In the absence of a clear contraindication to surgery or anesthesia, the recommendation of this review, although conditional, should prompt early fixation. However, the surgical decision must be individualized to each patient’s needs. Delayed treatment has been associated with improved survival rates among patients with serious abdominal injuries and a reduction in adverse outcomes in patients with multiple injuries.[13] In addition, delayed stabilization (24–48 hours) may be safer than stabilization within 12 hours for severely injured patients.[48]
Of the large number of articles reviewed, there was only one prospective randomized trial addressing the issue of early versus late fixation of femur fractures.[5] The total number of patients in this study (83) was relatively small. The only outcomes of interest with respect to this PMG were mortality and VTE. Among the other outcomes reported in this study, the early fixation arm had significantly shorter stay in the intensive care unit and in the hospital. As a result of the lower length of stay, the average hospital cost was also decreased in the early fixation arm.
The rest of the other articles reviewed were retrospective reviews. Hence, patients were not matched in early versus delayed fixation groups. Another issue was inconsistent timing of fracture fixation. In many articles, the time of fixation was less than 48 hours and not further specified. These were not included in the analysis. One article reported fixation less than 12 hours or greater than 48 hours.[49] Another article excluded all patients who had fixation after 48 hours. In addition, there were variations in the fracture type. We specifically excluded studies with intertrochanteric fracture fixation.[50] One article was excluded because patients with femur fractures were not separated from pelvis and spine fractures.[51] Other articles were excluded as they compared the type of fixation, instead of the timing of fixation. Pediatric studies were also excluded. Finally, all case series with four or fewer cases were excluded.
Some of the articles reported damage-control orthopedics compared with definitive fixation. These articles had external fixation performed early, followed by definitive internal fixation later on. These articles were also excluded because their patients did not have internal fixation within 24 hours. Another major common reason for exclusion was that the outcomes reported were not relevant to this review, namely, mortality, infection, VTE, nonunion/malunion, and amputation. One of the items not considered was economics. However, it seems early fixation did lead to an efficient use of operating room and other resources compared with delayed fixation.[5][46]
This PMG has several limitations primarily related to the study design resulting in a high risk of bias in all but two studies, resulting in a conditional recommendation. In addition, we were unable to separate open from closed femoral fractures. The findings are also limited to the five outcomes included in the literature review. No inference should be made about other outcomes such as fat embolism, compartment syndromes, and functional outcomes.
Recommendation
In trauma patients with open or closed femur fractures, we suggest early (<24 hours) open reduction and internal fracture fixation. This recommendation is conditional because the strength of the evidence is low. Early stabilization of femur fractures shows a trend (statistically insignificant) toward lower risk of infection, mortality, and VTE. Therefore, the panel concludes that the desirable effects of early femur fracture stabilization probably outweigh the undesirable effects in most patients. Additional well-designed observational or prospective cohort studies may be informative. Although the overall quality of evidence was low, the other factors GRADE allows the writing committee to consider helped to guide our recommendation. The potential patient benefit of early femur fixation likely outweighs the harm in most patients.
Recommendation
In trauma patients with open or closed femur fractures, we suggest early (<24 hours) open reduction and internal fracture fixation. This recommendation is conditional, and the strength of the evidence is low. Early stabilization of femur fractures shows a trend (statistically insignificant) toward lower risk of infection, mortality, and VTE. Therefore, the panel concludes that the desirable effects of early femur fracture stabilization probably outweigh the undesirable effects in most patients. Conditional recommendation (low quality of evidence).
Using These Guidelines In Clinical Practice
This guideline represents a very detailed summary of the literature regarding open reduction and internal fixation of femur fractures and surgical timing and is meant to inform the decision-making process, not replace clinical judgment. The optimal timing for internal fixation remains controversial.[2–4] The literature available for review thus far support the course of earlier open reduction and internal fixation in polytrauma patients with open or closed femur fractures.
Conclusion
In conclusion, we conditionally recommend internal fixation of femur fractures in less than 24 hours from the time of injury to reduce mortality, infection, and VTE. Further research in a well-designed fashion with adequate sample size is needed to determine the benefits of early fixation of femur fractures.
