Pediatric Blunt Renal Trauma
Published 2019
Citation: J Trauma. 86(5):916-925, May 2019
Pediatric blunt renal trauma practice management guidelines
Collaboration between the Eastern Association for the Surgery of Trauma and the Pediatric Trauma Society
Authors
Hagedorn, Judith C., MD; Fox, Nicole, MD; Ellison, Jonathan S., MD; Russell, Robert, MD; Witt, Cordelie E., MD; Zeller, Kristen, MD; Ferrada, Paula, MD; Draus, John M. Jr, MD
Author Information
From the Department of Urology (J.C.H.), University of Washington, Seattle, Washington; Division of PediatricSurgery, Department of Surgery (N.F.), Cooper University, Camden, New Jersey; Children's Hospital of Wisconsin and Medical College of Wisconsin (J.S.E.), Milwaukee, Wisconsin; Department of Surgery (R.R.), Children's Hospital of Alabama, University of Alabama at Birmingham, Birmingham, Alabama; Department of Surgery (C.E.W.), University of Washington, Seattle, Washington; Department of Surgery (K.Z.), Section of PediatricSurgery, Wake Forest School of Medicine, Wake Forest, North Carolina; Department of Surgery (P.F.), Virginia Commonwealth University, Richmond, Virginia; and Division of Pediatric Surgery, Department of Surgery (J.M.D.), University of Kentucky, Lexington, Kentucky.
Submitted: September 10, 2018, Revised: November 20, 2018, Accepted: December 24, 2018, Published online: Febuary 7, 2019.
Address for reprints: Judith C. Hagedorn, MD, Department of Urology, Harborview Injury Prevention and Research Center (HIPRC), University of Washington Harborview Medical Center, Box 359960, 325 9th Avenue, Seattle, WA 98104; email: judithch@uw.edu.
These guidelines were presented at the 31st EAST Annual Scientific Assembly, January 11-15th, 2018 in Lake Buena Vista, FL.
BACKGROUND Injury to the kidney from either blunt or penetrating trauma is the most common urinary tract injury. Children are at higher risk of renal injury from blunt trauma than adults, but no pediatric renal traumaguidelines have been established. The authors reviewed the literature to guide clinicians in the appropriate methods of management of pediatric renal trauma.
METHODS Grading of Recommendations Assessment, Development and Evaluation methodology was used to aid with the development of these evidence-based practice management guidelines. A systematic review of the literature including citations published between 1990 and 2016 was performed. Fifty-one articles were used to inform the statements presented in the guidelines. When possible, a meta-analysis with forest plots was created, and the evidence was graded.
RESULTS When comparing nonoperative management versus operative management in hemodynamically stable pediatric patient with blunt renal trauma, evidence suggests that there is a reduced rate of renal loss and blood transfusion in patients managed nonoperatively. We found that in pediatric patients with high-grade American Association for the Surgery of Trauma grade III-V (AAST III-V) renal injuries and ongoing bleeding or delayed bleeding, angioembolization has a decreased rate of renal loss compared with surgical intervention. We found the rate of posttraumatic renal hypertension to be 4.2%.
CONCLUSION Based on the completed meta-analyses and Grading of Recommendations Assessment, Development and Evaluation profile, we are making the following recommendations: (1) In pediatric patients with blunt renal trauma of all grades, we strongly recommend nonoperative management versus operative management in hemodynamically stable patients. (2) In hemodynamically stable pediatric patients with high-grade (AAST grade III-V) renal injuries, we strongly recommend angioembolization versus surgical intervention for ongoing or delayed bleeding. (3) In pediatric patients with renal trauma, we strongly recommend routine blood pressure checks to diagnose hypertension. This review of the literature reveals limitations and the need for additional research on diagnosis and management of pediatric renal trauma.
LEVEL OF EVIDENCE Guidelines study, level III.
Accidental trauma is the leading cause of death among children and adolescents.[1] Injury to the kidney from blunt trauma is the most common urinary tract injury. In children, blunt trauma is responsible for 90% of renal injuries, and the kidney is injured in approximately 10% of all pediatric blunt abdominal trauma.[2] Children are at higher risk of renal injury from blunt trauma than adults due to several anatomic factors including decreased perirenal fat, weaker abdominal musculature, and a less ossified thoracic cage—all of which offer less protection to the kidney.[3]
Several surgical/urologic societies, including the American Urologic Association and the European Association of Urology, and the Eastern Association for the Surgery of Trauma (EAST), have guidelines for adult renal trauma; however, there are currently no renal trauma guidelines focused on pediatric patients.[4–7] As a result, the Pediatric Trauma Society and EAST Guidelines committees collaborated to develop guidelines for this topic using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework recently adopted by EAST.[8]
The GRADE methodology is being used worldwide to aid with the development of evidence-based practice managementguidelines. The GRADE framework serves as a systematic and transparent guide that leads to a summary of the existing evidence and eventually allows this evidence to be translated into recommendations. For each study, evidence is rated concerning a specific clinical outcome that deems to be important to clinical care. The strength of the final recommendations is based on evidence quality, taking into consideration the balance between clinical outcomes and patient preferences and values.
Areas of focus in the pediatric blunt renal trauma guidelines include management of pediatric renal trauma (operative vs. nonoperative), type of surgical intervention (angioembolization vs. open surgery), and follow-up (blood pressure checks vs. no blood pressure checks).
