Rib Fractures, Open Reduction and Internal Fixation of (UPDATE IN PROCESS)
Published 2017
Citation: J Trauma. 82(3):618-626, March 2017
Authors
Kasotakis, George MD, MPH; Hasenboehler, Erik A. MD; Streib, Erik W. MD; Patel, Nimitt MD; Patel, Mayur B. MD, MPH; Alarcon, Louis MD; Bosarge, Patrick L. MD; Love, Joseph MD; Haut, Elliott R. MD, PhD; Como, John J. MD, MPH
Objectives
Our population, intervention, comparator, and outcome (PICO) questions are defined as follows:
* Population: adult patients (>18 years of age) with rib fractures following blunt trauma.
* Intervention: operative fixation of fractured ribs.
* Comparator: nonoperative management.
* Outcomes: mortality; duration of mechanical ventilation (DMV); ICU and hospital length of stay (LOS); incidence of pneumonia; need for tracheostomy; and pain control.
* PICO Question 1: In adult patients with flail chest after blunt trauma, should rib ORIF be performed (versus nonoperative management) to decrease mortality; DMV, ICU LOS, and hospital LOS; incidence of pneumonia and need for tracheostomy; and improve pain control?
* PICO Question 2: In adult patients with nonflail rib fractures after blunt trauma, should rib ORIF be performed (versus nonoperative management) to decrease mortality and incidence of pneumonia; shorten DMV, hospital LOS; improve pain control; and decrease need for tracheostomy if applicable?
Identification of References
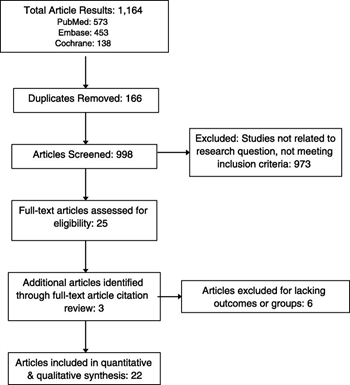
Figure 1. PRISMA flow diagram for study selection for analysis.
Our systematic review was registered with the PROSPERO registry of systematic reviews and meta-analyses (Registration No. CRD42014015575). Subsequently, , Embase, and the Cochrane databases were searched in duplicate by professional librarians from two medical schools (Boston University and Harvard University) on January 29, 2016. The following medical subject headings (MeSH) terms were included: rib fracture, flail chest, fracture treatment, surgical management, fixation, plating, ORIF in various combinations.1 No restrictions were placed on language. The ranges for our literature search were from January 1900 to January 2016. Prospective trials and retrospective cohort/case-control studies that compared rib ORIF versus nonoperative management of rib fractures in adults with either flail and/or nonflail chest patients were eligible for inclusion and were retrieved. Case reports, commentaries, and animal studies were excluded, as were studies describing operative technique alone, and reviews. The reference lists of retrieved papers were also screened to identify additional studies. For a study to be included in our final analysis, a clear comparison between operative versus nonoperative subjects had to be present and at least one of the critical outcomes reported.
Upon completion of the electronic literature search, citation lists were independently reviewed by two authors (G.K., M.B.P.) to identify potentially relevant studies. Titles and abstracts were screened, and full articles were reviewed as needed. Any disagreement on inclusion was resolved by consensus (Fig. 1).
Outcome Measures
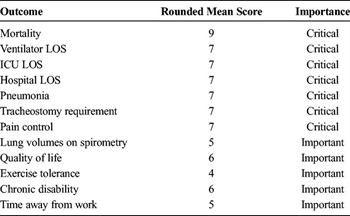
TABLE 1. Classification of Important Outcomes in Patients With Rib Fractures After Blunt Trauma Undergoing Rib ORIF for PICO 1 (Rib ORIF in Trauma Patients With Flail Chest) and PICO 2 (Rib ORIF in Trauma Patient With Nonflail Rib Fractures)
Numerous candidate outcomes (including in-hospital mortality; DMV, ICU LOS, and hospital LOS; incidence of pneumonia; need for tracheostomy; pain control; lung volumes on spirometry; quality of life after discharge; exercise tolerance; chronic disability; and time away from work) were voted on independently by each author on a scale from 1 to 9 per the GRADE methodology.[13] Outcomes with scores 7 to 9 were considered critical, those with scores 4 to 6 were considered important, and those with scores in the 1 to 3 range were considered of limited importance. After rounding to the nearest integer, outcomes with an average score of 7 or greater (considered to be critical) were included in our PICO questions. The intervention, rib ORIF, was compared against nonoperative management, as described earlier. Finally, patients were grouped into those with flail chest as defined by each reviewed manuscript although classically defined as those with three or more consecutive ribs fractured at 2 or more sites each, and those without flail chest pattern. The rounded average scores for each of the considered clinically relevant outcomes are summarized on Table 1.
