Thoracic Trauma, Blunt, Pain Management of
Replaces: Blunt Thoracic Trauma (BTT), Pain Management in
Published 2016
Citation: J Trauma. 81(5):936-951, November 2016
Authors
Galvagno, Samuel Michael Jr DO, PhD; Smith, Charles E. MD; Varon, Albert J. MD, MHPE; Hasenboehler, Erik A. MD; Sultan, Shahnaz MD, MHSc; Shaefer, Gregory DO; To, Kathleen B. MD; Fox, Adam D. DO, DPM; Alley, Darrell E.R. MD; Ditillo, Michael DO; Joseph, Bellal A. MD; Robinson, Bryce R.H. MD, MS; Haut, Elliott R. MD, PhD
Author Information
From the Department of Anesthesiology, University of Maryland School of Medicine and Program in Trauma, R Adams Cowley Shock Trauma Center, Baltimore, Maryland (S.M.G.); Case Western Reserve University School of Medicine, and Cardiothoracic and Trauma Anesthesia, Department of Anesthesiology, MetroHealth Medical Center, Cleveland, Ohio (C.E.S.); Department of Anesthesiology, University of Miami Miller School of Medicine, and Ryder Trauma Center at Jackson Memorial Hospital, Miami, Florida (A.J.V.); Department of Orthopedic Surgery, Adult and Trauma Service, Johns Hopkins Hospital and Johns Hopkins Bayview Medical Center, Baltimore, Maryland (E.A.H.); Division of Gastroenterology, Hepatology, and Nutrition, Department of Medicine, and Center for Chronic Diseases Outcomes Research, Minneapolis Veterans Affairs Health System, Minnesota (S.S.); Division of Trauma, Critical Care, and Acute Care Surgery, Department of Surgery, West Virginia University, Morgantown, West Virginia (G.S.); Division of Acute Care Surgery (Trauma, Burn, Critical Care, Emergency Surgery), Department of Surgery, University of Michigan, Ann Arbor, Michigan (K.B.T.); Division of Trauma Surgery and Critical Care, Department of Surgery, Rutgers University–New Jersey School of Medicine, Newark, New Jersey (A.F.); East Texas Medical Center, Tyler, Texas (D.E.R.A.); Allegheny General Hospital, Pittsburg, Pennsylvania (M.D.); Division of Trauma, Critical Care, & Emergency Surgery, The University of Arizona College of Medicine, Arizona (B.A.J.); Department of Surgery, Harborview Medical Center, University of Washington, Seattle, Washington (B.R.H.R.); and Division of Acute Care Surgery, Department of Surgery, Johns Hopkins Hospital, Baltimore, Maryland (E.R.H.).
Submitted: March 19, 2016, Revised: May 10, 2016, Accepted: May 11, 2016, Published online: August 16, 2016.
B.R.H.R. and E.R.H. are co–senior authors.
Preliminary data from this article were presented as a podium talk/status update during the Practice Management Guideline meeting at the Eastern Association for the Surgery of Trauma in 2015, Orlando, Florida.
Address for reprints: Samuel Michael Galvagno, Jr, DO, PhD, Divisions of Critical Care Medicine and Trauma Anesthesiology, Department of Anesthesiology, 22 South Greene St, T3N08, Shock Trauma Center, Baltimore, MD 21201; email: sgalvagno@anes.umm.edu.
Overview
Thoracic trauma is the second most prevalent nonintentional injury in the United States and is associated with significant morbidity.[1–3] In particular, rib fractures occur in up to 10% of hospitalized trauma patients and may be associated with a mortality of 3% to 13%.[1][4][5] Injuries caused by blunt thoracic trauma are frequently associated with pulmonary complications such as pneumonia and severe pain, prolonging both hospital and intensive care unit (ICU) stay and significantly increasing healthcare costs, especially in elderly patients.[6][7] Pain is acknowledged as a contributing element for much of the morbidity associated with blunt thoracic trauma,[2][5][8] and optimization of analgesia is an essential component of a strategy that uses early mobilization and chest physiotherapy to enhance recovery.
In 2005, the Eastern Association for the Surgery of Trauma (EAST) published a pain management guideline for blunt thoracic trauma.[9] The authors of this review recognized the paucity of literature regarding the effectiveness of various analgesic modalities, and recommendations at the time reflected the most reasonable and likely approach to ensure positive outcomes.[9] While several modalities were reviewed, the authors concluded that epidural analgesia is the preferred technique. This recommendation was challenged by Carrier et al.[8] in a 2009 systematic review and meta-analysis and more recently by Duch and Møller.[10] In adults with blunt thoracic trauma, the ideal analgesic modality remains uncertain.