Objectives
The objectives of these guidelines are to evaluate the management of pediatric blunt renal trauma (operative vs. nonoperative), type of surgical intervention (angioembolization vs. open surgery), and follow-up (blood pressure checks vs. no blood pressure checks). The Population (P), Intervention (I), Comparator (C), and Outcome (O) questions are defined below:
- PICO Question 1: In hemodynamically stable pediatric patients with blunt renal trauma of all grades (P), should operative management (I) versus nonoperative management (C) be performed to decrease the incidence of renal loss, blood transfusion, urinoma formation, additional procedures, and additional imaging (O)?
- PICO Question 2: In hemodynamically stable pediatric patients with high-grade American Association for the Surgery of Trauma grade III-V (AAST III-V) renal injuries from blunt trauma and ongoing or delayed bleeding (P), should angioembolization (I) versus surgical intervention (C) be performed to decrease incidence of renal loss, blood transfusion, and complications(O)?
- PICO Question 3: In pediatric patients with blunt renal trauma (P), should blood pressure checks (I) versus no blood pressure checks (C) be performed on follow up to diagnose hypertension (O)?
Identification of References
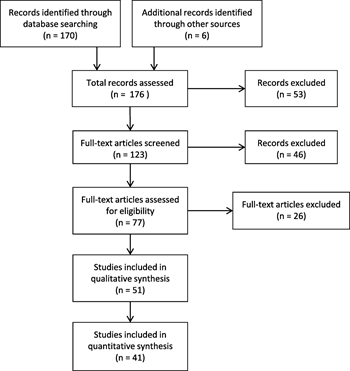
Figure 1. Prisma diagram for systematic review.
A search of the world's peer-reviewed literature was conducted with the assistance of a professional medical research librarian using PubMed (www.pubmed.gov), Scopus (www.elsevier.com/solutions/scopus), and Web of Science (www.webofknowledge.com) with citations published between 1990 and 2016. In addition to the electronic search, we reviewed the bibliographies of recent review articles and published articles and included pertinent citations. Articles were limited to those in English language and involving human subjects. The search terms used included: renal, kidney, trauma, injury, pediatric, penetrating, stab, firearm, gunshot, blunt, and human. We excluded letters to the editor, case reports, book chapters and review articles. A total of 123 articles were identified, and these articles were reviewed by two committee members (J.C.H., J.M.D.). The final reference list of 77 citations was then distributed to the remainder of the guidelines group to review. Of these, 51 articles were felt to be appropriate to include in these guidelines (Fig. 1).
Outcome Measure Types
Following GRADE methodology, we chose the outcomes by having all committee members rate the proposed outcomes in importance from 1 to 9 with scores 7 to 9 representing critical outcomes. For PICO question 1, the following outcomes were considered by the committee members: renal loss (partial or total nephrectomy), blood transfusion, urinoma formation, additional procedures, additional imaging, length of stay. Of these outcomes, the committee deemed the following to be “critical” outcomes for PICO question 1: renal loss, blood transfusion, and additional imaging. Urinoma formation and additional procedures were categorized as “important” outcomes and due to the lack of data length of stay was not included as an outcome. For PICO 2, the following outcomes were rated: renal loss, blood transfusion, infection, length of stay, and urine leak. The committee determined the following outcomes to be critical for PICO 2: renal loss, and blood transfusion. Complications such as infection and urine leak were rated as “important.” Due to the lack of data length of stay was not included as an outcome. The diagnosis of hypertension was the only outcome rated for PICO 3 and was deemed to be “critical.”
Data Extraction and Methodology
After the identification of 51 articles pertinent to our pediatric blunt renal trauma guidelines, each article was assigned to two committee members for extraction of data for each PICO question. All of the studies were retrospective reviews, and none of the articles were randomized controlled trials. All of the studies included pediatric patients.
PICO 1
Forty-six articles included data relevant to PICO 1.[9–54] Intrinsic limitations of the data existed because of nonstandardized study design, incomplete reporting of complications, and possible misclassification of renal injury grade. Additionally, some studies only focused on AAST grade IV-V injuries. A total of 46 studies included information on renal loss, eight of these studies did not have a comparison group or reported zero events in each group and were therefore excluded from the meta-analysis and are recorded as “not estimable” in the forest plot. Thirteen studies reported on blood transfusions, and 33 studies had data on additional procedures/imaging. Concerning the meta-analysis, thirty-eight studies had the necessary information to make Forest plots for the outcome of renal loss, and eight studies included the necessary information to make Forest plots for the outcome of blood transfusion, comparing operative versus nonoperative management.
PICO 2
A total of six articles included data relevant to PICO 2.[14][30][35][55–57] The same limitations seen with PICO 1 existed. Three articles contained sufficient information to construct Forest plots on the outcome of renal loss, two studies for the outcome of blood transfusion, and two studies on infection/urine leak, comparing angioembolization versus surgical intervention. All six studies reported on renal loss, three studies reported on blood transfusions and five studies had data on complications, defined as infection and urine leak.
PICO 3
Sixteen articles were available to address PICO 3.[17][19][21][26][29–31][33][34][40][42][43][46][53][54][58] The major limitation of the data for PICO 3 is the short follow-up and/or loss to follow-up in many of the studies. No study reported on the incidence of hypertension in the pediatric patients who did not get any blood pressures on follow-up. Therefore, there was no comparison group to generate Forest plots and was not included in the meta-analysis.