Methods
Data Extraction and Methodology
Data extraction from each study was performed using standardized data collection sheets and was performed in duplicate (G.K., N.P., E.A.H., E.S.). Data extracted included authors; journal; publication year; country of origin; study design; whether patients with traumatic brain injury were excluded; patients' age, sex, and Injury Severity Scores; number of patients in the operative and nonoperative arms; number of patients with flail and nonflail chest rib fracture patterns (if available); time from admission to operation (if available), and the critical outcomes previously outlined (including mean and standard deviation [SD] values for the continuous outcomes). Whenever only mean and p values were provided and no SDs for the continuous variables, the latter were calculated using the following formula: Standard Deviation (SD) = [(Mean Difference/t-Score)] / Square Root of (1 / N1 + 1 / N2), where the t-score was calculated for each outcome using the provided p value and each study's degrees of freedom. N1 and N2 represent the number of patients in the ORIF and nonoperative groups, respectively. If no p value was provided but statistical significance was declared, the highest p value of the alpha error declared by the authors was used for the SD calculations (e.g., if statistical significance was declared at a two-tailed level of less than 0.05 and no exact p value was provided, it was assumed that the p value was 0.05). When a range was provided and no SD, the latter was calculated by subtracting the minimum from the maximum value and dividing by 4.[14] Forest plots were generated and treatment effects calculated, with each study weighing proportionally to the number of subjects it contributed in each outcome analysis. Heterogeneity for the analysis of each outcome was calculated using χ[2] (Cochran Q statistic) and quantified with I[2]. I[2] values less than 25% were considered to provide a low degree of heterogeneity; I[2]values in the 25% to 50% range moderately heterogeneous, and values greater than 50% were indicative of high heterogeneity.[15]
Publication bias was evaluated using the Egger test,[16][17] and the GRADE framework was applied to all quantified outcomes for assessment of bias, publication bias, inconsistency, imprecision, and indirectness. Analyses were performed with STATA version 13.1 (Stata, College Station, TX), and all recommendations and their reported strengths were reviewed and agreed on by the entire authoring team. GRADEproGDT (Cochrane Informatics & Knowledge Management, Baltimore, MD) was used to generate evidence profile tables.
Results
Results for PICO Question 1 (RIB ORIF in Trauma Patients with Flail Chest)
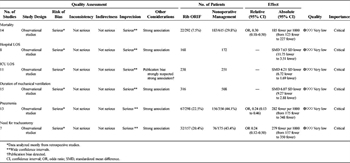
TABLE 2. GRADE Evidence Table for PICO 1: Rib ORIF Compared to Nonoperative Management for Flail Chest After Blunt Trauma
Qualitative Synthesis
Although a wide variety of surgical techniques for operative management of flail chest were described, ranging from struts and wires[18][19] to plates in the most recent studies, small numbers of patients treated with each method precluded us from assessing for differences across different techniques, and all patients undergoing operative management were pooled together. The same was true for nonoperatively managed patients, in whom intubation and tracheostomy thresholds, ventilation and weaning strategies, pain control, fluid administration, bronchodilator and pulmonary toilet regimens varied across studies. Despite the variability in both surgical technique and conservative management options, surgical rib stabilization demonstrated fairly consistent results across studies conducted in a variety of settings, regarding DMV, ICU LOS and hospital LOS, incidence of pneumonia, and need for tracheostomy. The effect on mortality was more pronounced in studies conducted before 2000,[18][20][21] before recent advances in critical care and invasive ventilation were widespread. Only one study[22] assessed pain control in patients with flail chest and found it to be improved with rib ORIF; however, the sample size was too small to elicit any meaningful inferences (n = 37) and thus was eliminated from the evidence table (Table 2).
