Prehospital spine immobilization/spinal motion restriction in penetrating trauma
Published 2018
Citation: J Trauma. 84(5):736-744, May 2018
Authors
Velopulos, Catherine, G., MD, MHS; Shihab, Hasan, M., MPH; Lottenberg, Lawrence, MD; Feinman, Marcie, MD; Raja, Ali, MD, MBA, MPH; Salomone, Jeffrey; Haut, Elliott, R., MD, PhD
Abstract
BACKGROUND Spine immobilization in trauma has remained an integral part of most emergency medical services protocols despite a lack of evidence for efficacy and concern for associated complications, especially in penetrating trauma patients. We reviewed the published evidence on the topic of prehospital spine immobilization or spinal motion restriction in adult patients with penetrating trauma to structure a practice management guideline.
METHODS We conducted a Cochrane style systematic review and meta-analysis and applied Grading of Recommendations, Assessment, Development, and Evaluation methodology to construct recommendations. Qualitative and quantitative analyses were used to evaluate the literature on the critical outcomes of mortality, neurologic deficit, and potentially reversible neurologic deficit.
RESULTS A total of 24 studies met inclusion criteria, with qualitative review conducted for all studies. We used five studies for the quantitative review (meta-analysis). No study showed benefit to spine immobilization with regard to mortality and neurologic injury, even for patients with direct neck injury. Increased mortality was associated with spine immobilization, with risk ratio [RR], 2.4 (confidence interval [CI], 1.07–5.41). The rate of neurologic injury or potentially reversible injury was very low, ranging from 0.002 to 0.076 and 0.00034 to 0.055, with no statistically significant difference for neurologic deficit or potentially reversible deficit, RR, 4.16 (CI, 0.56–30.89), and RR, 1.19 (CI, 0.83–1.70), although the point estimates favored no immobilization.
CONCLUSION Spine immobilization in penetrating trauma is associated with increased mortality and has not been shown to have a beneficial effect on mitigating neurologic deficits, even potentially reversible neurologic deficits. We recommend that spine immobilization not be used routinely for adult patients with penetrating trauma.
LEVEL OF EVIDENCE Systematic review with meta-analysis study, level III.
KEYWORDS Guidelines; penetrating trauma; spine immobilization; spinal motion restriction
Author Information
From the Department of Surgery, University of Colorado School of Medicine, Aurora, Colorado (C.G.V.); Combined Family Medicine and Preventive Medicine Residency Program, MedStar Franklin Square Medical Center, and Johns Hopkins University School of Public Health, Baltimore, Maryland (H.M.S.); Department of Surgery, St. Mary’s Medical Center, West Palm Beach, Florida (L.L.); Department of Surgery, Sinai Surgery and ICU Associates, Baltimore, Maryland (M.F.); Department of Emergency Medicine, Massachusetts General Hospital, and Harvard Medical School, Boston, Massachusetts (A.R.); Department of Surgery, Banner Desert Medical Center, Mesa, Arizona (J.S.); Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, Maryland (E.R.H.); Department of Anesthesiology & Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland (E.R.H.), Department of Emergency Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland (E.R.H.); The Armstrong Institute for Patient Safety, Johns Hopkins Medicine, Baltimore, Maryland (E.R.H.); and Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland (E.R.H.).
Submitted: September 15, 2017, Revised: November 20, 2017, Accepted: November 24, 2017, Published online: December 28, 2017.
Address for reprints: Catherine Garrison Velopulos, MD, MHS, FACS, University of Colorado School of Medicine, Trauma, Acute Care Surgery, and Critical Care, 12631 E 17th St, Room 6001, Aurora, Colorado 80045; email: Catherine.Velopulos@ucdenver.edu.
Presented at Eastern Association for the Surgery of Trauma 30th Annual Scientific Assembly, January 10-14, 2017, Hollywood, FL.