Results for PICO Question 1
In pediatric patients with blunt renal trauma of all grades (P), should operative management (I) versus nonoperative management (C) be performed to decrease the incidence of renal loss, blood transfusion, urinoma formation, additional procedures, and additional imaging (O) in hemodynamically stable patients?
Qualitative Synthesis
The management of renal trauma has shifted in favor of nonoperative over the past 30 years.[59] Nonoperative management gained popularity owing to considerably higher renal salvage rates than operative management.[60] The trend toward nonoperative management has been reported for blunt renal injuries in children as well.[61][62] Although randomized trials do not exist and would likely not be feasible in the trauma setting, nonoperative management for low grade (AAST I-III) renal injuries is well accepted, whereas less evidence is available for the management of high-grade (AAST IV-V) renal injuries.[63] Nevertheless, high-grade injuries are being managed nonoperatively with increasing frequency.[9][15][25][30] The only absolute indication for operative management is failure to respond to resuscitation which manifests in persistent hemodynamic instability.[63]
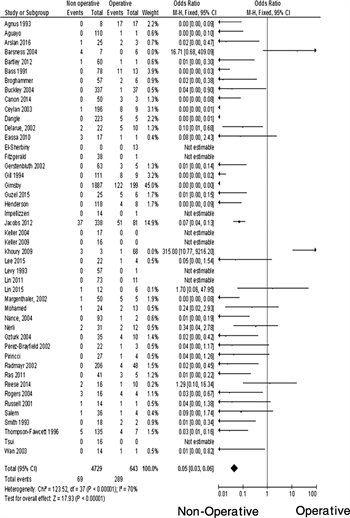
Figure 2. Forest plot for PICO 1, comparing the outcome of renal loss for nonoperative and operative management of hemodynamically stable pediatric patients with blunt renal trauma of all grades.
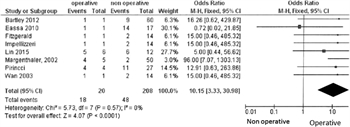
Figure 3. Forest plot for PICO 1, comparing the outcome of blood transfusion for operative and nonoperative management of hemodynamically stable pediatric patients with blunt renal trauma of all grades.
Forty-six studies published after 1990 were relevant to this PICO question. Combining all the studies, a total of 5,561 children sustained blunt renal trauma of which 579 (10%) underwent operative intervention, and 4,982 (89.6%) were managed nonoperatively. Thirty-eight of the studies included comparison data on renal loss that was adequate to create a Forest plot (Fig. 2). Studies that had no renal loss in neither the operative nor the nonoperative group were not included in the meta-analysis (“not estimable” in Fig. 2). In the operative group, almost half (44.9%) of the children had renal loss compared with 1.5% in the nonoperative group. Eight of the studies included comparison data on blood transfusion that was adequate to create a Forest plot (Fig. 3). In the operative group, 90% required blood transfusion compared with 23.1% in the nonoperative group. Twenty-eight studies included information on urinoma formation, and 2.4% developed a urinoma in the operative group versus 1.2% in the nonoperative group. Thirty-two studies had information about additional procedures that were needed for 2.8% of patients in the operative group and 5.7% in the nonoperative group. Fifteen studies reported on additional imaging which was performed in 0.3% of the operative group and 3.5% in the nonoperative group. Only four studies included information on length of hospital stay. Due to the lack of data, we did not include length of hospital stay in our final PICO question.
Quantitative Synthesis (Meta-Analysis)
Thirty-eight studies were included in the meta-analysis for the outcome of renal loss, comparing the nonoperative to the operative group. Nonoperative management was significantly associated with reduced renal loss rates with an odds ratio (OR) of 0.05 (95% confidence interval [CI], 0.03–0.06). Of note, the I[2] statistic was 70%, falling into the “moderate to high” heterogeneity category, indicating that the effect size varies substantively across studies. Nonoperative management had significantly less blood transfusion requirements with an OR of 10.15 (95% CI, 3.33–30.98). The I[2] was 0%, falling into the “low” heterogeneity category, indicating that the studies are comparable.
Due to the small numbers reported, as well as the heterogeneity and variability in the reporting of urinoma formation and additional procedures/imaging among all the studies, a meta-analysis was not appropriate for these outcomes.
Grading the Evidence

Table 1. Evidence Table for PICO Question 1
All of the data related to this PICO question were retrospective and observational in nature. With the use of the GRADE framework for evaluating the outcome of renal loss we rated the evidence as moderate due to the magnitude of effect. For the outcomes of blood transfusion the quality of the data for this PICO question suffered from imprecision (Table 1). Imprecision was assigned for blood transfusion due to the very low numbers of events. The overall quality of evidence was determined to be very low.
