Hospital-Based Violence Intervention Programs Targeting Adult Populations
Published 2016
Citation: Trauma Surgery & Acute Care Open (doi:10.1136/tasco-2016-000024)
Authors
Steven Affinati, Desmond Patton, Luke Hansen, Megan Ranney, A Britton Christmas, Pina Violano, Aparna Sodhi, Bryce Robinson, Marie Crandall, from the Eastern Association for the Surgery of Trauma Injury Control and Violence Prevention Section and Guidelines Section
Background
After falling dramatically in the 1990s, national fatal and non-fatal violent crime and injury rates have plateaued in the USA.[1],[2] Though national trends stabilized since the turn of the millennium, specific under-resourced ethnicities continue to incur higher incidences of intentional violent injury.[3–10] An acute violent injury treated in the emergency department often represents the ‘primary or sole access point to the healthcare system’[11] for those most at risk for intentional violent reinjury.[12] Once discharged from the hospital, nearly 50% of patients injured by violence will suffer violent reinjury.[3],[4],[6],[13–18] These patients often suffer not only acute physical but also psychological wounds, including trauma-related and stressor-related maladies such as post-traumatic stress disorder (PTSD) and acute stress disorder (ASD).[11],[19],[20]
Intentional violent injury and re-injury also incur substantial economic and societal cost.[3–5],[21],[22] Lee et al[21] estimated that in 2010 the economic cost, defined as ‘direct medical services and lost productivity’ per non-fatal firearm injury for patients admitted to the hospital was over US$423 813, and for those discharged from the emergency department the cost was estimated at US$122 372. Approximately 75% of violent injury cases involve uninsured and underinsured patients.5 In total, the annual societal cost of firearm injury in the USA is estimated to be US$174.1 billion.[21]
Trauma surgeons have taken an active role in describing the risk factors and consequences of violent injury. Livingston et al has described the scope and burden of gunshot wound (GSW) injuries in their communities, demonstrating significant clustering and repeat injury.[23] Many other trauma centers, including University of California San Francisco and University of Pennsylvania, have taken active approaches to violence prevention. Hospital-based violence intervention programs (HVIPs) have emerged nationwide to help address the societal and economic costs of violence. The goal of these programs is to intervene with those individuals who survive violent injury, at this ‘sole access point’ into the healthcare system.[4] In addressing ‘the psychosocial challenges that these patients face’,[8] HVIPs are designed to interrupt the costly cycles of violent injury by transforming medical treatment into a catalyst for life and societal change.[8],[24]
Such programs propose to take advantage of the convergence of intentional violent injury and exposure to the health system, or ‘teachable moments’,[8],[24] to affect potential behavior change. HVIPs often provide peer-based, community-based and/or hospital-based case management.[8] In addition to other services, HVIPs may involve family or group therapy, substance abuse treatment, and/or training in emotional regulation skills. Although there is no standard HVIP, all offer significant additional resources after a patient's treatment for a violent injury.
Despite strong theoretical underpinnings for HVIPs, to date the literature regarding the efficacy and effectiveness of HVIPs remains poorly delineated. To better understand the characteristics of and data regarding HVIPs, we undertook a systematic review of the literature applying the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology[25],[26] to critical appraisal of the evidence.
Objectives
The objective of this evidence-based review (EBR) was to evaluate the preventive efficacy of HVIPs in adult patients (age 18+) treated for intentional violent injury. This population limitation was chosen because males (especially if African-American, unemployed, and uninsured) aged 25–31 are at high risk for intentional violent trauma recidivism.[6],[11],[15],[16] Understanding that violent injury prevention in adult populations has been less well studied than among youth, the writing team's leadership (MC, LH, SA) a priori created the populations (P), intervention (I), comparator (C), and outcome (O), or PICO question. Given the complex multitude of variables pertaining to transnational political, social, and cultural heterogeneity, this review's objective was restricted to the USA. Our injury outcomes of interest were violent reinjury and other reinjury. Both were considered to be equivalent in terms of impact and deemed critically important by all group members (GRADE rank order 9 for both). Secondary outcomes were deemed important and were also included: job attainment, educational attainment, legal conflicts such as arrest or incarceration, mental health and substance abuse issues, and quality of life (GRADE rank order 7 for all).
PICO questions
- Population: Adult victims of intentional violent trauma.