While most subjects in our analysis were identified through retrospective chart reviews,[18][20][21][23–32] there were also three prospective randomized trials. Tanaka et al.[22] (n = 37; 18 patients underwent rib ORIF and 19 nonoperative management) conducted the first prospective randomized clinical trial including adult blunt trauma victims with severe flail chest on mechanical ventilation, unable to wean by postinjury Day 5. Patients with fewer than six fractured ribs; those with severe closed head injury (head AIS > 3) and/or spinal injury; with chronic preexisting heart, pulmonary, hepatic, and/or renal disease were excluded. Rib fixation afforded shorter DMV and ICU LOS, lower incidence of pneumonia and need for tracheostomy, and improved pain and subjective shortness of breath, all while hastening functional recovery. This study also demonstrated that these outcomes could be achieved with lower costs. Granetzny et al.[33] prospectively randomized 40 flail chest patients to rib ORIF (n = 20) versus conservative management (n = 20). Patients with head injury leading to altered mental status; myocardial contusion or other injuries that could be adversely affected by general anesthesia; severe multiorgan trauma; and injury of only the top three ribs were excluded. The group demonstrated reduced DMV, ICU LOS and hospital LOS, as well as lower incidence of pneumonia and chest wall deformity. Spirometry was also noted to be improved 2 months after injury. Most recently, Marasco et al.[34]randomized 46 flail chest victims, if they were ventilator dependent with no prospect of successful weaning within the next 48 hours. Subjects older than 80 years, severe traumatic brain injury (Glasgow Coma Scale < 10), spinal injuries precluding lateral decubitus positioning, and open rib fractures with soiling or infection were excluded. Patients undergoing rib fixation (n = 23) benefitted from shorter DMV and ICU LOS, as well as decreased need for postoperative noninvasive ventilation. These outcomes also accompanied significant cost savings, although no differences were noted in quality of life, spirometric findings, or activity levels at later follow-ups. Two of the prospective randomized trials[22][34] surgically stabilized only Ribs 3 to 10 per the corresponding trials protocols, as Ribs 1 to 2 and 11 to 12 were not considered to contribute much to chest wall stability and pulmonary mechanics, while adding significant surgical morbidity due to technically challenging access.
Patients with moderate to severe traumatic brain injury were commonly excluded,[22][23][26][27][30][32–34] as these patients can easily confound the commonly assessed outcome measures, as their brain trauma may drive up pneumonia incidence and need for tracheostomy (in the face of altered mental status and inadequate secretion clearance), and require longer DMV, ICU LOS, and hospital LOS. Brain injury itself is also associated with higher mortality rates, and afflicted subjects may not derive the full benefit of rib ORIF owing to extrapulmonary reasons. Conversely, severe brain trauma victims may not be able to lie flat for lengthy chest operations in the presence of intracranial hypertension, and the risk-to-benefit ratio of chest wall reconstruction has to be carefully evaluated on an individual basis.
Two investigators attempted to shed light on the effect of rib ORIF for flail chest after blunt trauma in patients with significant underlying pulmonary contusions.[29][31] Zhang et al only demonstrated shorter hospital LOS in surgically managed patients with flail chest and clinically significant pulmonary contusions (38 vs 60 days, p = 0.049).[31] Voggenreiter et al.[29] studied 42 patients with flail chest with or without significant underlying pulmonary contusion. His team demonstrated shorter DMV only in patients without pulmonary contusion, suggesting that in patients with contused lungs, rib ORIF may not improve outcomes, despite restoration of chest wall mechanics.
Regarding the optimal timing of rib ORIF, it seems that patients enrolled in studies that offered surgery early (within 24–72 h after injury)[18][20][23][26–28][32][33] enjoyed shorter DMV, ICU LOS, and hospital LOS, as well as lower incidence of pneumonia and need for tracheostomy, compared to those that were operated on later on (72 hours after injury).[22][30][34] This suggests that patients with flail chest after blunt trauma who are deemed appropriate surgical candidates should be operatively managed early, as soon as resuscitation is complete and other potentially life-threatening injuries have been addressed.
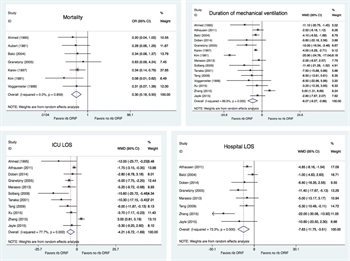
Figure 2. Forest plots for mortality, DMV, ICU LOS, and hospital LOS, respectively.