Recommendation
Although the overall quality of the data for this PICO question was considered to be very low, the guidelines panel considered the fact that most patients would place very high value on nonoperative management with a much decreased rate of renal loss compared with operative intervention. The panel discussion centered around the benefits from nonoperative management as a national standard of care. There is no literature that describes patient preferences, but one can assume that patients would rather avoid a major surgery and potential renal loss compared with nonoperative management even if this requires minor interventions such as ureteral stent placements or urinoma drainage. We did not find any evidence that nonoperative management leads to longer hospital stay, but the data are scarce. The panel went through a blinded voting process for this PICO question. The responses were tallied and eventually discussed among the entire group. The final vote was unanimous. For the final recommendation, the guidelines panel considered the following: quality of evidence, balance between desirable and undesirable outcomes, patients' values and preferences. Within the GRADE framework, a strong recommendation implies that most individuals would want the recommended course of action and only a small proportion would not.
“In pediatric patients with blunt renal trauma of all grades, we strongly recommend nonoperative management versus operative management in hemodynamically stable patients.”
Results for PICO Question 2
In hemodynamically stable pediatric patients with high-grade (AAST III-V) renal injuries from blunt trauma and ongoing or delayed bleeding (P), should angioembolization (I) versus surgical intervention (C) be performed to decrease incidence of renal loss, blood transfusion, and complications.(O)?
Qualitative Synthesis
Contemporary treatment options for blunt renal trauma include observation, renal angioembolization, open repair or nephrectomy. Angioembolization has the potential advantage of less morbidity, lower rate of complications, faster convalescence and renal loss than open surgery and has become widely used for patients with ongoing bleeding from renal trauma. It must be noted that angioembolization does have its own risks, including radiation exposure, contrast nephropathy, hemorrhage, pain, arterial dissection, and ectopic coil placement.[64–68] Therefore, its use should be reserved for patient with ongoing bleeding from renal trauma, and its overuse in hemodynamically stable patients, especially with low grade injuries, should be discouraged.[67] Radiographic predictors of the need for subsequent intervention have been reported in the literature and include hematoma rim distance greater than 3.5 cm, intravascular contrast extravasation, and medial renal laceration site.[69] These radiographic characteristics have been reported for patients of any age and have not specifically been studied in the pediatric population.
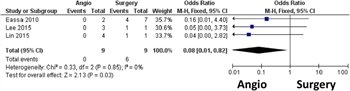
Figure 4. Forest plot for PICO 2, comparing the outcome of renal loss for angioembolization and surgery in hemodynamically stable pediatric patients with high-grade (AAST III-V) renal injuries and ongoing or delayed bleeding.
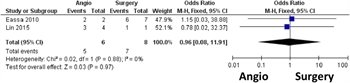
Figure 5. Forest plot for PICO 2, comparing the outcome of blood transfusion for angioembolization and surgery in hemodynamically stable pediatric patients with high-grade (AAST III-V) renal injuries and ongoing or delayed bleeding.
Six studies published after 1990 were relevant to this PICO question. Combining all of the studies, a total of 62 children presented with high-grade (AAST III-V) blunt renal trauma of which 18 (29%) underwent angioembolization and nine (14.5%) underwent open surgical intervention. Three of the studies included comparison data on renal loss that was adequate to create a Forest plot (Fig. 4). In the angioembolization group, no child had renal loss (0%) compared with 66.7% in the operative group. Two of the studies included comparison data on blood transfusion that was adequate to create a Forest plot (Fig. 5). In the angioembolization group, 83.3% required blood transfusion, compared with 87.5% in the operative group. In the angioembolization group, 0% developed a urine leak/infectious complications, compared with 33.3% in the operative group. Three studies evaluated angioembolization only, a total of 55 children were included in these studies and two (3.6%) had renal loss, two (3.6%) needed a blood transfusion and one (1.8%) child had a complication (infection/urine leak).
Quantitative Synthesis (Meta-Analysis)
Three studies were included in the meta-analysis for the outcome of renal loss, comparing the angioembolization to the operative group. Angioembolization was significantly associated with reduced renal loss rates with an OR of 0.08 (95% CI 0.01, 0.82). The I[2] was 0%, falling into the “low” heterogeneity category, indicating that the effect size was comparable across studies. Two studies were included in the meta-analysis for the outcome of blood transfusion, comparing the angioembolization to the operative group. There was no difference between the two groups (OR, 0.96; 95% CI, 0.08–11.91). Due to the small numbers reported, as well as the heterogeneity and variability in the reporting of complications (infection/urine leak) among all the studies, a meta-analysis was not appropriate for these outcomes.
Grading the Evidence

Table 2. Evidence Table for PICO Question 2
All of the data related to this PICO question were retrospective and observational in nature. With the use of the GRADE framework for evaluating the outcomes, including renal loss and blood transfusion, the quality of the data for this PICO question was affected by imprecision due to the very low numbers of events (Table 2). Due to these factors, the overall quality of evidence was determined to be very low.
Recommendation
Even though the overall data quality for this PICO question was considered to be very low, the guidelines panel considered the fact that most patients would place very high value on minimally invasive management with angioembolization which has a much decreased rate of renal loss compared with operative intervention. The panel went through a blinded voting process for this PICO question. The responses were tallied and eventually discussed among the entire group. The final vote was unanimous. For the final recommendation, the guidelines panel considered the following: quality of evidence, balance between desirable and undesirable outcomes, patients' values and preferences and cost and resource use. Within the GRADE framework, a strong recommendation implies that most individuals would want the recommended course of action and only a small proportion would not.
In hemodynamically stable pediatric patients with high-grade (AAST grade III-V) renal injuries from blunt trauma, we strongly recommend angioembolization versus surgical intervention for ongoing or delayed bleeding.”