- Intervention: Any trauma center, emergency department, or hospital-based postinjury violence intervention program.
- Comparator: Usual standard of care.
- Outcomes: Intentional violent injury reinjury and/or death, job and/or school attainment, arrest and/or incarceration, substance abuse and/or mental health issues, and quality of life.
Are HVIPs attending to adult patients (age 18+) treated for intentional violent injury more effective than the usual standard care in improving the following outcomes: intentional violent injury reinjury and/or death; arrest and/or incarceration; substance abuse and/or mental issues; quality of life; job and/or school attainment? (PICO 1).
Methods
Inclusion criteria for this review
Study types
Studies included randomized controlled trials, prospective and retrospective observational studies, and case–control studies. Case reports, conceptual pieces, and reviews containing no original data or analyses were excluded. Additionally, any papers on child abuse, sexual assault, and/or intimate partner violence were excluded. Studies were limited to those written in English and conducted in the USA. No limitations were put on year of publication.
Review methods
Search strategy
A research librarian aided our systematic search of PubMed, Web of Science, Google Scholar, and the Cochrane Library. After a preliminary query, we chose to apply the following PubMed search string: (“Violence”[Mesh] AND (“Recurrence”[Mesh] OR recur* OR recidivism) AND “Health Facilities”[Mesh] AND (prevention OR intervention*). We then inspected each review article's reference section. No restrictions were placed on either language or dates. We did, however, only include studies in the USA. Figure 1 contains the MeSH terms used for the initial search. Eight months later a research assistant member of the writing team (SA) performed a unique and independent systematic search. Two new articles were found, neither of which met the PICO question criteria. Finally, in January 2016, an institutional research librarian performed a literature search which found two additional relevant articles, and these articles were included in our literature review.
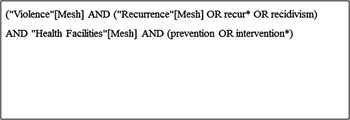
Figure 1. MeSH search terms.
Study selection
After completing an exhaustive literature search, three independent reviewers (LH, PV, MC) and a research assistant (SA) screened the titles and abstracts, excluding reviews, case reports, youth-focused articles, and unrelated articles. The articles identified in 2016 were screened by a single reviewer (MC) for inclusion. The resulting studies were used for the review. The study selection process is highlighted in the PRISMA flow diagram for figure 2.
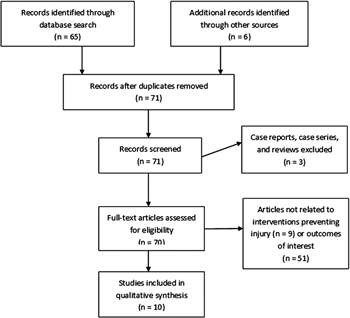
Figure 2. PRISMA flow diagram.
A total of 71 abstracts were identified by our search. Of these, zero were duplicates, three were excluded after title review, and one more was identified after abstract review. Of the 25 articles selected for full review, our team found that 8 met our predetermined criteria.[6],[12],[16],[22],[23],[27–29] The remaining articles were either entirely or primarily youth focused (meaning participants were under the age of 18) or were reviews themselves and were therefore excluded from our final data analysis. The subsequent literature search in 2016 found two more articles, bringing the total article number of reviewed articles to 10.
Data extraction and management
All articles, GRADE resources, and instructions were electronically available to all members of the writing team. Each independent reviewer shared his or her PICO sheet and literature review with all members of the team. Independent interpretations of the data were shared through group email, conference calls, and in-person discourse. No major reviewer discrepancies in grading occurred. Had they occurred, we would have used a modified Delphi technique to resolve differences.
Methodological quality assessment
We used the validated GRADE methodology for this study.[25],[26] The GRADE methodology entails the creation of a predetermined PICO question or set of PICO questions that the literature must answer. Each designated reviewer independently evaluates the data in aggregate with respect to the quality of the evidence to adequately answer each PICO question and quantified the strength of any recommendations. Reviewers are asked to determine effect size, risk of bias, inconsistency, indirectness, precision, and publication bias.
Recommendations are based on the overall quality of the evidence on the participant. GRADE methodology suggests the phrases, ‘we recommend’ for strong evidence, and ‘we suggest’ or ‘we conditionally recommend’ for weaker evidence.