A variety of analgesic techniques are available for the treatment of pain after thoracic trauma. Epidural analgesia is the best-studied modality in both thoracic trauma and elective thoracotomies and involves the administration of opioid and/or local anesthetic agents into the epidural space at the thoracic or lumbar level. Pain relief is often pronounced, but this technique is contraindicated in patients with coagulopathy, associated with potentially troublesome adverse effects such as hypotension, and is technically demanding. Moreover, historical concerns about epidural analgesia include loss of lower-extremity sensation, a requirement for bladder catheterization, and venous pooling, which might precipitate deep venous thrombosis.[11]
Thoracic paravertebral blockade produces unilateral segmental somatic and sympathetic nerve blockade. In thoracic paravertebral blockade, in the paravertebral space, which contains spinal nerves and preganglionic and postganglionic sympathetic nerves, local anesthetics are injected as a single-shot procedure or with placement of a catheter for a continuous block.[12] Thoracic paravertebral blocks are technically easier to perform than epidural analgesia, require less nursing surveillance, and have fewer absolute contraindications.[13] The use of thoracic paravertebral blocks in patients with blunt thoracic trauma is not as well studied as epidural analgesia, and the effectiveness of this technique has not been subjected to the scrutiny of large clinical trials. However, with the proliferation of ultrasound, thoracic paravertebral blockade may become a desirable technique.
Intrapleural analgesia (sometimes also referred to in the literature as “interpleural” analgesia) involves placement of a local anesthetic agent into the pleural space.[9][14] The anesthetic agent traverses the parietal pleura and blocks multiple unilateral dermatomes. This technique preserves lower-extremity sensation, does not cause hypotension, and does not require bladder catheterization. Disadvantages of this technique include loss of anesthetic via draining chest tubes, impaired absorption of agent in the presence of a hemothorax, higher risk of local anesthetic systemic toxicity, and unknown overall effectiveness in patients with blunt thoracic trauma. Intercostal nerve blocks include single or continuous injections of local anesthetics into the posterior component of the intercostal space. This technique has been shown to improve pain scores and compliance with pulmonary toilet,[15] but overall effectiveness in patients with blunt thoracic trauma has not been rigorously analyzed. Finally, a multimodal analgesic strategy that incorporates different regional techniques, systemic analgesics, and analgesic adjuncts (e.g., intravenous acetaminophen, nonsteroidal anti-inflammatory agents [NSAIDs], transdermal opioids) may improve management of pain related to blunt thoracic trauma.
The goal of this article, which was sponsored by the EAST and cosponsored by the Trauma Anesthesiology Society, is to provide updated evidence-based recommendations that may be used to direct the decision-making processes related to the care of patients with blunt thoracic trauma. This guideline has been developed using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework adopted by EAST.[16–18]
The GRADE framework, now in use by more than 90 international societies and organizations worldwide, provides a systematic and transparent framework for clarifying questions, determining the outcomes of interest, summarizing the evidence for such questions, and moving from evidence to a recommendation or decision. Importantly, within GRADE, the evidence is rated not according to each individual study, but across studies for specific patient-important clinical outcomes. Recommendation strength and direction are based not only on evidence quality but also on the balance between desirable and undesirable outcomes and patient values and preference.[18]
Objectives
The objective of this guideline is to evaluate the optimal mode of analgesia for patients with blunt thoracic trauma. The PICO questions[18] (population [P], intervention [I], comparator [C], and outcome [O]) are defined as follows:
- PICO Question 1: In adult patients with blunt thoracic trauma (P), does epidural analgesia (I) versus nonregional modalities of pain control (C) (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
- PICO Question 2: In adult patients with blunt thoracic trauma (P), does paravertebral blockade (I) versus nonregional modalities of pain control (C) (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
- PICO Question 3: In adult patients with blunt thoracic trauma (P), does continuous intrapleural infusions of local anesthetics (I) versus other regional modalities of pain control (C) (i.e., epidural or paravertebral nerve blocks) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
- PICO Question 4: In adult patients with blunt thoracic trauma (P), does multimodal analgesia (I) (i.e., use of different classes of analgesics, including combinations of opioids with other agents such as NSAIDs, pregabalin/gabapentin, acetaminophen) compared with opioids alone (C) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
- PICO Question 5: In adult patients with blunt thoracic trauma (P), does continuous intercostal infusions of local anesthetics (I) versus nonregional modalities of pain control (C) (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
Inclusion Criteria for this Review
Study Types
We included randomized controlled trials (RCTs), case-control studies, and prospective or retrospective observational cohort studies (with a comparator group). Reviews containing no original data or comments were excluded.