Results for PICO Question 3
In pediatric patients blunt renal trauma (P), should blood pressure checks (I) versus no blood pressure checks (C) be performed on follow up to diagnose hypertension (O)?
Qualitative Synthesis
Renal ischemia can lead to renin-mediated posttraumatic hypertension. Renal ischemia can be vascular in etiology, for example, arterial thrombosis, arteriovenous malformation/pseudoaneurysm, or due to external compression by hematoma or fibrosis (known as Page kidney). Immediately after the injury, hypertension could be due to pain and may resolve with adequate treatment and observation. In the literature, trauma-induced hypertension after a high-grade injury (AAST grade III-V) has been reported to be around 5%.[46][60] If posttraumatic renal hypertension is diagnosed, imaging should be considered to assess for arteriovenous malformation/pseudoaneurysm and if present treated with angioembolization. If a poorly functioning kidney is associated with posttraumatic hypertension, nephrectomy may be the best option.[34][60] If no such abnormalities can be identified on imaging, posttraumatic renal hypertension should be controlled with angiotensin-converting enzyme inhibitors.
Sixteen studies published after 1990 were relevant to this PICO question. Combining all the studies, a total of 909 children sustained blunt renal trauma, and 496 (52.3%) had blood pressure checks on follow up over months to years. Of note, the follow up for the studies varied widely from 2 weeks postdischarge up to 17 years. The majority (95.8%) of the patients who had received blood pressure checks on follow up were normotensive, whereas 4.2% were diagnosed with hypertension on follow up.
Quantitative Synthesis (Meta-Analysis)
Due to the heterogeneity and variability in the reporting among all the studies a meta-analysis was not appropriate for this PICO question.
Grading the Evidence
All of the data related to this PICO question were retrospective and observational in nature. With the use of the GRADE framework for evaluating the quality of the data, this PICO question was suffering from risk of bias. Risk of bias was assigned due to the incomplete and inadequate short follow-up as well as failure to include a control group. Due to these factors, the overall quality of evidence was determined to be low.
Recommendation
Even though the overall quality of the data for this PICO question was considered to be low the guidelines panel considered the fact that most patients would place high value on treating hypertension to prevent long-term adverse health effects. Additionally, blood pressure checks are noninvasive and low cost. There is no data on the interval, nor length of follow up time that blood pressure monitoring should be conducted. The panel went through a blinded voting process for this PICO question. The responses were tallied and eventually discussed among the entire group. The final vote was unanimous. For the final recommendation, the guidelines panel considered the following: quality of evidence, balance between desirable and undesirable outcomes, patients' values and preferences and cost and resource use. Within the GRADE framework, a strong recommendation implies that most individuals would want the recommended course of action and only a small proportion would not.
“In pediatric patients with blunt renal trauma, we strongly recommend routine blood pressure checks on follow up to diagnose hypertension.”
Using These Guidelines in Clinical Practice
These guidelines represent the thorough and comprehensive review of the literature regarding management and follow up of pediatric patients with renal injuries from blunt trauma. They are meant to guide the decision making process and do not replace clinic judgment. The literature available for review strongly supports nonoperative management for low grade and even high-grade renal injuries in patients with normal hemodynamics and the use of angioembolization in children with high-grade (AAST III-V) renal injuries with ongoing or delayed bleeding. Of note, renal injuries involving the ureteric pelvic junction, which are a AAST grade V injury and identified on the excretory/delayed phase CT images with medial contrast extravasation warrant urgent surgical intervention. In hemodynamically stable patients, a ureteric pelvic junction injury should be assessed with a retrograde ureterorenography and possible stent placement versus open repair.[5] For hemodynamically unstable patients a percutaneous nephrostomy tube can divert the urine until definite repair can be accomplished. An additional indication for surgical intervention for renal trauma in children is of course life-threatening hemorrhage.[37] Concerning blood pressure checks, we know, even with limited data, that posttraumatic hypertension occurs in children with all grades of renal injury.[17][26][30][31][33][46][58] Furthermore, hypertension may be diagnosed during the index hospitalization or during follow-up months to years after the injury.[31][46][58] Children with a history of renal trauma should have their blood pressure measured as part of the follow-up visit with the treating physicians. Thereafter, the child should have their blood pressure checked every year with their primary care provider as recommended by the American Academy of Pediatrics.[70]
Conclusion
In summary, we strongly support three important and evidence-based recommendations regarding pediatric renal traumausing the GRADE methodology. First, we strongly recommend nonoperative management for children with renal trauma. Second, we strongly recommend angioembolization for hemodynamically stable children with high-grade (AAST III-V) renal trauma and ongoing or delayed bleeding. Lastly, we strongly recommend routine blood pressure checks on follow-up to diagnose posttraumatic renal hypertension in children.
Authorship
J.C.H. and J.M.D. conceived the study. All listed authors with exception of P.F. were part of creation of the PICO questions and voted regarding the outcomes of interest for these PICO questions. J.C.H. and J.M.D. performed the entire literature search, read all of the abstracts, and selected the articles for review. All listed authors with exception of P.F. reviewed and summarized selected articles. All listed authors with the exception of P.F. extracted the data from the selected articles. J.C.H. and J.M.D. entered the extracted data into GRADEpro. All listed authors with exception of P.F. evaluated the results for recommendations. P.F. assisted with data analysis. J.C.H. wrote the article. J.M.D. and N.F. participated in the critical review of all versions of this article.