Results
After applying validated GRADE methods, the quality of evidence proved too weak to warrant a separate assessment of interventional efficacy for each outcome.
All 10 included in our synthesis were in English. Three study sites published more than one article on their programs. As a result, six metropolitan areas were represented: Richmond, Virginia; Baltimore, Maryland; Indianapolis, Indiana; San Francisco, California; Oakland, California; and Chicago, Illinois.
Of the 10 papers, 4 were randomized clinical trials (RCTs) and 6 were observational studies: 1 prospective and 5 retrospective, including 2 cost-effectiveness analyses. Six of eight studies had an average age between 17.5 and 21, and one paper required participants to be 18 years of age and older. The authors of this review were unable to identify the average age for one of the articles included in our synthesis.
Measured outcomes and frequency of measurement in the identified articles were as follows: arrest and/or incarceration (7); intentional violent injury recidivism and/or death (7); employment and/or education (2); and substance abuse (1). One RCT measured attitudes about violence. No study measured postintervention mental health or quality of life.
Of the seven articles reporting measurements of intentional violent injury recidivism and/or death, four demonstrated no effect (among three original sample pools).[6],[18],[30],[31] Three studies consisting of three unique sample pools suggested a positive interventional impact on intentional violent injury recidivism and/or death: Gomez et al[32] noted a 1-year reinjury reduction rate from 8.7% to 2.9%.[32] Cooper et al[14] wrote that their “nonintervention group was six times more likely than intervention group to be hospitalized as a result of a violent injury.” Smith et al[24] reported a 16–4% reduction in intentional violent reinjury. The three studies with a positive outcome had low sample sizes (combined n=254).[14],[24],[32] One of these studies did not report how outcomes were assessed;[14] and another was limited by its historical comparison control group and the exclusion of inactive participants when measuring success.[24]
No study demonstrated statistical significance for reduction in violent reinjury. Among the eight studies in this review, the largest had 154 participants, however its a priori calculation suggested that 600 participants would have been needed to have adequate power to detect an intervention effect.[18] Among the three unique RCT sample pools, the largest enrollment at 6 months was even less than this (N=120), with nearly 50% loss to follow-up in treatment and control arms.[31]
Finally, two cost-effectiveness analyses[33],[34] were performed on previously studied samples,[4],[16] using reported reinjury reduction rates. Markov mathematical modeling was used in both studies, which shared a coinvestigator. Modeling results concluded in both studies that there is a cost savings with HVIPs.
Brief summaries of the eight papers that provided original data about reinjury are provided below, organized by study type and in reverse chronological order. The cost-effectiveness analyses were models and will not be summarized here. Table 1 provides an overview of salient findings.

Table 1. Summary of evidence for preventative efficacy of HVIPs in adult patients (age 18+) treated for intentional violent injury.
Randomized clinical trials
Aboutanos et al6 included admitted patients aged 10–24 years (average age=19) presenting to the emergency department after intentional violent injury (assault, stabbings, and firearm) in Richmond, Virginia. Eighty-seven percent of the participants were African-American while White and other made up the remaining 13%. Seventy-four of 75 participants presented with either gunshot or stab wounds. In lieu of a control group (prohibited on ethical grounds by an Institutional Review Board), this study compared two randomly assigned intervention groups (Group I received psychoeducational intervention; Group II psychoeducational intervention plus wraparound services such as vocational, educational, house, and mental health resources) to historical trauma registry data. The study had 20% attrition by week-6 follow-up, with nearly half of remaining patients subsequently being lost from the study by the 6-month follow-up. This study showed no intervention effect on employment, education, or intentional violent injury recidivism and/or death, although 17% of the intervention group versus 30% of the historical group were incarcerated postdischarge (no statistical significance reported). At 6 weeks, there was a 35% reduction (OR=2.5; CI 1.2 to 5.4; p<0.023) in alcohol consumption, but by 6 months the remaining sample size (N=16) was low. Likewise, there was a statistically significant reduction in drug use at 6 weeks, but the sample size at 6 months was again extremely small.