Quantitative Synthesis (Meta-analysis)
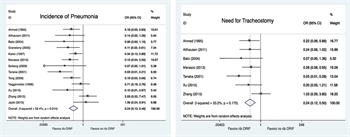
Figure 3. Forest plots for incidence of pneumonia and need for tracheostomy.
A total of 986 subjects with flail chest after blunt trauma, 334 of whom underwent surgical rib fixation, were included in our analysis for PICO Question 1. The average age and Injury Severity Score for the rib ORIF patients were 44.5 ± 6.7 versus 45.7 ± 8.1 and 29.8 ± 6.2 versus 30 ± 6.4, respectively. Comparisons between rib ORIF and nonoperative management on the aforementioned outcome variables are summarized in the forest plots displayed in Figures 2–3. Analysis of the pooled data demonstrated improved mortality (odds ratio [OR], 0.3 [95% confidence interval {CI}, 0.18–0.50; p < 0.001]), DMV (weighted mean difference [WMD], −6.07 [95% CI, −9.27 to −2.89; p < 0.001]), ICU (WMD −4.21 [95% CI, −6.72 to −1.69; p = 0.001]), and hospital LOS (WMD, −7.63 [95% CI, −11.75 to −3.51; p < 0.001]), as well as decreases in the incidence of pneumonia (OR, 0.24 [95% CI, 0.13–0.46; p < 0.001]) and need for tracheostomy (OR, 0.24 [95% CI, 0.12–0.50; p < 0.001]) in the surgically managed victims with flail chest. Heterogeneity was minimal in the analysis of mortality (I[2] = 0%), moderate with regard to need for tracheostomy (I[2] = 33.2%, likely due to variability in time from injury to intervention and threshold and timing of tracheostomy), and high in the analysis of DMV (I[2] = 86.9%), ICU (I[2] = 77.7%), and hospital LOS (I[2] = 73.3%) as well as pneumonia (I[2] = 52.4%, likely due to variability in time from injury to intervention and heterogeneity in pneumonia definition). The GRADE assessment of studies available for PICO Question 1 is summarized on Table 2. Quantitative analysis for pain control with or without rib ORIF was not possible given the paucity of data for this critical outcome.
Results for PICO Question 2 (RIB ORIF in Trauma Patients with Nonflail Rib Fractures)
Qualitative Synthesis
Qualitative synthesis in patients with nonflail chest patients was not feasible, as no studies included only patients with nonflail rib fractures. Among studies that included both flail and nonflail rib fracture patterns, no subanalyses were performed and no breakdown of the two distinct patient cohorts and their corresponding outcomes was provided.
Two notable studies were those conducted by Khandelwahl et al.[35] and Pieracci et al.,[36] respectively. The former assessed pain scores in patients with any rib fracture pattern prospectively, and subjects with scores greater than 5 were enrolled. These subjects were managed with an aggressive pain regimen and pulmonary toilet and were offered surgical rib stabilization only if by the 11th postinjury day their pain scores were greater than 7. Although significant selection bias may exist, patients who underwent rib ORIF had improved pain scores postoperatively and were able to return earlier to baseline activity. Most recently, Pieracci et al.[36] conducted a crossover analysis of patients with flail chest, multiple displaced fractures, intractable pain, or inability to wean off ventilation. After adjusting for rib fracture and overall injury severity, as well as the presence of intracranial injury, they demonstrated shorter DMV and decreased need for tracheostomy, although narcotic requirement was not dissimilar between the two groups.
Majercic et al.[37] retrospectively reviewed all their institution's patients with rib fracture: Surgery was offered to those with flail chest, severe rib dislocation, intractable pain, and/or inability to wean from mechanical ventilation, per their protocol. Intensive care unit LOS was shorter in patients with rib ORIF; and in the subset of trauma victims with no brain injury, DMV was shorter and need for tracheostomy was less. Wu et al.[38] studied patients with flail chest and multiple or displaced rib fractures: In this study, patients self-selected operative or conservative management. Those who underwent surgery had shorter DMV, ICU LOS, and hospital LOS; and their incidence of pulmonary infections, mortality, and need for tracheostomy was lower compared to their nonoperative counterparts. Pain control was also improved in the rib ORIF group. De Moya et al.[39] studied pain control in subjects with any fracture type and demonstrated that although there was no difference in analgesic requirements between the rib ORIF and nonoperatively managed patients, narcotics were administered less frequently in the surgically stabilized cohort, likely the result of selection bias. However, patients that underwent rib ORIF required less narcotics postoperatively compared to preoperatively.