Acknowledgments
We thank the Eastern Association for the Surgery of Trauma (EAST)for the opportunity to write this article and the detail-oriented peer review of this article by the guidelines committee.
We acknowledge the University of Washington Harborview Injury Prevention and Research Center for support of this work.
Disclosure
No conflict of interest, financial or other exists.
The authors did not receive funding for this project.
Reference
- The Leading Cause of Death and Injury. https://www.cdc.gov/injury/wisqars/LeadingCauses.html2015.
- McAninch JW, Carroll PR, Klosterman PW, Dixon CM, Greenblatt MN. Renal reconstruction after injury. J Urol. 1991;145(5):932–937.
- Brown SL, Elder JS, Spirnak JP. Are pediatric patients more susceptible to major renal injury from blunt trauma? A comparative study. J Urol. 1998;160(1):138–140.
- Morey AF, Brandes S, Dugi DD 3rd, Armstrong JH, Breyer BN, Broghammer JA, Erickson BA, Holzbeierlein J, Hudak SJ, Pruitt JH, et al. Urotrauma: AUA guideline. J Urol. 2014;192(2):327–335.
- Lynch TH, Martínez-Piñeiro L, Plas E, Serafetinides E, Türkeri L, Santucci RA, Hohenfellner M. EAU guidelines on urological trauma. Eur Urol. 2005;47(1):1–15.
- Serafetinides E, Kitrey ND, Djakovic N, Kuehhas FE, Lumen N, Sharma DM, Summerton DJ. Review of the current management of upper urinary tract injuries by the EAU trauma guidelines panel. Eur Urol. 2015;67(5):930–936.
- Holevar M EJ, Luchette F, Nagy K, Sheridan R, Spirnak PJ, Yowler C. Practice management guidelines for the management of genitourinary Trauma2004. https://www.east.org/education/practice-management-guidelines/genitourinary-trauma-management-of.
- Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, Stassen N, Dahm P, Committee EAftSoTPMGAH. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S283–S287.
- Okur MH, Arslan S, Aydogdu B, Arslan MS, Goya C, Zeytun H, Basuguy E, Uygun I, Çigdem MK, Önen A, et al. Management of high-grade renal injury in children. Eur J Trauma Emerg Surg. 2017;43:99–104.
- Buckley JC, McAninch JW. Pediatric renal injuries: management guidelines from a 25-year experience. J Urol. 2004;172(2):687–690; discussion 690.
- Bass DH, Semple PL, Cywes S. Investigation and management of blunt renal injuries in children: a review of 11 years' experience. J Pediatr Surg. 1991;26(2):196–200.
- Ceylan H, Gunsar C, Etensel B, Sencan A, Karaca I, Mir E. Blunt renal injuries in Turkish children: a review of 205 cases. Pediatr Surg Int. 2003;19(11):710–714.
- Gill B, Palmer LS, Reda E, Franco I, Kogan SJ, Levitt SB. Optimal renal preservation with timely percutaneous intervention: a changing concept in the management of blunt renal trauma in children in the 1990s. Br J Urol. 1994;74(3):370–374.
- Lee JN, Lim JK, Woo MJ, Kwon SY, Kim BS, Kim HT, Kim TH, Yoo ES, Chung SK. Predictive factors for conservative treatment failure in grade IV pediatric blunt renal trauma. J Pediatr Urol. 2016;12(2):93.e1–93.e7.
- Russell RS, Gomelsky A, McMahon DR, Andrews D, Nasrallah PF. Management of grade IV renal injury in children. J Urol. 2001;166(3):1049–1050.
- Thompson-Fawcett M, Kolbe A. Paediatric renal trauma: caution with conservative management of major injuries. Aust N Z J Surg. 1996;66(7):435–440.
- Eeg KR, Khoury AE, Halachmi S, Braga LH, Farhat WA, Bägli DJ, Pippi Salle JL, Lorenzo AJ. Single center experience with application of the ALARA concept to serial imaging studies after blunt renal trauma in children—is ultrasound enough? J Urol. 2009;181(4):1834–1840; discussion 1840.
- Raz O, Haifler M, Copel L, Lang E, Abu-Kishk I, Eshel G, Klin B, Lindner A, Zisman A. Use of adult criteria for slice imaging may limit unnecessary radiation exposure in children presenting with hematuria and blunt abdominal trauma. Urology. 2011;77(1):187–190.
- Smith EM, Elder JS, Spirnak JP. Major blunt renal trauma in the pediatric population: is a nonoperative approach indicated? J Urol. 1993;149(3):546–548.
- Jacobs MA, Hotaling JM, Mueller BA, Koyle M, Rivara F, Voelzke BB. Conservative management vs early surgery for high grade pediatric renal trauma—do nephrectomy rates differ? J Urol. 2012;187(5):1817–1822.
- Margenthaler JA, Weber TR, Keller MS. Blunt renal trauma in children: experience with conservative management at a pediatric trauma center. J Trauma. 2002;52(5):928–932.
- Grimsby GM, Voelzke B, Hotaling J, Sorensen MD, Koyle M, Jacobs MA. Demographics of pediatric renal trauma. J Urol. 2014;192(5):1498–1502.