Cooper et al[14] restricted study participation to patients 18 years and older admitted to the hospital for violent injuries and on probation/parole. Additional psychosocial services such as family or group therapy and substance abuse treatment were provided for the intervention group (n=56); the control group (n=44) received standard care. Age and gender were similar between the intervention and control groups. The study reported a 5% intentional violent injury and/or death recidivism rate and 82% employment rate for the intervention group, versus rates of 36% and 20%, respectively, in the control group. Statistical analysis was provided for neither outcome. The study also reported a reduction in the intervention cohort's arrest rate (64%) compared to the nonintervention group (80%) (OR=1.2; CI 1.0 to 1.9; p=0.095). The percentage of intervention group patients (18%) arrested for violent crime was lower than that for the nonintervention group (49%).
Zun et al[30] included patients aged 10–24 years (average age=18.6) presenting to the emergency department after violent interpersonal life-threatening or limb-threatening injury in Chicago, Illinois, USA. Cases involving child abuse, sexual assault and intimate partner violence were excluded. Participants assigned to the intervention group (n=96 at 6 months; n=62 at 12 months) were provided assessment and 6-month case management in contrast to control group participants (n=92 at 6 months; n=59 at 12 months), who received a resource list. The initial study group was 65% African-American and 31% Hispanic; 41% were between 20 and 24 years-old. At 6 months: violence victimization rates were 6.5% for the intervention group and 7.4% for the control (χ2=3.87; p=0.05); arrest rates were 7.5% vs 7.4% (χ2=0.002; p=ns); incarceration rates were 12.9% vs 13.7% (χ2=0.03; p=ns). The authors reported a lower intervention group reinjury rate, but the rate was based on self-reports. Limitations included small sample size and large loss-to-follow-up (nearly 50%), use of self-reports, and high case manager turnover.
Zun et al[31] used the same study population as described above, but the measured outcome at 6 and 12 months was attitude toward violence. There was no significant difference between the intervention or control groups. Limitations included small sample size and high patient attrition.
Observational studies
Smith et al[24] screened violently injured patients aged 10–30 years for low versus high risk for reinjury. “Trained case managers performed risk assessments to distinguish high-risk vs low-risk individuals, oftentimes by identifying physical signs (ie, elusive tattoos), social cues (ie, multiple gang member visitors), or emotional volatility (ie, anger and/or discussion of retaliation).” Participants were then provided either a moderate (3–6 hours per week) or high (>6 hours per week) dose of case management exposure in first three months of the intervention (no specification on whether within first 3 months indicates since time of injury, postdischarge, or other). As stated above, in comparison to the institution's historical rate, a 16–4%[14] reduction rate in intentional violent injury recidivism was reported, but only active participants were analyzed for this calculation.
Gomez et al[32] included patients admitted for violent injury and screened by support specialists in Indianapolis, Indiana, USA. Support specialists worked with participants to identify goals and develop tailored service plans (n=64 patients enrolled; n=34 in program for at least 1 year) and then referred community services. The violent reinjury rate was reduced from 8.7% to 2.9% among all participants. No data on those who declined to participate were available. Owing to only having access to the abstract, the authors of this paper were unable to determine which violent injuries were included and/or excluded and were not privy to any statistical significance reporting.
Shibru et al[18] included patients aged 10–20 years (average age=17) hospitalized for intentional violent trauma in Oakland, California, USA. This group provided a peer intervention program for the enrolled group (n=75; n=300 needed for statistical significance). The comparison group (n=79; n=300 needed for statistical significance) consisted of anonymous trauma registry database patients matched by age, gender, race/ethnicity, type of injury, and year of admission to enrollees. Intervention patients and their families were assigned an intervention specialist who assisted with activities including transportation to and from the hospital, court hearings, mental health counseling, work, and school. Fifty-nine percent of the enrolled group and 60% of the control group were African-American and 35% and 32% were Latino, respectively. Gunshot and stab wounds made up 66% of the enrolled group injuries versus 59% for the control group. Control group bias existed due to inclusion of ‘missed’ patients (eg, patients treated and released outside business hours, not arriving for first scheduled appointment, or missed during admission by study coordinator). Compared with the control group, the enrolled cohort showed no reduction in intentional violent injury and/or death recidivism and some reduction in violent criminal behavior (7% reduction; p=0.15) and criminal justice involvement (relative risk=0.67; 95% CI 0.45 to 0.99; p=0.04).