Overview
Spine immobilization in trauma has remained an integral part of most emergency medical services (EMS) protocols despite a lack of evidence for efficacy and concern for associated complications, especially in penetrating traumapatients. Several studies have shown that, even with proper application, functional immobilization is not actually achieved, prompting an impending change in terminology to “spinal motion restriction” and further pushing the risk/benefit ratio away from recommending the use of cervical spine collars and longboards.[1–5]
There is an increasing call to end the routine use of spine immobilization in patients who would not benefit given the associated risks related to local pressure injury, increased intracranial pressure, covering penetrating wounds leading to missed injury, and decreasing or delaying the success of lifesaving procedures such as endotracheal intubation, particularly in patients who are victims of penetrating trauma.[6–12] For instance, one study assessing patterns of error that lead to trauma mortality cites a 16% failure to secure an airway, which is known to be more difficult in immobilized patients.[13] Aside from the potential complications, we know that most penetrating injuries to the spine represent complete injury that will not be modified by prehospital immobilization.[13–16] Even the injuries deemed unstable and requiring operative fixation are not helped by immobilization with cervical collar or spine board since these methods are not particularly effective. A recent cost-utility analysis reinforced this knowledge and showed that not only is spine immobilization not cost-effective, it does not change the outcome for these patients.[14]
Despite evidence that prehospital spine immobilization is not advantageous, and may indeed be harmful, a recent study examining EMS providers and emergency department personnel attitudes and knowledge about the topic revealed that most of this evidence is not known, although attitudes and practice about immobilization varied the most depending on the priority the provider placed on time to definitive care.[15] Other groups have written guidelines on this topic[16] [17]; however, none have used the robust Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology or performed a meta-analysis.
Based on data, many large, regional systems have already eliminated the use of cervical collars or spine boards in penetrating trauma.[18] We sought to review the published evidence on the topic of prehospital spine immobilization or spinal motion restriction in patients with penetrating trauma to structure a guideline with the potential to change practice nationwide and eliminate its use in this patient population.
Methods
Objectives
This guideline was created using the GRADE methodology for guideline creation as required by the Eastern Association for the Surgery of Trauma (EAST).[19] The objective of this guideline is to evaluate whether nonoperative spine immobilization of any type is beneficial or harmful in penetrating trauma patients. The population (P), intervention (I), comparator (C), and outcome (O) (PICO) questions are defined below:
PICO Question 1: In adult penetrating trauma patients, does spine immobilization versus no spine immobilization decrease mortality?
PICO Question 2: In adult penetrating trauma patients, does spine immobilization versus no spine immobilizationdecrease the incidence of neurologic deficit or the incidence of potentially reversible deficit?
Choosing the Outcome
According to GRADE methodology, outcomes were chosen by the team and rated in importance from 1 to 9, with 7 to 9 representing a critical outcome and 4 to 6 representing an important outcome. The votes of each member of the team were considered equally, and then a score was assigned to each outcome based on the collective conclusion. The outcomes considered were mortality, neurologic deficit, potentially reversible neurologic deficit, missed injury, and failed intubation. The outcomes rated as critical included mortality, neurologic deficit, and potentially reversible neurologic deficit. Potentially reversible deficits were defined as neurologic deficits that could possibly be either improved or entirely reversed with definitive spine immobilization. Outcomes considered important were missed injury and failed intubation, each with a score of 6. There were no other outcomes that the team included, and no outcomes rated less than a 6.
Criteria for Considering Studies for this Review
Type of Studies
We considered randomized controlled trials, prospective observational or retrospective studies, and case-control studies. Only studies pertaining to the treatment of penetrating trauma patients (gunshot or stab wound) were included.
Type of Participants
We included studies with adult patients, of either sex, and with no restriction by ethnicity or comorbidities. Because patients as young as 13 are treated as adults in many centers, these patients were included as adults. Since 13 is commonly used as a cutoff point and was a distinct and consistent cutoff in the reviewed literature, this was decided as a reasonable age criteria for inclusion. Studies consisting solely of pediatric patients were excluded, and there were no studies that mixed adult and pediatric population younger than 13 years. Meta-analyses, case reports, letters, and reviews containing no original data or comments were excluded.
Type of Intervention
We included studies if spine immobilization was studied in comparison with no immobilization. Spine immobilization was defined as cervical collar and/or longboard.
Type of Outcome Measures
Primary Outcome Measure
The three primary outcomes were mortality, neurologic deficit, or potentially reversible neurologic deficit after spine immobilization versus no immobilization after penetrating trauma.
Secondary Outcome Measures
Secondary outcomes considered were missed injury and failed intubation; however, all were deemed to be noncritical for decision making in the GRADE framework.