Of the outcomes noted to have improved (mortality;[38] DMV;[36][38][40] ICU LOS[37][38] and hospital LOS;[38]incidence of pneumonia[38] and need for tracheostomy;[36][38] and pain[38]), it is unclear whether the effect size is due to the improved outcomes in the significant proportion of the included patients with flail chest, or an overall effect of rib ORIF in any patient receiving it.
Quantitative Synthesis (Meta-analysis)
No studies were identified that explicitly enrolled only patients with nonflail rib fractures. All published data evaluated for PICO Question 2 included patients with “any rib fracture pattern,” and most encompassed a significant proportion of flail chest victims. Therefore, a meta-analysis is not possible for PICO Question 2.
Grading the Evidence
Applying the GRADE framework to the outcomes quantitatively studied (mortality, pneumonia incidence and need for tracheostomy, DMV, hospital LOS, and ICU LOS) in patients with flail chest after blunt injury, risk of bias was considered serious, given most subjects were contributed from retrospective chart reviews. There was also concern about imprecision, given the wide confidence intervals, and the high heterogeneity noted in most outcomes studied. No major issues were detected in inconsistency and indirectness, and publication bias may have been present for the ICU LOS. The overall quality of evidence was deemed very low. Given the improvement in all outcomes (in which adequate data were available for analysis) and the consistent and sizeable treatment effect of rib ORIF in patients with flail chest after blunt trauma, the authors voted to conditionally recommend the intervention in this patient population. Consideration to upgrade this recommendation from conditional to strong was given; however, the authors voted to maintain a conditional recommendation (6–4 votes; typically 70% of votes are required for a strong recommendation[41]). This recommendation implies that rib ORIF should be offered to most trauma victims with flail chest after blunt trauma to benefit from the aforementioned improved outcomes, including lower mortality; shorter DMV, hospital LOS, and ICU LOS; and lower incidence of pneumonia and need for tracheostomy. However, consideration should be given to patients' personal preferences, resource availability, the burden of associated injuries, and the overall treatment plan and prognosis for quality of life. Regarding pain control in flail chest subjects, inconsistency and publication bias are difficult to assess given the small number of studies identified, and the variability of methods for pain control used may include significant bias. Multicenter studies currently underway are likely to shed additional light to the use of rib ORIF in the future.
Regarding the outcomes in patients with nonflail chest fractures, neither a qualitative nor a quantitative analysis can be performed, as none of the studies reviewed allows identification of the patients with purely nonflail chest; and the risk of selection bias, imprecision, and indirectness is very high.
Recommendations

TABLE 3. Summary of Recommendations
Based on the aforementioned analyses, in adult patients with flail chest after blunt trauma, we conditionally recommend operative rib ORIF compared to nonoperative management, to decrease mortality; shorten DMV, ICU LOS, and hospital LOS; incidence of pneumonia, and need for tracheostomy. This level of recommendation is given based on the low quality of evidence. We cannot offer a recommendation for pain control with currently available evidence.
In adult patients with nonflail pattern rib fractures, we cannot offer a recommendation regarding rib ORIF, compared to conservative management, to decrease mortality; DMV, ICU LOS, and hospital LOS; incidence of pneumonia and need for tracheostomy; and improve pain control, with currently available evidence.
Our recommendations are summarized in Table 3.
Authorship
G.K. conceived and designed the study, analyzed the data, and drafted the manuscript. G.K. and M.B.P. reviewed the literature. G.K., E.A.H., E.S., N.P., M.B.P., L.A., P.B., J.L., E.H., and J.C. graded the outcomes. G.K., N.P., E.A.H., and E.S. performed the data extraction. G.K., E.A.H., E.S., N.P., M.B.P., L.A., P.B., J.L., E.H., and J.C. graded and reviewed the evidence. J.C. and E.H. oversaw the study.
Acknowledgement
The authors thank David Flynn at Boston University's School of Medicine Library and Carol Ann Mita at Harvard University's Countway Library of Medicine. Without their expertise and guidance, this project would not have been feasible.