Becker et al[12] evaluated 112 violently injured and hospitalized participants, the majority of whom (61.6%) were aged 18 years or above. Sixty percent of participants were African-American and 26% were Latino. The applied intervention was a peer-based program. ‘Crisis intervention specialists’ with cultural backgrounds similar to the patients and who had experienced violence themselves met with enrollees and their families as soon as possible. They later provided assistance with engaging community resources, home visits and housing, in addition to other services. In contrast to the intervention group (n=43) where 67.4% of participants were injured in firearm violence, members of the retrospective control group (n=69) were one-third less likely to have been victims of firearm violence and more likely to have been victims of blunt, as opposed to penetrating, trauma. The intervention had no reported effect on intentional violent injury and/or death recidivism, but the control group was 70% less likely (OR=0.257; 95% CI 0.54 to 1.223; p=0.06). A major limitation is that data collection was limited to a 6-month postinjury period. Statistical analysis was limited by low sample size.
Discussion
Our EBR of the current literature demonstrates that when it comes to understanding if HVIPs abate cycles of street violence and reinjury in adult populations throughout the USA, there remains little scientific evidence on which to base interventional recommendations. By applying validated GRADE methods, the quality of evidence proved too weak to warrant a separate assessment of interventional efficacy for each outcome.
While hospitals have effectively used emergency departments to intervene in substance abuse, child abuse, domestic abuse, and self-harm,[8] the limited data available preclude any empirical evaluation of HVIP impact on adult populations injured by intentional violence. Our state of the science has not changed since 2007 when, for example, the National Academy of Sciences concluded that despite the USA exhibiting the highest rate of gun violence in the democratized world, “inadequate data and inadequate access to existing data are among the most critical barriers to understanding gun violence”.[35]
Pragmatically, data collection on HVIPs is bound by at least two constraints. First, the low socioeconomic status of under-resourced ethnicities at high risk for intentional violent injury recidivism makes them difficult to not only recruit but also to retain in research.[7],[11],[22],[27],[28] In addition to limited resources for gas and parking costs, patients injured by intentional violent injury report fear of leaving the house and fear of using public transit as impediments to hospital service usage and follow-up, even when extremely pleased with their in-patient care.[5] Others have noted logistical constraints such as frequent changes in addresses and phone numbers in these patients.[5],[28] In 2010, Schwartz et al[28] noted that “little research is available to describe the specific barriers and facilitators to research participation” and a need to “identify challenges and facilitators to conducting research with Black male victims of community violence, particularly with regard to recruitment and maintenance of a study sample.”
A second major constraint is the cost of adequate research personnel to engage and retain prospective study participants.[8] For example, Aboutanos et al6 were unable to enroll 265 of 376 potentially eligible patients due to a lack of resources, such as having only a part-time coordinator during the first year of the study. Likewise, Zun et al[30] reported high case manager turnover and, in fact, stated that their “study was limited by the availability, effectiveness, and reliability of services at the time of the study.” Similarly, Shibru et al[18] were unable to reach patients who were treated and released outside of business hours or when the injury prevention coordinator missed them at admission, which presumably played a role in their attaining in 5½ only 25% of the sample size necessary “to identify the clinically relevant outcomes of death and traumatic injury from intentional violence,” as indicated by a power analysis. Owing to the lack of federal or foundation funding for large-scale research, these needed resources are difficult to obtain. Compared with other medical-related or trauma-related injuries, the paucity of funding for gun violence research sharply restricts large-scale efforts and limits an evidence-based national discussion. Finally, two of our outcomes of interest, arrest or incarceration and school attainment, were not represented in the literature.
The Affordable Care Act promises to facilitate coverage for many preventive services[29],[36] but fails to address intentional violent injury. While recent developments in the US healthcare system may increase primary care service usage and thus expand targetable occasions, these will remain ‘opt-in’ services, meaning the individual retains the burden of purposely seeking care, versus ‘opt-out’ opportunities where the injured patient is positioned to refuse, rather than seek, further care such as counseling. HVIPs represent an ‘opt-out’ possibility for prevention.
Finally, we are very encouraged by ongoing efforts, with respect to research and advocacy, from groups such as the National Network of Hospital-Based Violence Intervention Projects, and Cure Violence. Since this type of work is nearly impossible to perform in the context of a RCT, future researchers will need to find innovative ways to study and judge the quality of these programs. We look forward to reexamining this topic in the near future, as many of these programs have ongoing evaluation arms that should hopefully be published in peer-reviewed journals in the next several years.