Search Methods for Identification of Studies
Electronic Searches
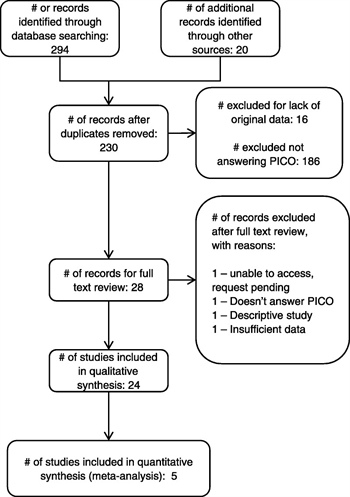
Figure 1. PRISMA diagram.
The PRISMA flow diagram for study selection is shown in Figure 1. A professional librarian conducted a systematic search using the PubMed, Embase, and the Cochrane Library databases for studies with publication dates from January 1, 1980 through February 28, 2017. The search used the following medical subject headings (MESH) terms: Penetrat*[All Fields] AND ("injuries"[Subheading] OR "injuries"[All Fields] OR "trauma"[All Fields] OR "wounds and injuries"[MeSH Terms] OR “wound” OR “wound” OR “injury” OR "wounds and injuries"[All Fields]) AND ("immobilisation"[All Fields] OR "immobilization"[MeSH Terms] OR "immobilization"[All Fields]). We did not restrict by language or country of publication, although all studies retrieved were in English.
We used the “related articles” function to broaden the search and scanned all citations for relevance. In addition, we repeated the search using the term “spinal motion restriction,” as this is a newer term to describe the practice. Because this did not yield any studies using this terminology, spine immobilization will remain the language used throughout the rest of this review. Finally, in addition to the electronic search, we hand searched the bibliographies of recent reviews and papers selected for analysis.
Methods of the Review
Selection of Studies
After completing the electronic literature search, two independent reviewers screened titles and abstracts, applying inclusion criteria. Any disagreement on inclusion was resolved by consensus of at least three members of the group. The resulting studies then underwent full-text review, again by two independent reviewers, to determine appropriateness for inclusion, and the bibliographies were hand searched for additional articles. Review articles were screened for studies not already included in the electronic search.
Data Extraction and Management
A subgroup committee appointed by the Chair of the EAST Guidelines Committee was responsible for reading and grading the articles included. All the reviewers are authors of the present manuscript.
Using a form developed by the team, two independent reviewers extracted information from the studies into Microsoft Excel (Microsoft, Redmond, Washington) using double data entry for accuracy. We then entered these into Review Manager X.6 (RevMan, Cochrane Community, London, UK). Variables collected included information on the authors, study number, country of the study, the methodology of the study, the population, intervention, and the relevant outcome measures.
Assessment of Methodological Quality of the Included Studies
The articles were evaluated using the GRADE system.[19] The GRADE system describes four levels of quality of evidence. When rating the quality of evidence, decision makers must consider the confidence in the estimate of each effect and whether or not these estimates are likely to be correct. The four levels of quality are high, moderate, low, and very low. Recommendations are made based on the GRADE methodology in the following domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The data were entered into GRADEpro (Cochrane Community, London, UK) to generate evidence tables.
Strong recommendations are prefaced by the statement “we recommend”, and weak recommendations are prefaced by the statement “we suggest” or “we conditionally recommend,” as per the GRADE methodology. These recommendations are based not only on the quality of the evidence and the risk versus benefit ratio but also on patient values and preferences.
Measures of Treatment Effect
We reported outcomes as risk ratios (RRs), with associated 95% confidence intervals (CIs) and p values. The unit of analysis was individual patients.
Assessment of Heterogeneity
Potential heterogeneity exists due to population differences, different types of surgery performed, and how patients are defined. We examined these differences across studies to assess the clinical and methodological heterogeneity. For the meta-analysis (see subsection “Data Synthesis (Meta-analysis)” below), we used RevMan to calculate the Q statistic, and then the I [2] statistic (%) was used to determine the proportion of variation between studies attributable to heterogeneity, and categorized as low (25–49%), moderate (50–74%), or high (74–100%). We also used the χ[2] test for heterogeneity and examined the CIs for overlap, with decreasing overlap representing increasing heterogeneity.