Authorship
R.R.G., S.S. and E.R.H. conceived the study. R.R.G. built the PICO questions. J.K.L., D.A., J.W., T.R., E.H., F.B.R., S.S., and R.R.G. voted regarding the outcomes of interest for the PICO questions. R.R.G., S.S., and T.L.O. evaluated the articles independently for outcomes and relevance. T.L.O. performed the entire literature search, read all the abstracts, and selected the articles for review. R.R.G., S.S., and T.L.O. reviewed and summarized those articles selected. T.L.O. extracted the data from those articles. E.R.H. and B.L. placed the extracted data in the RevMan and GRADEpro programs and evaluated the results for recommendations. R.R.G., S.S., and T.L.O. also evaluated the results for the recommendation. R.R.G., S.S., and T.L.O. wrote the manuscript. E.R.H. and B.L. contributed to the writing of the methods and results. All authors participated in the critical review of this article.
Acknowledgment
We thank the Eastern Association for the Surgery of Trauma (EAST) and the EAST foundation for the opportunity to write this article, the specialized training provided to the writers regarding the GRADE method, and the detail-oriented peer review of multiple versions of this article by the guidelines committee.
Disclosure
E.R.H. is the primary investigator and supported by a contract (CE-12-11-4489) from the Patient-Centered Outcomes Research Institute (PCORI) entitled “Preventing Venous Thromboembolism: Empowering Patients and Enabling Patient-Centered Care Via Health Information Technology.” E.R.H. receives royalties from Lippincott, Williams, & Wilkins for a book, “Avoiding Common ICU Errors” and has given expert witness testimony in various medical malpractice cases. E.R.H. is a member of the EAST Board of Directors and Chairs the EAST Guidelines Committee. R.R.J. is a speaker for Lifecell. E.H. is supported by grants from Synthes and Smith and Nephew and is a consultant for Synthes. E.H. is also a speaker for AO North America Faculty. B.L. is the co–principal investigator of a contract (CE-12-11-4489) with the Patient-Centered Outcomes Research Institute (PCORI) entitled “Preventing Venous Thromboembolism: Empowering Patients and Enabling Patient-Centered Care Via Health Information Technology.” H.A.V. is a member of the board for the Orthopaedic Trauma Association and Center for Orthopaedic Trauma Advancement. H.A.V. receives support for the METRC research consortium funded by the Department of Defense, the FAITH research study funded by the National Institute of Health, and the sacrum research study funded by the Orthopaedic Trauma Association. J.W. is supported by a grant to study acupuncture in the ICU by the Medical Research Foundation and receives travel expenses for PROPPR trial meetings. S.S., F.B.R., T.R., D.A., J.K.L., and T.L.O. have nothing to disclose.
References
- Giannoudis PV, Papakostidis C, Roberts C. A review of the managment of open fractures of the tibia and femur. J Bone Joint Surg. 2006; 88: 281–289.
- Kaltenecker G, Wruhs O, Quaicoe S. Lower infection rate after interlocking nailing in open fractures of the femur and tibia. J Trauma. 1990; 30: 474–490.
- Williams MM, Askins V, Hinkes EW, Zych GA. Primary reamed intramedullary nailing of open femoral shaft fractures. Clin Orthop. 1995; 318: 182–190.
- Baixauli F Sr, Baixauli AJ, Sanchez-Alepuz E, Baixauli F. Interlocked intramedullary nailing for treatment of open femoral shaft fractures. Clin Orthop. 1998; 350: 67–73.
- Bone LB, Johnson KD, Weigelt J, Schienberg R. Early versus delayed stabilization of femoral fractures. J Bone Joint Surg. 1989; 71: 336–340.
- Dunham CM, Bosse MJ, Clancy TV, et al. Practice management guidelines for the optimal timing of long-bone fracture stabilization in polytrauma patients: the EAST Practice Management Guidelines Work Group. J Trauma. 2001; 50: 958–967.
- Seibel R, LaDuca J, Hassett JM, et al. Blunt multiple trauma (ISS 36), femur traction, and the pulmonary failure-septic state. Ann Surg. 1985; 202: 283–295.
- Giannoudis PV, Veysi VT, Pape HC, et al. When should we operate on major fractures in patients with severe head injuries? Am J Surg. 2002; 183: 261–267.
- Labeeu F, Pasuch M, Toussaint P, et al. External fixation in war traumatology. J Trauma. 1996; 40: 223–227.
- Gregory P, Sanders R. The management of severe fractures of the lower extremities. Clin Orthop. 1995; 318: 95–105.
- Nahm NJ, Como JJ, Wilber JH, Vallier HA. Early appropriate care: definitive stabilization of femoral fractures within 24 hours of injury is safe in most patients with multiple injuries. J Trauma. 2011; 71: 175–185.