Disclosure
Conflicts of Interest: GK is the recipient of the NIH-NIGMS grant “Targeted polymerized shell microbubbles to image surgical adhesions” (R41GM116530) as coinvestigator and NIH-NCATS grant “Predicting and Preventing Re-Admissions Within 30 days after Surgery” (1UL1TR001430-01) as co–primary investigator. He is also the recipient of Boston University's Faculty Research Scholarship fund “Histone Acetylation in Acute Lung Injury” as primary investigator and receives royalties for developing surgical training modules from McGraw-Hill Medical. He is also the paid author of a textbook chapter commissioned by Wolters-Kluwer Health for “Greenfield's Surgery: Scientific Principles and Practice, 6th Edition” entitled “Surgical Nutrition,” and the paid author of a textbook chapter commissioned by Elsevier for ‘”Advances in Surgery, 2015 Edition” entitled ”Trainee Participation in Emergency Surgery: What Are the Consequences?” EAH is a paid consultant for DePuy Synthes Trauma. He receives research grants support as well as a grant for a research fellow from DePuy Synthes Trauma. He is also a paid lecturer and faculty for AO North America Trauma. MBP is supported by the Vanderbilt Faculty Research Scholars Program and NIH (HL111111). EH is the primary investigator of a grant (1R01HS024547-01) from the Agency for Healthcare Research and Quality (AHRQ) titled “Individualized Performance Feedback on Venous Thromboembolism Prevention Practice” and a contract (CE-12-11-4489) with The Patient-Centered Outcomes Research Institute (PCORI) titled “Preventing Venous Thromboembolism: Empowering Patients and Enabling Patient-Centered Care via Health Information Technology.” He receives royalties from Lippincott Williams & Wilkins for the book Avoiding Common ICU Errors and is a paid consultant and speaker for the “Preventing Avoidable Venous Thromboembolism—Every Patient, Every Time” VHA/Vizient IMPERATIV® Advantage Performance Improvement Collaborative and the Illinois Surgical Quality Improvement Collaborative “ISQIC.” He was the paid author of a paper commissioned by the National Academies of Medicine titled “Military Trauma Care's Learning Health System: The Importance of Data Driven Decision Making,” which was used to support the report titled “A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury.”
Source of Funding: Not applicable.
References
- Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975–979.
- Vana PG, Neubauer DC, Luchette FA. Contemporary management of flail chest. Am Surg. 2014;80:527–535.
- Chapman BC, Herbert B, Rodil M, et al. RibScore: a novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg. 2016;80:95–101.
- Lin FC, Li RY, Tung YW, Jeng KC, Tsai SC. Morbidity, mortality, associated injuries, and management of traumatic rib fractures. J Chin Med Assoc. 2016;79:329–334.
- Cannon RM, Smith JW, Franklin GA, Harbrecht BG, Miller FB, Richardson JD. Flail chest injury: are we making any progress? Am Surg. 2012;78:398–402.
- Leinicke JA, Elmore L, Freeman BD, Colditz GA. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013;258:914–921.
- Britt T, Sturm R, Ricardi R, Labond V. Comparative evaluation of continuous intercostal nerve block or epidural analgesia on the rate of respiratory complications, intensive care unit, and hospital stay following traumatic rib fractures: a retrospective review. Local Reg Anesth. 2015;8:79–84.
- Duch P, Moller MH. Epidural analgesia in patients with traumatic rib fractures: a systematic review of randomised controlled trials. Acta Anaesthesiol Scand. 2015;59:698–709.
- Richardson JD, Adams L, Flint LM. Selective management of flail chest and pulmonary contusion. Ann Surg. 1982;196:481–487.
- Zaw AA, Murry J, Hoang D, Chen K, Louy C, Bloom MB, Melo N, Alban RF, Margulies DR, Ley EJ. Epidural analgesia after rib fractures. Am Surg. 2015;81:950–954.
- Coleman FP, Coleman CL. Fracture of ribs; a logical treatment. Surg Gynecol Obstet. 1950;90:129–134, illust.
- Proctor H, London PS. The stove-in chest with paradoxical respiration. Br J Surg. 1955;42:622–633.
- Kerwin AJ, Haut ER, Burns JB, et al. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73:S283–S287.
- Egger M, Smith G, Altman D. Systematic Reviews in Health Care: Meta-Analysis in Context. London, UK: BMJ Books; 2011.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558.
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634.
- Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–105.
- Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg. 1995;110:1676–1680.
- Khan IA, Ghaffar S, Asif S, Zia-ur-Rehman, Asad S, Ahmed E, Ahmed W, Asif Z. Management of thoracic trauma: experience at Ayub Teaching Hospital, Abbottabad. J Ayub Med Coll Abbottabad. 2009;21:152–154.
- Karev DV. Operative management of the flail chest Wiadomosci Lekarskie (Warsaw, Poland (1960): 1997;50: (Suppl 1, Pt 2):205–208.
- Kim M, Brutus P, Christides C, et al. [Compared results of flail chests treatments: standard internal pneumatic stabilization, new technics of assisted ventilation, osteosynthesis (author's translation)]. J Chir (Paris). 1981;118:499–503.
- Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–732; discussion 32.
- Althausen PL, Shannon S, Watts C, Thomas K, Bain MA, Coll D, O'mara TJ, Bray TJ. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma. 2011;25:641–647.
- Aubert M, Antoine P, Pilichowski P, Contamin C, Peyrin JC, Jacquot C, Carpentier F, Roche C. [Flail chests. Study of 224 cases (author's translation)]. Ann Chir. 1981;35:33–39.
- Balci AE, Eren S, Cakir O, Eren MN. Open fixation in flail chest: review of 64 patients. Asian Cardiovasc Thorac Ann. 2004;12:11–15.
- Doben AR, Eriksson EA, Denlinger CE, Leon SM, Couillard DJ, Fakhry SM, Minshall CT. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care. 2014;29:139–143.
- Solberg BD, Moon CN, Nissim AA, Wilson MT, Margulies DR. Treatment of chest wall implosion injuries without thoracotomy: technique and clinical outcomes. J Trauma. 2009;67:8–13; discussion.
- Teng J, Cheng Y, Ni D, et al. Outcomes of traumatic flail chest treated by operative fixation versus conservative approach. Journal of Shanghai Jiaotong University. 2009;29:1495–1498.
- Voggenreiter G, Neudeck F, Aufmkolk M, Obertacke U, Schmit-Neuerburg KP. Operative chest wall stabilization in flail chest—outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998;187:130–138.
- Xu JQ, Qiu PL, Yu RG, Gong SR, Ye Y, Shang XL. Better short-term efficacy of treating severe flail chest with internal fixation surgery compared with conservative treatments. Eur J Med Res. 2015;20:55.
- Zhang Y, Tang X, Xie H, Wang RL. Comparison of surgical fixation and nonsurgical management of flail chest and pulmonary contusion. Am J Emerg Med. 2015;33:937–940.
- Jayle CP, Allain G, Ingrand P, Laksiri L, Bonnin E, Hajj-Chahine J, Mimoz O, Corbi P. Flail chest in polytraumatized patients: surgical fixation using Stracos reduces ventilator time and hospital stay. Biomed Res Int. 2015;2015:624723.
- Granetzny A, Abd El-Aal MA, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4(6):583–587.
- Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216(5):924–932.
- Khandelwal G, Mathur RK, Shukla S, Maheshwari A. A prospective single center study to assess the impact of surgical stabilization in patients with rib fracture. Int J Surg. 2011;9:478–481.
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2016;80:187–194.
- Majercik S, Wilson E, Gardner S, Granger S, VanBoerum DH, White TW. In-hospital outcomes and costs of surgical stabilization versus nonoperative management of severe rib fractures. J Trauma Acute Care Surg. 2015;79:533–538; discussion 8–9.
- Wu WM, Yang Y, Gao ZL, Zhao TC, He WW. Which is better to multiple rib fractures, surgical treatment or conservative treatment? Int J Clin Exp Med. 2015;8(5):7930–7936.
- de Moya M, Bramos T, Agarwal S, Fikry K, Janjua S, King DR, Alam HB, Velmahos GC, Burke P, Tobler W. Pain as an indication for rib fixation: a bi-institutional pilot study. J Trauma. 2011;71:1750–1754.
- Nirula R, Allen B, Layman R, Falimirski ME, Somberg LB. Rib fracture stabilization in patients sustaining blunt chest injury. Am Surg. 2006;72:307–309.
- Jaeschke R, Guyatt GH, Dellinger P, Schünemann H, Levy MM, Kunz R, Norris S, Bion J; GRADE Working Group. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008;337:a744.