Data Synthesis (Meta-analysis)
If heterogeneity was “moderate” to “high,” we examined whether pooling the data was appropriate, and we performed a qualitative narrative summary of results. Based on methodological and clinical similarity, we performed meta-analysis for the outcome for each PICO question. We used the DerSimonian and Laird random effects model method, as our studies did not uniformly share a common effect size, and unknown influential factors could vary across studies (unknown confounders). This allowed us to incorporate both the within-study variability and between-study variability, along a distribution of “true” effects, which weighs larger and smaller studies more evenly.
Results
Search Results
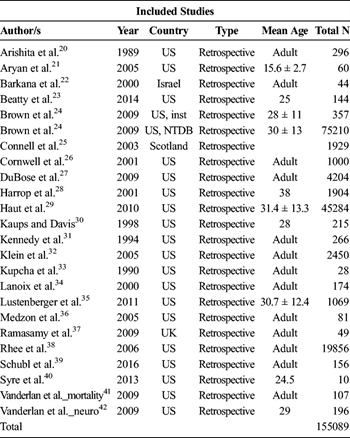
Table 1. Studies Included in Qualitative and/or Quantitative Synthesis.
A total of 314 records were identified and screened (Fig. 1). After excluding duplicates, those lacking original data and those not addressing the PICO questions, 28 records underwent full-text review. After further exclusions, a total of 24 studies (Table 1) were included in qualitative synthesis, with five of these also included in the quantitative synthesis (meta-analysis).[20–42]
Qualitative Analysis

Table 2. Event Rates for Studies Reporting Neurologic Outcomes.
Qualitative analysis was performed for the outcomes of mortality, neurologic deficit, potentially reversible neurologic deficit, missed injury, and failed intubation. No study showed benefit to spine immobilization with regard to mortality and neurologic injury, even for patients with direct neck injury. The rate of neurologic injury was generally very low whether patients had spine immobilization or not, with the incidence overall ranging from approximately 2 of 1000 to 76 of 1000 for all comers. Predictably, incidence was much higher in studies selecting for populations with a higher risk of neurologic injury, with an incidence of 136 of 1000 to 204 of 1000 in studies specifically targeting patients with injuries to the head and neck. One study only included patients with neurologic injury. Despite varying rates of injury, the proportion of potentially reversible neurologic injury was consistently very low across all of the studies reporting neurologic outcomes, ranging from 3.4 of 10,000 to 550 of 10,000 (Table 2). Schubl et al.,[39] who examined patients with firearm injury to the head and/or neck, concluded that cervical spine immobilization might be of value; however, of the two patients with unstable fractures, while one of them developed transient neurologic symptoms, it was later in the course and would not have been affected by prehospital care.
Arishita et al.[20] noted that intubation takes two EMS providers 5.64 + 1.49 minutes to perform correctly in the setting of immobilization. Kaups and Davis[30] similarly noted the association with spine immobilization and intubation, where multiple intubation attempts resulted with greater frequency in immobilized patients: 49 attempts in 34 patients versus 5 attempts in 4 patients who were not immobilized.
Some large database studies have suggested that spine immobilization in penetrating trauma may not be beneficial and may, in fact, be potentially harmful. Haut et al.[29] in a National Trauma Data Bank study showed that the number needed to treat to potentially benefit just one penetrating trauma patient is 1032. In contrast, the number needed to treat to potentially contribute to one death was only 66. Cornwell et al.[26] looked at 1000 patients in Maryland with torso gunshot wounds and found that only two patients required operative vertebral column stabilization but that given the almost uniformly complete injury sustained with this mechanism, “thoracolumbar immobilization is almost never beneficial in patients with torso GSW [gunshot wounds]” and “the role of formal thoracolumbar immobilization should be reexamined.”[26]
A recent study by Beatty et al. of 144 patients with GSW to the neck closely examined progression of injury. Complete spinal cord injury was noted in 28 patients. Fourteen patients underwent intervention for incomplete injury; of these, two had measured deterioration during their course, but this was noted to be from compression from the bullet rather than concern over movement of the neck, and both had marked recovery after decompression. Three of the patients who underwent operative stabilization with incomplete injury improved by one level. There were no patients with deterioration or improvement attributed to nonoperative immobilization.[23] Another recent study by Syre et al.[40] examined patients with atlanto-occipital injury. Only one of these patients presented with unstable injury, and the two patients with deficits had delayed presentation after several days that would not have been affected by prehospital spine immobilization.