- Behrman SW, Fabian TC, Kudsk KA., Taylor JC. Improved outcome with femur fractures: early vs delayed fixation. J Trauma. 1990; 30: 792–797.
- Poole GV, Miller JD, Agnew SG, Griswold JA. Lower extremity fracture fixation in head-injured patients. J Trauma. 1992; 32:(5): 654–659.
- Pape HC, Regel G, Dwenger A, Sturm JA, Tscherne H. Influence of thoracic trauma and primary femoral intramedullary nailing on the incidence of ARDS in multiple trauma patients. Injury. 1993; 24: S82–S103.
- Pape HC, Auf’m’Kolk M, Paffrath T, Regel G, Sturm JA, Tscherne H. Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion—a cause of posttraumatic ARDS? J Trauma. 1993; 34: 540–548.
- Jaicks RR, Cohn SM, Moller BA. Early fracture fixation may be deleterious after head injury. J Trauma. 1997; 42: 1–5.
- Townsend RN, Lheureau T, Protech J, Reimer B, Simon D. Timing fracture repair in patients with severe brain injury (Glasgow Coma Scale score < 9). J Trauma. 1998; 44: 977–982.
- Ziran BH, Le T, Zhou H, Fallon W, Wilber JH. The impact of the quantity of skeletal injury on mortality and pulmonary morbidity. J Trauma. 1997; 43: 916–921.
- Charash WE, Fabian TC, Croce MA. Delayed surgical fixation of femur fractures is a risk factor for pulmonary failure independent of thoracic trauma. J Trauma. 1994; 37: 667–672.
- Bosse MJ, MacKenzie EJ, Riemer BL, et al. Adult respiratory distress syndrome, pneumonia, and mortality following thoracic injury and femoral fracture treated either with intramedullary nailing with reaming or with a plate. A comparitive study. J Bone Joint Surg. 1997; 79: 799–809.
- Starr AJ, Hunt JL, Chason DP, Reinert CM, Walker J. Treatment of femur fracture with associated head injury. J Orthop Trauma. 1998; 12: 38–45.
- Brundage SI, McGhan R, Jurkovich GJ, Mack CD, Maier RV. Timing of femur fracture fixation: effect on outcome in patients with thoracic and head injuries. J Trauma. 2002; 52:(2): 299–307.
- Morshed S, Miclau T, Bembom O, Cohen M, Knudson MM, Colford JM. Delayed internal fixation of femoral shaft fracture reduces mortality among patients with multisystem trauma. J Bone Joint Surg. 2009; 91: 3–13.
- Scalea TM, Scott JD, Brumback RJ, et al. Early fracture fixation may be “just fine” after head injury: no difference in central nervous system outcomes. J Trauma. 1999; 46: 839–846.
- Weninger P, Figl M, Spitaler R, Mauritz W, Hertz H. Early unreamed intramedullary nailing of femoral fractures is safe in patients with severe thoracic trauma. J Trauma. 2007; 62: 692–696.
- Kerwin AJ, Haut ER, Burns JB, et al. Eastern Associaiton for the Surgery of Trauma Practice Management Guidelines Ad Hoc Committee. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012; 73:(5): S283–S287.
- Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011; 64: 383–394.
- Guyatt G, Oxman AD, Sultan S, et al. GRADE guidelines 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. 2012 .
- Guyatt GH, Oxman AD, Schunemann HJ. GRADE guidelines-an introduction to the 10th–13th articles in the series. J Clin Epidemiol. 2012 .
- Brunetti M, Shemilt I, Pregno S, et al. Grade guidelines: 10. Considering resource use and rating the quality of economic evidence. J Clin Epidemiol. 2012 .
- Guyatt G, Oxman AD, Kunz R, et al. GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol. 2011; 64: 1294–1302.
- Guyatt G, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol. 2011; 64: 1294–1302.
- Guyatt G, Oxman AD, Montori V, et al. GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol. 2011; 64: 1277–1282.
- Guyatt G, Oxman AD, Kunz R, et al. GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol. 2011; 64: 1303–1310.
- Guyatt G, Oxman AD, Sultan S, et al. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol. 2011; 64: 1311–1316.
- Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J Clin Epidemiol. 2011; 64: 407–415.
- Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011; 64: 401–406.
- Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011; 64: 380–382.
- Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011; 64: 395–400.