Participant Types (Population, P)
Only studies pertaining to the treatment of hospitalized patients with blunt thoracic trauma were included. Blunt thoracic trauma was defined as chest wall injuries such as rib fracture, flail chest, sternal fracture, and soft tissue contusion; intrapleural lesions such as hemothorax and pneumothorax; parenchymal lung injuries such as pulmonary contusion and lung laceration; and mediastinal lesions such as blunt cardiac injury or great vessel injury.[9] We included studies of adult patients (>16 years of age) without restricting gender, ethnicity, or degree of comorbidity.
Intervention Type (I)
We included studies in which regional anesthetic techniques, such as epidural or paravertebral catheters, intercostal nerve blocks, multimodal approaches (i.e., opioids plus pregabalin/gabapentin, or other nonregional drug combinations), or intrapleural infusions of anesthetics, were used compared with nonregional techniques such as use of intravenous or enteral analgesics (i.e., opioids, acetaminophen, NSAIDs).
Outcome Measure Types (O)
Outcomes were chosen by group consensus as recommended by the GRADE approach.[16] Outcomes were chosen by the committee and rated in importance from 1 to 9, with scores of 7 to 9 representing critical outcomes and scores of 4 to 6 representing important outcomes. Critical outcomes for all five PICO questions included analgesia (as measured by a validated pain scale such as the visual analog scale), postoperative pulmonary complications (PPCs), and pulmonary function as evidenced by objective measures, requirement for intubation, and mortality. Important outcomes included hospital or ICU length of stay. Additional outcomes considered by the committee were cost, ventilator days, and labor-intensiveness.
Review Methods
Search Strategy
A systematic search of the , EMBASE, CINAHL, MEDLINE (OVID), and The Cochrane Register of Controlled Trials electronic databases was performed by the primary author (S.M.G.) for studies published from January 1967 to October 2015. A systematic search of the National Institutes of Health MEDLINE database was performed using . Search terms included the following: Epidural Analgesia [MeSH], thoracic epidural analgesia, thoracic epidural, blunt thoracic trauma, Thoracic Injuries [majr], pneumothorax, hemothorax, rib fracture(s), sternal fracture, chest contusion, Randomized Controlled Trial [Publication Type], Cohort Studies [MeSH], Case-control Studies [majr], Mortality {Mesh], Hospital Mortality [MeSH], reintubation, pneumonia [MeSH], Pulmonary Atelectasis [majr], Respiratory Function Tests [MeSH], Analgesia [MeSH], Analgesia, Patient-controlled [MeSH], Pain Measurement [MeSH], Length of Stay [MeSH], postoperative pulmonary contusions. A similar systematic search of the EMBASE database was performed using the following search terms (including Emtree mapping terms): epidural anesthesia, thorax blunt trauma, blunt AND thoracic AND trauma, pneumothorax, hemothorax, lung AND contusion, pulmonary AND contusion, flail chest, chest AND contusion, thoracic AND epidural AND analgesia, epidural OR regional AND anesthesia, postoperative complications, reintubation, randomized controlled trial, cohort analysis, case control study. For PICO Questions 2 to 5, the searches were adjusted accordingly, using terms for the analgesic intervention of interest (i.e., “epidural analgesia” was replaced with “paravertebral block,” etc.). The methodology for the MEDLINE and EMBASE searches was used to conduct searches in The Cochrane Register of Controlled Trials and CINAHL. Non-English articles, when included, were reviewed by multilingual members of the research team (S.M.G., A.J.V., C.E.S.). In addition to the electronic search, we manually searched the bibliographies of included studies and recent review articles.
Assessment of the Quality of Evidence
The quality of the evidence for each outcome in a PICO was evaluated using the GRADE framework.[16][17] While RCTs were considered high-quality evidence, we rated down for quality if there were concerns that lowered our certainty in the estimate of effect for that outcome. We evaluated for risk of bias, inconsistency (also referred to at heterogeneity), indirectness, imprecision, and other considerations (e.g., publication bias). Observational studies, by default, were considered low-quality evidence, but could be rated up under the following circumstances: large effect, dose-response gradient, or if all possible confounders would decrease an effect or move the effect in the opposite direction.