These studies all purportedly exclude blunt trauma, although minor blunt trauma may have been present. Across these studies, there is the suggestion that minor blunt trauma can be exempted from immobilization as well; but none of the studies in this review examined this question closely enough to draw any conclusion.
Quantitative Analysis
Quantitative analysis was performed for the outcomes of mortality, neurologic deficit, and potentially reversible neurologic deficit. No benefit to spine immobilization was found with regard to these outcomes. There were insufficient data to perform a meta-analysis with regard to failed intubation or missed injury.
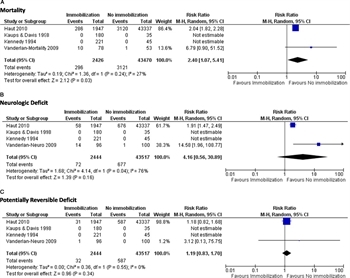
Figure 2. (A–C) Forest plots.
For mortality, only four studies had sufficient data points to complete the meta-analysis.[29–31] [41] Because two studies had no mortality in either group, the pooled estimate relied heavily on two studies, but these represented 43,390 patients, with a relative risk of 2.4 (CI, 1.07–5.41) for increased mortality associated with spine immobilization, shown in Figure 2A. Because one study contributed the vast number of events, thus being disproportionately represented, a random effects model was used to account for variation in study size and relative contribution. Because the point estimates are in the same direction, this is a fair representation of the conclusions of both studies.
For neurologic deficits, there were also four studies meeting criteria for inclusion with sufficient data points for the meta-analysis.[29–31] [42] There was no statistically significant difference between spine immobilization versus no immobilization, although the point estimate was in favor of no immobilization (RR, 4.16; CI, 0.56–30.89; Fig. 2B). The failure to meet statistical significance is likely due to across-study variability, as the point estimates were quite significant for the unpooled studies (RR, 1.91; CI, 1.47–2.49 and RR, 14.58; CI, 1.96–108.77), and a more conservative random effects model was used. The data were pooled in the setting of a moderate to high I [2] to visually highlight this heterogeneity contributing to lack of statistical significance. Finally, no difference was seen for potentially reversible deficits (Fig. 2C), with RR 1.19 (CI 0.83, 1.70) and minimal heterogeneity across the studies.
Grading the Evidence

Table 3. Question: Spine Immobilization Versus No Spine Immobilization for Penetrating Trauma.
The GRADE evidence table is shown in Table 3. For the outcome of mortality, rated by the group as a critical outcome, the included studies were rated as having no serious risk of bias, and no serious inconsistency, indirectness, or imprecision. No publication bias was detected. In fact, given previous assumptions and protocols endorsing the benefits of spine immobilization, one might expect that these studies would have been at risk for nonpublication for arriving at the opposite conclusion. Given no downgrades in these areas of study quality, and due to a large magnitude of effect, the quality of the evidence was upgraded from the starting point of low for observational studies to moderate. For neurologic deficit, also a critical outcome, included studies were rated as having no serious risk of bias, and no serious inconsistency, indirectness, or publication bias. Due to the wide CIs, however, as well as potential confounding by indication, the evidence was downgraded from the starting point of low for observational studies to very low. For the additional critical outcome of potentially reversible neurologic deficit, there was no serious risk of bias, including publication bias, detected. There was also no serious indirectness noted, but because of inconsistency related to variation in the definition of “potentially reversible” across the studies, and imprecision related to wide CIs and the rareness of the event rate, the evidence for this outcome was also downgraded from the starting point of low for observational studies to very low.
Discussion
Similar to previous reviews, routine spine immobilization in penetrating trauma is not of benefit and may be harmful. The most striking finding of this systematic review is that mortality is clearly associated with spine immobilization. Some studies suggest that this may be related to the injuries themselves, while others suggest that immobilization hampers the ability of providers to care appropriately for the patient as it can obscure injury, make necessary life-saving procedures more difficult, and delay transportation to definitive surgical care at a trauma center.