Recommendations
Are HVIPs attending to adult patients (age 18+) treated for intentional violent injury more effective than usual standard care in improving the following outcomes: intentional violent injury reinjury and/or death; arrest and/or incarceration; substance abuse and/or mental issues; quality of life; job and/or school attainment? (PICO 1).
Recommendation: We make no recommendation with respect to adult-focused HVIP interventions to reduce violent reinjury and other outcomes, due to quality of evidence concerns such as self-selection bias and small sample sizes. However, we acknowledge that some single center programs have been effective at improving outcomes among motivated patients. Ensuring that studies are sufficiently and adequately staffed, continuing efforts to increase research funding for gun violence-related issues, and developing strategies to not only reach but also retain adult populations injured in intentional violence may lessen the constraints prohibiting robust empirical support for HVIPs.
Conclusions
Given the powerful impact on health by social determinants[37] such as neighborhood household income,[38] and insurance status,[39],[40] it behooves the successful research, development, and implementation of any intentional violence intervention program to be sufficiently informed of patient preadmission and postdischarge psychosocial contexts.[11] While multiple hospital-based programs have been implemented, the weak quality of aggregate data prohibits either the validation or invalidation of HVIP efficacy on a population level. Therefore, ongoing, rigorous evaluation methods will be necessary to substantiate the hypothesis that HVIPs are, in fact, efficacious and cost-effective. Evidence of efficacy will legitimate further funding for such program development and ensure that healthcare services sufficiently meet patient needs.
Acknowledgments
The authors acknowledge the Eastern Association for the Surgery of Trauma Guidelines Section members for their editorial support.
Footnotes
- Contributors SA, DP, LH, and MC were responsible for the conceptualization, evidence grading, and manuscript preparation. PV, MR, and ABC were responsible for evidence grading and editorial support. AS and BR were responsible for key editorial support.
- Competing interests None declared.
- Provenance and peer review Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
References
- Cohn D, Taylor P, Lopez MH, Gallagher CA, Parker K, Maass KT. Gun homicide rate down 49% since 1993 peak; public unaware. Washington (DC): Pew Research Center, 2013.http://www.pewsocialtrends.org/2013/05/07/gun-homicide-rate-down-49-since-1993-peak-public-unaware/(accessed Dec 2015).
- Papachristos AV, Wildeman C, Roberto E. Tragic, but not random: the social contagion of nonfatal gunshot injuries. Soc Sci Med 2015;125: 139–50. doi:10.1016/j.socscimed.2014.01.056 CrossRef Medline Google Scholar
- Corbin TJ, Purtle J, Rich LJ, Rich JA, Adams EJ, Yee G, Bloom SL. The prevalence of trauma and childhood adversity in an urban, hospital-based violence intervention program. J Health Care Poor Underserved2013;24:1021–30. doi:10.1353/hpu.2013.0120 Google Scholar
- Purtle J, Dicker R, Cooper C, Corbin T, Greene MB, Marks A, Creaser D, Topp D, Moreland D. Hospital-based violence intervention programs save lives and money. J Trauma Acute Care Surg 2013;75:331–3. doi:10.1097/TA.0b013e318294f518 Google Scholar
- Liebschutz J, Schwartz S, Hoyte J, Conoscenti L, Christian AB Sr., Muhammad L, Harper D, James T. A chasm between injury and care: experiences of black male victims of violence. J Trauma 2010;69:1372–8. http://dx.doi.org/10.1097/TA.0b013e3181e74fcf Medline Google Scholar
- Aboutanos MB, Jordan A, Cohen R, Foster RL, Goodman K, Halfond RW, Poindexter R, Charles R, SmithSC, Wolfe LG, et al. Brief violence interventions with community case management services are effective for high-risk trauma patients. J Trauma 2011;71:228–36; discussion 236–7. doi:10.1097/TA.0b013e31821e0c86 Medline Google Scholar