Risk-of-Bias Assessment
Risk of bias was assessed for each outcome using the instrument developed by the Cochrane Collaboration[19] and the Jadad Scale.[20] The Cochrane instrument includes the domains of random sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and baseline imbalance and bias due to vested financial interest.[19] The Jadad score, which assesses randomization, blinding, and patient withdrawals/dropouts, was used to grade included studies with a score between 0 and 5.[20] For nonrandomized studies, the Downs and Black assessment tool was used.[21] This instrument includes assessment items for reporting bias, external validity, internal validity, confounding, and selection bias.[21] For both the Cochrane and Downs and Black assessment tools, if one or more domains were judged as being high or unclear, we classified the trial as having a high risk of bias. Systematic reviews were assessed with the AMSTAR instrument, a tool designed to assess the methodological quality of systematic reviews.[22]
Statistical Analyses
When a quantitative analysis was indicated, we calculated relative risk with 95% confidence intervals (CIs) for dichotomous outcome measures and the mean difference (MD) with 95% CI for continuous outcome measures using the Mantel-Haenszel random-effects model.[19] These measures were pooled in conventional cumulative meta-analyses for each critical and important outcome included in this recommendation. Heterogeneity, or inconsistency, was assessed using the I[2] statistic (inconsistency factor).[23] An I[2] value more than 50% was suggestive of moderate heterogeneity, and a value greater than 75% indicated substantial heterogeneity due to real differences in protocols, trial populations, interventions, and/or outcomes.[23] The meta-analysis was performed using the Cochrane Collaboration’s “Revman” software (version 5.3; Cochrane Collaboration, Oxford, UK). Evidence tables were created using the GRADE Working Group’s open access Guideline Development Tool (May 25, 2015, update; Evidence Prime, Inc., Hamilton, Ontario, Canada). All tests were two-tailed, and p < 0.05 was considered statistically significant.
Search Results
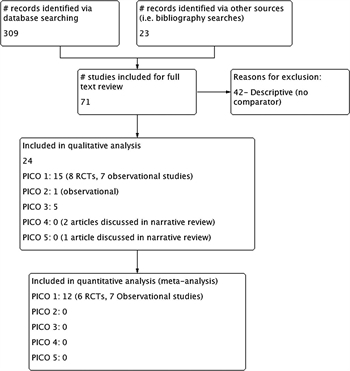
Figure 1. PRISMA study flow diagram.
The original search yielded 332 records, of which 70 were deemed to be appropriate for full text review (Fig. 1). We excluded 42 studies that were descriptive only in nature and did not have a comparator. Included studies were independently assessed by two authors; discrepancies were adjudicated by the primary author (S.M.G.). We ultimately included 28 studies in this guideline for recommendation. All of these studies were analyzed qualitatively, whereas only 12 of these studies could be included for quantitative analysis (meta-analysis). All 12 studies analyzed quantitatively pertained to PICO Question 1. For PICO Questions 2, 4, and 5, although no articles that met the strict inclusion criteria for evaluation could be found, a qualitative review was performed for articles that were tangentially pertinent to this recommendation.
Results for PICO Question 1
In adult patients with blunt thoracic trauma (P), does epidural analgesia (I) versus nonregional modalities of pain control (C) (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
Qualitative Synthesis
Analgesia
Data regarding pain scores at rest or with coughing or deep breathing were available in three studies included in this recommendation.[24–26] Pain at rest, at 24, 48, and 72 hours, was not significantly reduced by epidural analgesia compared with other analgesic modalities.[8] In Moon et al.,[24] the epidural analgesia group had a significant reduction of pain with coughing compared with patients receiving systemic opioids via patient-controlled anesthesia. Pain control in the epidural group was also significantly less on Day 3. Data on pain were available in only one observational study included in this recommendation.[27] Median pain scores were statistically lower compared with intermittent systemic morphine in Wu et al.[27] when pain scores were measured at multiple time intervals, ranging from 8 hours after epidural placement to 80 hours. In the two previously published systematic reviews, no significant difference in pain was found at rest or with coughing between the epidural analgesia and control groups at various time intervals.[8][10] It should be noted that control groups varied in these reviews and frequently included groups receiving other regional anesthetics rather than intravenous opioids.