Importantly, we cannot show that spine immobilization is beneficial with regard to critical outcomes related to neurologic deficits. Although not discussed in this review specifically, multiple studies not done directly on patients, but looking at the mechanics of spine immobilization, demonstrate that the available methods are not effective in eliciting the degree of immobilization that would be necessary to be even theoretically effective.[43] [44] Although the level of evidence is low, when one intervention shows no benefit over another and is done solely by tradition, there is a reasonable argument for its removal from standard practice.
All of the studies in this area are observational; there have been no randomized controlled trials of immobilization versus nonimmobilization. Most studies assume spine immobilization was performed since it was the protocol in most areas at the time of the studies, which may not have always been the case. Few of the studies specify the type or extent of immobilization, whether with cervical collar, longboard, or other types of immobilization devices. Further complicating analysis instead of directly comparing interventions, many of the studies only look at projected risk versus benefit by assessing which patients did or did not have any injury. Assumptions vary as to what constitutes “potential benefit,” particularly with regard to “potentially preventable neurologic deficit.” For instance, some studies use surgical fixation as a surrogate end point for reversible neurologic disease, but the studies actually examining this rate demonstrate that surgical fixation may halt or prevent, but not reverse, injury that has already occurred.
Recommendation

Table 4. Summary of Findings and Recommendation.
We recommend that spine immobilization not be used routinely for adult patients with penetrating trauma, as it is associated with increased mortality and has no benefit in preventing neurologic deterioration (Table 4). This strong recommendation is based on the assumption that most patients (although not all) would place a higher value on survival, even with potential neurologic deficits. The strength of the recommendation is based on magnitude of effect, assumption of patient preference, and the favorable risk/benefit profile.
Conclusion
Spine immobilization in adult penetrating trauma patients is associated with increased mortality and has not been shown to have a beneficial effect on mitigating neurologic deficits, even potentially reversible neurologic deficits. We recommend that spine immobilization not be used routinely for adult patients with penetrating trauma.
Authorship
C.G.V. and E.R.H. conceptualized the study. C.G.V. and E.R.H. created the PICO questions. C.G.V., L.L., M.F., J.S, and E.R.H. voted regarding the outcomes of interest for these PICO questions. C.G.V. and H.M.S. evaluated the articles independently for secondary outcomes. C.G.V., H.M.S., and ERH performed the literature search, read all of the abstracts, and selected the articles for review, as well as reviewed and summarized the selected articles. C.G.V. and H.M.S. extracted the data from the selected articles. C.G.V. entered the extracted data into the RevMan and GRADEpro programs and evaluated the results for recommendations. C.G.V. and E.R.H. wrote the manuscript. A.R., H.M.S., L.L., J.S., and E.R.H. reviewed this manuscript for methodological content and made critical revisions to the final draft. All authors participated in the critical review of all versions of this paper.
Acknowledgements
The authors thank the Eastern Association for the Surgery of Trauma (EAST) for the opportunity to write this manuscript, the specialized training provided to the authors regarding the GRADE method, and the detail-oriented peer review of multiple versions of this manuscript by the Guidelines Committee.
Disclosure
The authors declare no conflicts of interest.
Dr Haut is supported by a research grant (1R01HS024547) from the Agency for Healthcare Research and Quality (AHRQ) titled “Individualized Performance Feedback on Venous Thromboembolism Prevention Practice.” Dr Haut is also supported by a contract (CE-12-11-4489) from the Patient-Centered Outcomes Research Institute (PCORI) titled “Preventing Venous Thromboembolism: Empowering Patients and Enabling Patient-Centered Care via Health Information Technology.”
Dr Haut receives royalties from Lippincott Williams & Wilkins for a book—"Avoiding Common ICU Errors". He is a paid consultant and speaker for the “Preventing Avoidable Venous Thromboembolism—Every Patient, Every Time” VHA IMPERATIV® Advantage Performance Improvement Collaborative and the Illinois Surgical Quality Improvement Collaborative "ISQIC."
Dr Haut was the paid author of a paper commissioned by the National Academies of Medicine titled “Military Trauma Care’s Learning Health System: The Importance of Data Driven Decision Making,” which was used to support the report titled “A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury.”
None of these funding sources contributed to this work.
References
- Voss S, Page M, Benger J. Methods for evaluating cervical range of motion in trauma settings. Scand J Trauma Resusc Emerg Med. 2012;20:50.