- Nance ML, Lutz N, Carr MC, Canning DA, Stafford PW. Blunt renal injuries in children can be managed nonoperatively: outcome in a consecutive series of patients. J Trauma. 2004;57(3):474–478; discussion 478.
- Delarue A, Merrot T, Fahkro A, Alessandrini P, Guys JM. Major renal injuries in children: the real incidence of kidney loss. J Pediatr Surg. 2002;37(10):1446–1450.
- Rogers CG, Knight V, MacUra KJ, Ziegfeld S, Paidas CN, Mathews RI. High-grade renal injuries in children—is conservative management possible? Urology. 2004;64(3):574–579.
- He B, Lin T, Wei G, He D, Li X. Management of blunt renal trauma: an experience in 84 children. Int Urol Nephrol. 2011;43(4):937–942.
- Bartley JM, Santucci RA. Computed tomography findings in patients with pediatric blunt renal trauma in whom expectant (nonoperative) management failed. Urology. 2012;80(6):1338–1343.
- Angus LD, Tachmes L, Kahn S, Gulmi F, Gintautas J, Shaftan GW. Surgical management of pediatric renal trauma: an urban experience. Am Surg. 1993;59(6):388–394.
- Canon S, Recicar J, Head B, Linam L, Swearingen C, Maxson T. The utility of initial and follow-up ultrasound reevaluation for blunt renal trauma in children and adolescents. J Pediatr Urol. 2014;10(5):815–818.
- Eassa W, El-Ghar MA, Jednak R, El-Sherbiny M. Nonoperative management of grade 5 renal injury in children: does it have a place? Eur Urol. 2010;57(1):154–161.
- Güzel M, Arslan S, Turan C, Doganay S. Management of renal injury in children. Ann Ital Chir. 2015;86(3):246–251.
- Perez-Brayfield MR, Gatti JM, Smith EA, Broecker B, Massad C, Scherz H, Kirsch AJ. Blunt traumatic hematuria in children. Is a simplified algorithm justified? J Urol. 2002;167(6):2543–2546; discussion 6–7.
- Radmayr C, Oswald J, Muller E, Holtl L, Bartsch G. Blunt renal trauma in children: 26 years clinical experience in an alpine region. Eur Urol. 2002;42(3):297–300.
- Keller MS, Eric Coln C, Garza JJ, Sartorelli KH, Christine Green M, Weber TR. Functional outcome of nonoperatively managed renal injuries in children. J Trauma. 2004;57(1):108–110; discussion 110.
- Lin WC, Lin CH. The role of interventional radiology for pediatric blunt renal trauma. Ital J Pediatr. 2015;41:76.
- Aguayo P, Fraser JD, Sharp S, Holcomb GW 3rd, Ostlie DJ, St Peter SD. Nonoperative management of blunt renal injury: a need for further study. J Pediatr Surg. 2010;45(6):1311–1314.
- Broghammer JA, Langenburg SE, Smith SJ, Santucci RA. Pediatric blunt renal trauma: its conservative management and patterns of associated injuries. Urology. 2006;67(4):823–827.
- Dangle PP, Fuller TW, Gaines B, Cannon GM, Schneck FX, Stephany HA, Ost MC. Evolving mechanisms of injury and management of pediatric blunt renal trauma—20 years of experience. Urology. 2016;90:159–163.
- Impellizzeri P, Borruto FA, Scalfari G, Arena F, Antonuccio P, Santacaterina E, Montalto AS, Romeo C. Natural history of non-operative treatment for renal injuries in children. Minerva Pediatr. 2012;64(3):319–323.
- Mohamed AZ, Morsi HA, Ziada AM, Habib EM, Aref AM, Kotb EA, Eissa MA, Daw M. Management of major blunt pediatric renal trauma: single-center experience. J Pediatr Urol. 2010;6(3):301–305.
- Pirinççi N, Kaba M, Geçit I, Günes M, Tanik S, Ceylan K. Conservative approach in the treatment of renal trauma in children. Urol Int. 2014;92(2):215–218.
- Salem HK, Morsi HA, Zakaria A. Management of high-grade renal injuries in children after blunt abdominal trauma: experience of 40 cases. J Pediatr Urol. 2007;3(3):223–229.
- Tsui A, Lazarus J, Sebastian van As AB. Non-operative management of renal trauma in very young children: experiences from a dedicated South African Paediatric Trauma Unit. Injury. 2012;43(9):1476–1481.
- Barsness KA, Bensard DD, Partrick D, Hendrickson R, Koyle M, Calkins CM, Karrer F. Renovascular injury: an argument for renal preservation. J Trauma. 2004;57(2):310–315.
- Fitzgerald CL, Tran P, Burnell J, Broghammer JA, Santucci R. Instituting a conservative management protocol for pediatric blunt renal trauma: evaluation of a prospectively maintained patient registry. J Urol. 2011;185(3):1058–1064.
- Henderson CG, Sedberry-Ross S, Pickard R, Bulas DI, Duffy BJ, Tsung D, Eichelberger MR, Belman AB, Rushton HG. Management of high grade renal trauma: 20-year experience at a pediatric level I trauma center. J Urol. 2007;178(1):246–250; discussion 250.