- Schunemann HJ, Oxman AD, Brozek J, et al. GRADE: assessing the quality of evidence for diagnostic recommendations. ACP J Club. 2008; 149: 2
- Guyatt GH, Oxman AD, Kunz R, et al. GRADE Working Group. Going from evidence to recommendations. Br Med J. 2008; 336:(7652): 1049–1051.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7: 177–188.
- Stata Statistical Software: Release 12 [computer program]. College Station, Tx: StataCorp LP; 2011 .
- Fakhry SM, Rutledge R, Dahners LE, Kessler D. Incidence, management, and outcome of femoral shaft fracture: a statewide population-based analysis of 2805 adult patients in a rural state. J Trauma. 1994; 37:(2): 255–261.
- Reynolds MA, Richardson JD, Spain DA, Seligson D, Wilson MA, Miller FB. Is the timing of fracture fixation important for the patient with multiple trauma? Ann Surg. 1995; 222: 470–481.
- Rogers FB, Shackford SR, Vane DW, Kaups KL, Harris F. Prompt fixation of isolated femur fractures in a rural trauma center: a study examining the timing of fixation and resource allocation. J Trauma. 1994; 36: 774–777.
- van Niekerk JLM, ten Duis JH, Binnendijk B. Duration of fracture healing after early versus delayed internal fixation of fractures of the femoral shaft. Injury. 1987; 18: 120–122.
- Cantu RV GS, Spratt KF. In-hospital mortality from femoral shaft fracture depends on the initial delay to fracture fixation and Injury Severity Score: a retrospective cohort study from the NTDB 2002–2006. J Trauma Acute Care Surg. 2014; 76:(6): 1433–1440.
- Debrauwer S, Hendrix K, Verdonk R. Anterograge femoral nailing with a reamed interlocking titanium alloy nail. Acta Orthop Belg. 2000; 66: 484–489.
- Davis TRC, Sher JL, Porter BB, Checketts RG. The timing of surgery for interochanteric femoral fractures. Injury. 1988; 19: 244–246.
- Johnson KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress syndrome in patients with multiple musculoskeletal injuries: effect of early operative stabilization of fractures. J Trauma. 1985; 25: 375–384.
Previous version of this guideline
Long Bone Fracture Stabilization in Polytrauma Patients
Tables
Table 1
Characteristics of Studies of Early Versus Late Internal Fixation of Femur Fracture Among Trauma Patients
|
|
No. Patients |
Mean Age, y |
Male Sex, % |
Mean ISS |
|||||
|
Source |
Design |
Early |
Late |
Early |
Late |
Early |
Late |
Early |
Late |
|
Bone et al.,[5] 1989 |
PR |
46 |
37 |
27 |
29 |
78 |
68 |
22 |
20 |
|
Brundage et al.,[22] 2002 |
RO |
867 |
214 |
28 |
30 |
70 |
70 |
17 |
19 |
|
Charash et al.,[19] 1994 |
RO |
105 |
33 |
31 |
30 |
NR |
NR |
12 |
28 |
|
Fakhry et al.,[44] 1994 |
RO |
1,177 |
763 |
NR |
NR |
NR |
NR |
12 |
12 |
|
Morshed et al.,[23] 2009 |
RO |
2,299 |
770 |
32 |
34 |
NR |
NR |
27 |
31 |
|
Nahm et al.,[11] 2011 |
RO |
408 |
84 |
35 |
43 |
74 |
69 |
22 |
34 |
|
Pape et al.,[15] 1993 |
RO |
57 |
49 |
28 |
27 |
NR |
NR |
24 |
29 |
|
Reynolds et al.,[45] 1995 |
RO |
35 |
70 |
33 |
33 |
74 |
64 |
27 |
33 |
|
Rogers et al.,[46] 1994 |
RO |
18 |
49 |
37 |
38 |
61 |
69 |
NR |
NR |
|
Starr et al.,[21] 1997 |
RO |
12 |
10 |
38 |
33 |
NR |
NR |
27 |
26 |
|
van Niekerk et al.,[47] 1987 |
RO |
40 |
46 |
18 |
19 |
75 |
74 |
NR |
NR |
Table 2
Strength of Evidence for Early (G24 Hours) Versus Late (924 Hours) Stabilization of Femur Fractures in Trauma Patients
|
Outcome, Source |
Risk of Bias |