- Rich JA, Grey CM. Pathways to recurrent trauma among young Black men: traumatic stress, substance use, and the “code of the street”. Am J Public Health 2005;95:816–24. doi:10.2105/AJPH.2004.044560 CrossRef Medline Web of Science Google Scholar
- Cunningham R, Knox L, Fein J, Harrison S, Frisch K, Walton M, Dicker R, Calhoun D, Becker M, Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med 2009;53:490–500. doi:10.1016/j.annemergmed.2008.11.014 CrossRef Medline Google Scholar
- Hedges BE, Dimsdale JE, Hoyt DB, Berry C, Leitz K. Characteristics of repeat trauma patients, San Diego County. Am J Public Health 1995;85:1008–10. doi:10.2105/AJPH.85.7.1008 CrossRef Medline Web of Science Google Scholar
- Jones-Webb R, Wall M. Neighborhood racial/ethnic concentration, social disadvantage, and homicide risk: an ecological analysis of 10 U.S. cities. J Urban Health 2008;85:662–76. doi:10.1007/s11524-008-9302-y CrossRef Medline Web of Science Google Scholar
- Kelly VG, Merrill GS, Shumway M, Alvidrez J, Boccellari A. Outreach, engagement, and practical assistance: essential aspects of PTSD care for urban victims of violent crime. Trauma Violence Abuse 2010;11:144–56. doi:10.1177/1524838010374481 Abstract/FREE Full Text Google Scholar
- Becker MG, Hall JS, Ursic CM, Jain S, Calhoun D. Caught in the Crossfire: the effects of a peer-based intervention program for violently injured youth. J Adolesc Health 2004;34:177–83.doi:10.1016/j.jadohealth.2003.04.001 CrossRef Medline Web of Science Google Scholar
- Cooper C, Eslinger D, Nash D, Al-Zawahri J, Stolley P. Repeat victims of violence: report of a large concurrent case-control study. Arch Surg 2000;135:837–43. doi:10.1001/archsurg.135.7.837 CrossRef Medline Web of Science Google Scholar
- Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma2006;61:534–7; discussion 537–40. doi:10.1097/01.ta.0000236576.81860.8c CrossRef Medline Web of Science Google Scholar
- Kennedy F, Brown JR, Brown KA, Fleming AW. Geographic and temporal patterns of recurrent intentional injury in south-central Los Angeles. J Natl Med Assoc 1996;88:570–2. Medline Google Scholar
- Belcher JR, Deforge BR, Jani JS. Inner-city victims of violence and trauma care: the importance of trauma-center discharge and aftercare planning and violence prevention programs. J Health Soc Policy2005;21:17–34. doi:10.1300/J045v21n02_02 Medline Google Scholar
- Morrissey TB, Byrd CR, Deitch EA. The incidence of recurrent penetrating trauma in an urban trauma center. J Trauma 1991;31:1536–8. doi:10.1097/00005373-199111000-00013 CrossRef Medline Web of Science Google Scholar
- Shibru D, Zahnd E, Becker M, Bekaert N, Calhoun D, Victorino GP. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg 2007;205:684–9.doi:10.1016/j.jamcollsurg.2007.05.029 CrossRef Medline Google Scholar
- Corbin TJ, Rich JA, Bloom SL, Delgado D, Rich LJ, Wilson AS. Developing a trauma-informed, emergency department-based intervention for victims of urban violence. J Trauma Dissociation 2011;12:510–25. doi:10.1080/15299732.2011.593260 CrossRef Medline Web of Science Google Scholar
- Ramchand R, Marshall GN, Schell TL, Jaycox LH. Posttraumatic distress and physical functioning: a longitudinal study of injured survivors of community violence. J Consult Clin Psychol 2008;76:668–76. doi:10.1037/0022-006X.76.4.668 CrossRef Medline Web of Science Google Scholar
- Lee J, Quraishi SA, Bhatnagar S, Zafonte RD, Masiakos PT. The economic cost of firearm-related injuries in the United States from 2006 to 2010. Surgery 2014;155:894–8. doi:10.1016/j.surg.2014.02.011 CrossRef Medline Google Scholar
- Boccellari A, Alvidrez J, Shumway M, Kelly V, Merrill G, Gelb M, Smart S, Okin RL. Characteristics and psychosocial needs of victims of violent crime identified at a public-sector hospital: data from a large clinical trial. Gen Hosp Psychiatry 2007;29:236–43. doi:10.1016/j.genhosppsych.2007.01.008 CrossRef Medline Web of Science Google Scholar