- James CY, Riemann BL, Munkasy BA, Joyner AB. Comparison of cervical spine motion during application among four rigid immobilisation collars. J Athl Train. 2004;39:138–145.
- Tescher AN, Rindflesch AB, Youdas JW, Terman RW, Jacobson TM, Douglas LL, Miers AG, Austin CM, Delgado AM, Zins SM, et al. Range-of-motion restriction and craniofacial tissue-interface pressure from four cervical collars. J Trauma. 2007;63:1120–1126.
- Hostler D, Colburn D, Seitz SR. A comparison of three cervical immobilization devices. Prehosp Emerg Care. 2009;13:256–260.
- Lerner EB, Billittier AJ 4th, Moscati RM. The effects of neutral positioning with and without padding on spinal immobilization of healthy subjects. Prehosp Emerg Care. 1998;2(2):112–116.
- Liew SC, Hill DA. Complication of hard cervical collars in multi-trauma patients. Aust N Z J Surg. 1994;64:139–140.
- Murphy KM, Musiak H, Hanlon M. Patient with occipital pressure ulcer requiring continued cervical collar use. J Wound Ostomy Continence Nurs. 1997;24:58–60.
- Jacobson TM, Tescher AN, Miers AG, Downer L. Improving practice: efforts to reduce occipital pressure ulcers. J Nurs Care Qual. 2008;23:283–288.
- Hunt K, Hallworth S, Smith M. The effects of rigid collar placement on intracranial and cerebral perfusion pressures. Anaesthesia. 2001;56:511–513.
- Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury. 1996;27:647–649.
- Ho AM, Fung KY, Joynt GM, Karmakar MK, Peng Z. Rigid cervical collar and intracranial pressure of patients with severe head injury. J Trauma. 2002;53:1185–1188.
- March JA, Ausband SC, Brown LH. Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002;6(4):421–424.
- Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006;244(3):371–380.
- Garcia A, Liu TH, Victorino GP. Cost-utility analysis of prehospital spine immobilization recommendations for penetrating trauma. J Trauma Acute Care Surg. 2013;76(2):534–541.
- Bouland AJ, Jenkins JL, Levy MJ. Assessing attitudes toward spinal immobilization. J Emerg Med. 2013;45(4):117–125.
- Stuke LE, Pons PT, Guy JS, Chapleau WP, Butler FK, McSwain NE. Prehospital spine immobilization for penetrating trauma—review and recommendations from the Prehospital Trauma Life Support Executive Committee. J Trauma. 2011;71(3):763–769.
- Kornhall DK, Jørgensen JJ, Brommeland T, Hyldmo PK, Asbjørnsen H, Dolven T, Hansen T, Jeppesen E. The Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med. 2017;25(1):2.
- Trauma Protocol: Spinal Protection. The Maryland Medical Protocols for Emergency Medical Services Providers. Available at: www.miemss.org. Accessed August 4, 2016.
- Kerwin AJ, Haut ER, Burns JB, et al. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73:S283–S287.
- Arishita GI, Vayer JS, Bellamy RF. Cervical spine immobilization of penetrating neck wounds in a hostile environment. J Trauma. 1989;29(3):332–337.
- Aryan HE, Amar AP, Ozgur BM, Levy ML. Gunshot wounds to the spine in adolescents. Neurosurgery. 2005;57(4):748–752.
- Barkana Y, Stein M, Scope A, Maor R, Abramovich Y, Friedman Z, Knoller N. Prehospital stabilization of the cervical spine for penetrating injuries of the neck—is it necessary? Injury. 2000;31(5):305–309.
- Beaty N, Slavin J, Diaz C, Zeleznick K, Ibrahimi D, Sansur CA. Cervical spine injury from gunshot wounds. J Neurosurg Spine. 2014;21(3):442–449.
- Brown JB, Bankey PE, Sangosanya AT, Cheng JD, Stassen NA, Gestring ML. Prehospital spinal immobilization does not appear to be beneficial and may complicate care following gunshot injury to the torso. J Trauma. 2009;67(4):774–778.
- Connell RA, Graham CA, Munro PT. Is spinal immobilisation necessary for all patients sustaining isolated penetrating trauma? Injury. 2003;34(12):912–914.