Strength of Evidence and Magnitude of Effect,% |
|
Mortality
|
Low that early femur fracture stabilization is associated with lower incidence of mortality in trauma patients compared with late femur fracture stabilization; RR, 0.74 (95% CI, 0.50Y1.08; I2 = 14.9%) |
|
|
Bone et al.,[5] 1989 |
Moderate |
4.3 vs. 2.7 |
|
Brundage et al.,[22] 2002 |
High |
1.7 vs. 2.8 |
|
Charash et al.,[19] 1994 |
High |
3.8 vs. 9.1 |
|
Fakhry et al.,[44] 1994 |
High |
1.8 vs. 1.7 |
|
Morshed et al.,[23] 2009 |
Moderate |
3.3 vs. 4.3 |
|
Nahm et al.,[11] 2011 |
High |
1.0 vs. 4.8 |
|
Reynolds et al.,[45] 1995 |
High |
5.7 vs. 0 |
|
Starr et al.,[21] 1997 |
High |
0 vs. 10.0 |
|
Infection
|
Low that early femur fracture stabilization is associated with lower incidence of infection in trauma patients compared with late femur fracture stabilization; RR, 0.40 (95% CI, 0.10Y1.60; I2 = 0%) |
|
|
Nahm et al.,[11] 2011 |
High |
0.7 vs. 1.2 |
|
Pape et al.,[15] 1993 |
High |
1.8 vs. 6.1 |
|
Rogers et al.,[46] 1994 |
High |
0 vs. 8.2 |
|
Nonunion/Malunion |
Insufficient that early femur fracture stabilization is associated with lower incidence of nonunion/ malunion in trauma patients compared with late femur fracture stabilization. |
|
|
van Niekerk et al.,[47] 1987 |
High |
0 vs. 0 |
|
Amputation |
Insufficient that early femur fracture stabilization is associated with lower incidence of amputation in trauma patients compared with late femur fracture stabilization |
|
| Pape et al.,[15] 1993 | High | 3.5 vs. 4.1 |
| VTE |
Low that early femur fracture stabilization is associated with lower incidence of VTE in trauma patients compared with late femur fracture stabilization; RR, 0.63 (95% CI, 0.37Y1.07; I2 = 0%) |
|
| Bone et al.,[5] 1989 | Moderate | 2.2 vs. 8.1 |
| Brundage et al.,[22] 2002 | High | 0.3 vs. 0.9 |
| Charash et al.,[19] 1994 | High | 1.9 vs. 3.0 |
| Nahm et al.,[11] 2011 | High | 9.3 vs. 14.3 |
| Pape et al.,[15] 1993 | High | 1.8 vs. 0 |
| Rogers et al.,[46] 1994 | High | 0 vs. 4.1 |
Table 3
Outcomes Among Trauma Patients With Femur Fractures Who Received Early (G24 Hours) Versus Late (924 Hours) Open Reduction and Internal Fixation
|
|
No. Patients |
Mortality |
Infection |
Nonunion/ Malunion |
Amputation |
VTE |
||||||
|
Study |
Early |
Late |
Early |
Late |
Early |
Late |
Early |
Late |
Early |
Late |
Early |
Late |
|
Bone et al.,[5] 1989 |
46 |
37 |
2 |
1 |
nr |
nr |
nr |
nr |
nr |
nr |
1 |
3 |
|
Brundage et al.,[22] 2002 |
867 |
214 |
15 |
6 |
nr |
nr |
nr |
nr |
nr |
nr |
3 |
2 |
|
Charash et al.,[19] 1994 |
105 |
33 |
4 |
3 |
nr |
nr |
nr |
nr |
nr |
nr |
2 |
1 |
|
Fakhry et al.,[44] 1994 |
1,177 |
763 |
21 |
13 |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
|
Morshed et al.,[23] 2009 |
2,299 |
770 |
75 |
33 |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
|
Nahm et al.,[11] 2011, |
408 |
84 |
4 |
4 |
3 |
1 |
nr |
nr |
nr |
nr |
38 |
12 |
|
Pape et al.,[15] 1993 |
57 |
49 |
nr |
nr |
1 |
3 |
nr |
nr |
2 |
2 |
1 |
0 |
|
Reynolds et al.,[45] 1995 |
35 |
70 |
2 |
0 |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
|
Rogers et al.,[46] 1994 |
18 |
49 |
nr |
nr |
0 |
4 |
nr |
nr |
nr |
nr |
0 |
2 |
|
Starr et al.,[21] 1997 |
12 |
10 |
0 |
1 |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
nr |
|
van Niekerk et al.,[47] 1987 |
40 |
46 |
nr |
nr |
nr |
nr |
0 |
0 |
nr |
nr |
nr |
nr |