Postoperative Pulmonary Complications
Bulger et al.[28] and Mackersie et al.[26] reported data on pneumonia development. No statistically significantly increased intervention effect was found in trials that compared opioids with epidural analgesia.[10] All six observational studies included in this review[4][6][27][29–31] reported data regarding PPCs. Reporting of PPCs was limited by definition; some studies included complications such as empyema,[29] whereas others included a variety of conditions such as acute respiratory distress syndrome.[4][6] Other studies did not provide a definition of PPCs[31] or reported only pneumonia.[27] Only one controlled study that met the inclusion criteria for this review reported data on PPCs.[26] In the previous review by Duch et al.,[10] three trials that reported data on pneumonia found no statistically significant difference between epidural analgesia and various control groups in conventional meta-analysis. Six observational studies, including 1,054 patients, reported data on various PPCs such as pneumonia, empyema, atelectasis, and acute respiratory distress syndrome.[4][6][27][29–31] Results varied widely, with one study showing an association with reduction in PPCs in the epidural analgesia group,[4] two reporting a profoundly higher incidence of PPCs in the epidural analgesia group,[6][30] and four showing no difference.[11][27][29][31]
Pulmonary Function Tests
Among the randomized controlled studies, four studies reported data on pulmonary function.[24–26][32] Vital capacity was not altered by epidural analgesia.[8] At 72 hours, maximal inspiratory pressure was greater with epidural analgesia in Moon et al.[24] No pulmonary function test data were reported in any of the six observational studies included in this recommendation.
Need for Mechanical Ventilation
The need for mechanical ventilation was not defined in any of the RCTs included in this recommendation. Three observational trials[4][27][29] reported data on need for mechanical ventilation. Of note, some trials such as that of Kieninger et al.[30] excluded mechanically ventilated patients.
Mortality
For controlled trials, no significant difference in mortality in patients treated with epidural analgesia compared with those treated with other analgesic interventions could be found.[10] For observational studies, three studies indicated a positive benefit,[4][11][29] whereas two did not.[6][30]
Hospital Length of Stay
No statistically significant difference in hospital length of stay in patients treated with epidural analgesia compared with other analgesic interventions was found.[10] In Gage et al.,[29] patients treated with epidural analgesia had a longer length of stay (11.2 vs. 8.3 days; p = 0.03). However, the comparator was not well described; this trial received several downgrades for design, indirectness, and imprecision. In Wisner’s[4] study, a lower odds of longer length of stay was reported, but this trial was also subject to concerns based on the quality of evidence. Kieninger et al.,[30] in another observational study with multiple concerns for the quality of evidence, failed to find a statistically significantly lower hospital length of stay between the epidural analgesia group and patients who received opioids. Pierre et al.[33] published an abstract with a very small patient population. This study reported shorter length of stay for patients receiving epidural analgesia, but this was not statistically significant. The most recent observational study by Zaw et al.[11] showed a statistically longer length of stay in the epidural group (15.8 vs. 15.1 days, p = 0.02), but the clinical relevance of this result (i.e., <1-day difference) is unclear.
ICU Length of Stay
No statistically significant reduction in ICU length of stay was observed; data are reported in the quantitative synthesis section.[8][10] In observational studies, four studies[11][27][29][31] reported no significant difference in ICU length of stay between the epidural analgesia group and other comparators, whereas one study reported a longer length of stay in the epidural analgesia group.[6] Pierre et al.[33] reported shorter ICU length of stay for the epidural group, but this result was not statistically significant, and the study was small and underpowered. All observational studies had multiple downgrades for quality of evidence, and none had a low risk of bias.
Quantitative Synthesis (Meta-analysis)
Analgesia
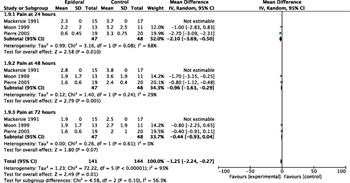
Figure 2. Forest plot for PICO 1: analgesia (RCTs).