- Levy JB, Baskin LS, Ewalt DH, Zderic SA, Bellah R, Snyder HM 3rd, Templeton J, Duckett JW. Nonoperative management of blunt pediatric major renal trauma. Urology. 1993;42(4):418–424.
- Nerli RB, Metgud T, Patil S, Guntaka A, Umashankar P, Hiremath M, Suresh SN. Severe renal injuries in children following blunt abdominal trauma: selective management and outcome. Pediatr Surg Int. 2011;27(11):1213–1216.
- Reese JN, Fox JA, Cannon GM Jr., Ost MC. Timing and predictors for urinary drainage in children with expectantly managed grade IV renal trauma. J Urol. 2014;192(2):512–517.
- Gerstenbluth RE, Spirnak JP, Elder JS. Sports participation and high grade renal injuries in children. J Urol. 2002;168(6):2575–2578.
- Ozturk H, Dokucu AI, Onen A, Otçu S, Gedik S, Azal OF. Non-operative management of isolated solid organ injuries due to blunt abdominal trauma in children: a fifteen-year experience. Eur J Pediatr Surg. 2004;14(1):29–34.
- Wan J, Corvino TF, Greenfield SP, DiScala C. The incidence of recreational genitourinary and abdominal injuries in the Western New York pediatric population. J Urol. 2003;170(4 Pt 2):1525–1527; discussion 1527.
- Keller MS, Green MC. Comparison of short- and long-term functional outcome of nonoperatively managed renal injuries in children. J Pediatr Surg. 2009;44(1):144–147; discussion 147.
- El-Sherbiny MT, Aboul-Ghar ME, Hafez AT, Hammad AA, Bazeed MA. Late renal functional and morphological evaluation after non-operative treatment of high-grade renal injuries in children. BJU Int. 2004;93(7):1053–1056.
- Kitase M, Mizutani M, Tomita H, Kono T, Sugie C, Shibamoto Y. Blunt renal trauma: comparison of contrast-enhanced CT and angiographic findings and the usefulness of transcatheter arterial embolization. Vasa. 2007;36(2):108–113.
- Kiankhooy A, Sartorelli KH, Vane DW, Bhave AD. Angiographic embolization is safe and effective therapy for blunt abdominal solid organ injury in children. J Trauma. 2010;68(3):526–531.
- Schuster T, Leissner G. Selective angioembolization in blunt solid organ injury in children and adolescents: review of recent literature and own experiences. Eur J Pediatr Surg. 2013;23(6):454–463.
- Fuchs ME, Anderson RE, Myers JB, Wallis MC. The incidence of long-term hypertension in children after high-grade renal trauma. J Pediatr Surg. 2015;50(11):1919–1921.
- Kuan JK, Wright JL, Nathens AB, Rivara FP, Wessells HAmerican Association for the Surgery of Trauma. American Association for the Surgery of Trauma Organ Injury Scale for kidney injuries predicts nephrectomy, dialysis, and death in patients with blunt injury and nephrectomy for penetrating injuries. J Trauma. 2006;60(2):351–356.
- Santucci RA, Wessells H, Bartsch G, Descotes J, Heyns CF, McAninch JW, Nash P, Schmidlin F. Evaluation and managementof renal injuries: consensus statement of the renal trauma subcommittee. BJU Int. 2004;93(7):937–954.
- Notrica DM. Pediatric blunt abdominal trauma: current management. Curr Opin Crit Care. 2015;21(6):531–537.
- Graziano KD, Juang D, Notrica D, Grandsoult VL, Acosta J, Sharp SW, Murphy JP, St Peter SD. Prospective observational study with an abbreviated protocol in the management of blunt renal injury in children. J Pediatr Surg. 2014;49(1):198–200; discussion 200−1.
- Notrica DM, Linnaus ME. Nonoperative Management of Blunt Solid Organ Injury in Pediatric surgery. Surg Clin North Am. 2017;97(1):1–20.
- Schwartz MJ, Smith EB, Trost DW, Vaughan ED. Renal artery embolization: clinical indications and experience from over 100 cases. BJU Int. 2007;99(4):881–886.
- Karlsberg RP, Dohad SY, Sheng R, Iodixanol Peripheral CTA Study Investigator Panel. Contrast-induced acute kidney injury (CI-AKI) following intra-arterial administration of iodinated contrast media. J Nephrol. 2010;23(6):658–666.
- Breyer BN, McAninch JW, Elliott SP, Master VA. Minimally invasive endovascular techniques to treat acute renal hemorrhage. J Urol. 2008;179(6):2248–2252; discussion 2253.
- Gor RA, Styskel BA, Li T, Canter DJ, Simhan J. Unexpected high rates of angiography and angioembolization for isolated low-grade renal trauma: results from a large, statewide, trauma database. Urology. 2016;97:92–97.
- Strauss KJ, Kaste SC. The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients—a white paper executive summary. Radiology. 2006;240(3):621–622.
- Dugi DD 3rd, Morey AF, Gupta A, Nuss GR, Sheu GL, Pruitt JH. American Association for the Surgery of Trauma grade 4 renal injury substratification into grades 4a (low risk) and 4b (high risk). J Urol. 2010;183(2):592–597.
- Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3).
Keywords:
Pediatric renal trauma; angioembolization; management; posttraumatic renal hypertension
© 2019 Lippincott Williams & Wilkins, Inc.