- Cornwell EE 3rd, Chang DC, Bonar JP, Campbell KA, Phillips J, Lipsett P, Scalea T, Bass R. Thoracolumbar immobilization for trauma patients with torso gunshot wounds: is it necessary? Arch Surg. 2001;136:324–327.
- DuBose J, Teixeira PG, Hadjizacharia P, Hannon M, Inaba K, Green DG, Plurad D, Demetriades D, Rhee P. The role of routine spinal imaging and immobilisation in asymptomatic patients after gunshot wounds. Injury. 2009;40:860–863.
- Harrop JS, Sharan AD, Vaccaro AR, Przybylski GJ. The cause of neurologic deterioration after acute cervical spinal cord injury. Spine (Phila Pa 1976). 2001;26(4):340–346.
- Haut ER, Kalish BT, Efron DT, Haider AH, Stevens KA, Kieninger AN, Cornwell EE 3rd, Chang DC. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68(1):115–121.
- Kaups KL, Davis JW. Patients with gunshot wounds to the head do not require cervical spine immobilization and evaluation. J Trauma. 1998;44(5):865–867.
- Kennedy FR, Gonzalez P, Beitler AL, Sterling-Scott R, Fleming AW. Incidence of cervical spine injury in patients with gunshot wounds to the head. South Med J. 1994;87(6):621–623.
- Klein Y, Cohn SM, Soffer D, Lynn M, Shaw CM, Hasharoni A. Spine injuries are common among asymptomatic patients after gunshot wounds. J Trauma. 2005;58(4):833–836.
- Kupcha PC, An HS, Cotler JM. Gunshot wounds to the cervical spine. Spine. 1990;15(10):1058–1063.
- Lanoix R, Gupta R, Leak L, Pierre J. C-spine injury associated with gunshot wounds to the head: retrospective study and literature review. J Trauma. 2000;49(5):860–863.
- Lustenberger T, Talving P, Lam L, Kobayashi L, Inaba K, Plurad D, Branco BC, Demetriades D. Unstable cervical spine fracture after penetrating neck injury: a rare entity in an analysis of 1,069 patients. J Trauma. 2011;70(4):870–872.
- Medzon R, Rothernhaus T, Bono CM, Grindlinger G, Rathlev NK. Stability of cervical spine fractures after gunshot wounds to the head and neck. Spine. 2005;30(20):2274–2279.
- Ramasamy A, Midwinter M, Mahoney P, Clasper J. Learning the lessons from conflict: pre-hospital cervical spine stabilisation following ballistic neck trauma. Injury. 2009;40(12):1342–1345.
- Rhee P, Kuncir EJ, Johnson L, Brown C, Velmahos G, Martin M, Wang D, Salim A, Doucet J, Kennedy S, et al. Cervical spine injury is highly dependent on the mechanism of injury following blunt and penetrating assault. J Trauma. 2006;61(5):1166–1170.
- Schubl SD, Robitsek RJ, Sommerhalder C, Wilkins KJ, Klein TR, Trepeta S, Ho VP. Cervical spine immobilization may be of value following firearm injury to the head and neck. Am J Emerg Med. 2016;34:726–729.
- Syre P 3rd, Rodriguez-Cruz L, Desai R, Greene KA, Hurst R, Schuster J, Malhotra NR, Marcotte P. Civilian gunshot wounds to the atlantoaxial spine: a report of 10 cases treated using a multidisciplinary approach. J Neurosurg Spine. 2013;19(6):759–766.
- Vanderlan WB, Tew BE, McSwain NE Jr. Increased risk of death with cervical spine immobilisation in penetrating cervical trauma. Injury. 2009;40(8):880–883.
- Vanderlan WB, Tew BE, Seguin CY, Mata MM, Yang JJ, Horst HM, Obeid FN, McSwain NE. Neurologic sequelae of penetrating cervical trauma. Spine. 2009;34(24):2646–2653.
- Mazolewski P, Manix TH. The effectiveness of strapping techniques in spinal immobilization. Ann Emerg Med. 1994;23(6):1290–1295.
- Chan D, Goldberg R, Tascone A, Harmon S, Chan L. The effect of spinal immobilization on healthy volunteers. Ann Emerg Med. 1994;23(1):48–51.