- Livingston D, Lavery R, Lopreiato M, Lavery D, Passannante M. Unrelenting violence: an analysis of 6322 gunshot wound patients at a Level I trauma center. J Trauma 2014;76:2–11. doi:10.1097/TA.0b013e3182ab19e7 Google Scholar
- Smith R, Dobbins S, Evans A, Balhotra K, Dicker RA. Hospital-based violence intervention: risk reduction resources that are essential for success. J Trauma Acute Care Surg 2013;74:976–80; discussion 980–982. doi:10.1097/TA.0b013e31828586c9 Google Scholar
- Jaeschke R, Guyatt GH, Dellinger P, Schuenemann H, Levy MM, Kunz R, Norris S, Bion J, GRADE Working Group. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ2008;337:a744. doi:10.1136/bmj.a744 FREE Full Text Google Scholar
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ, GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ2008;336:924–6. doi:10.1136/bmj.39489.470347.AD FREE Full Text Google Scholar
- Wang TF, Shi L, Nie X, Zhu J. Race/ethnicity, insurance, income and access to care: the influence of health status. Int J Equity Health 2013;12:29. doi:10.1186/1475-9276-12-29 CrossRef Medline Google Scholar
- Schwartz S, Hoyte J, James T, Conoscenti L, Johnson RM, Liebschutz J. Challenges to engaging black male victims of community violence in healthcare research: lessons learned from two studies. Psychol Trauma2010;2:54–62. doi:10.1037/a0019020 Medline Google Scholar
- US Department of Health and Human Services. The Affordable Care Act and African Americans. Nov 5, 2014. http://www.hhs.gov/healthcare/facts/factsheets/2012/04/aca-and-african-americans04122012a.html(accessed Dec 2015).
- Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. Am J Emerg Med 2006;24:8–13. doi:10.1016/j.ajem.2005.05.009 CrossRef Medline Web of Science Google Scholar
- Zun LS, Downey L, Rosen J. An emergency department-based program to change attitudes of youth toward violence. J Emerg Med 2004;26:247–51. doi:10.1016/j.jemermed.2003.06.008 CrossRef Medline Web of Science Google Scholar
- Gomez G, Simons C, St John W, Creasser D, Hackworth J, Gupta P, Joy T, Kemp H. Project Prescription for Hope (RxH): trauma surgeons and community aligned to reduce injury recidivism caused by violence. Am Surg 2012;78:1000–4. Medline Google Scholar
- Juillard C, Smith R, Anaya N, Garcia A, Kahn J, Dicker R. Saving lives and saving money: hospital-based violence intervention is cost-effective. J Trauma 2015;78:252–8. doi:10.1097/TA.0000000000000527 Google Scholar
- Chong VE, Smith R, Garcia A, Lee W, Ashley L, Marks A, Liu T, Victorino G. Hospital-centered violence intervention programs: a cost-effectiveness analysis. Am J Surg 2015;209:597–603. doi:10.1016/j.amjsurg.2014.11.003 Google Scholar
- Weiner J, Wiebe DJ, Richmond TS, Beam K, Berman AL, Branas CC, Cheney RA, Coyne-Beasley T, FirmanJ, Fishbein M, et al. Reducing firearm violence: a research agenda. Inj Prev 2007;13:80–4.doi:10.1136/ip.2006.013359 Abstract/FREE Full Text Google Scholar
- US Department of Health and Human Services. Preventive care benefits. 12 March 2015. https://www.healthcare.gov/preventive-care-benefits/(accessed Dec 2015).
- Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes.Public Health Rep 2014;129(Suppl 2):19–31. Abstract/FREE Full Text Google Scholar
- Leukhardt WH, Golob JF, Mccoy AM, Fadlalla AM, Malangoni MA, Claridge JA. Follow-up disparities after trauma: a real problem for outcomes research. Am J Surg 2010;199:348–52; discussion 353. doi:10.1016/j.amjsurg.2009.09.021 CrossRef Medline Google Scholar
- Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE III. Race and insurance status as risk factors for trauma mortality. Arch Surg 2008;143:945–9. doi:10.1001/archsurg.143.10.945 CrossRef Medline Web of Science Google Scholar
- Hansen L, Shaheen A, Crandall M. Outpatient follow-up after traumatic injury: challenges and opportunities.J Emerg Trauma Shock 2014;7:256–60. doi:10.4103/0974-2700.142612 Google Scholar