Three controlled studies reported data on pain.[24][26][33] Pain results for these studies were reported at various intervals, including pain at 24, 48, and 72 hours, as measured on a five-point scale (transformed on a 10-point scale). Cumulatively, at 24 hours, the epidural analgesia group had lower pain (mean pain score −2.10 lower; 95% CI, −0.05 to −3.69). At 48 hours, a statistically significantly lower mean level of pain was observed, but there was no significant difference at 72 hours (relative risk, 1.93 favoring the control; 95% CI, 0.38–9.83) (Fig. 2). This analysis was limited because the majority of results were derived from the abstract by Pierre et al.,[33] heterogeneity was high (χ[2] = 72/2; I[2] = 93%), and the total number of patients included was small.
Postoperative Pulmonary Complications
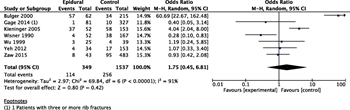
Figure 3. Forest plot for PICO 1: PPCs (observational studies).
Overall, no statistically significant difference in PPCs was found between epidural analgesia and opioid control groups among the observational studies (Fig. 3). Heterogeneity for this outcome was very high (I[2] = 91%) among the included studies, and the CIs wide.
Pulmonary Function Tests
Because of the heterogeneity of results reported, meta-analysis was not possible.
Need for Mechanical Ventilation
No RCTs were available to quantitatively analyze this outcome. The duration of mechanical ventilation was reported in three RCTs.[28][32][34] Epidural analgesia was associated with fewer ventilator days (weighted MD of −4.17; 95% CI, −5.45 to −2.88), but the number of participants was small.[8] The need for mechanical ventilation was greater in the three observational trials that reported data on this outcome.[4][27][29] Patients managed with an epidural had a higher odds of requiring mechanical ventilation (odds ratio, 2.21; 95% CI, 1.4–3.47).
Mortality
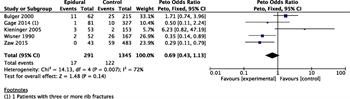
Figure 4. Forest plot for PICO 1: mortality (observational studies).
Two RCTs reported data regarding mortality.[24][28] A higher odds of death was not observed in these studies (odds ratio, 2.3; 95% CI, 0.19–27.3). In Moon et al.,[24] no deaths were reported in either group. In the four observational studies that reported data on mortality, no significant difference was found (odds ratio, 0.91; 95% CI, 0.52–1.58).[4][6][29][30] Heterogeneity was high (I[2] = 72%) for these studies, and all had a high risk of bias (Fig. 4).
Hospital Length of Stay
In four RCTs, hospital length of stay was not significantly associated with epidural analgesia.[24][26][28][32] In five observational trials that included 921 total patients, epidural analgesia was associated with longer hospital length of stay (MD, 2.36 days; 95% CI, 1.19–3.53).[6][27][29–31]
ICU Length of Stay
Four RCTs reported data on ICU length of stay.[24][28][32][34] Epidural analgesia was associated with a statistically significant decrease in mean ICU days (−3.16; 95% CI, −4.66 to −1.66); however, when only high methodological quality studies were analyzed, no difference was observed.[8] No observational studies reported data on this outcome.
Grading the Evidence
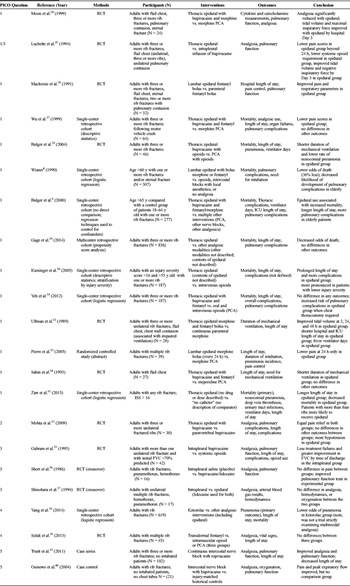
Table 1. Characteristics of Included Studies
For each outcome, we evaluated the quality of the evidence looking at the following domains: risk of bias, inconsistency, indirectness, and imprecision, or other considerations. Across all outcomes, the overall quality of evidence was very low, with some outcomes favoring epidural analgesia and other favoring nonregional analgesia. For the critical outcome analgesia, individuals who received epidural analgesia had lower pain scores. A GRADE evidence profile is presented in Table 1.
Recommendation
In adult patients with blunt thoracic trauma, we conditionally recommend epidural analgesia over nonregional modalities of pain control (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) for the treatment of pain. This recommendation is based on very low-quality evidence but places a high value on patient preferences for analgesia. If certain confounders (or effect modifiers) such as age,[4][6] number of rib fractures,[24][25][27–29][32] or severity of injury[11] are considered, a stronger positive magnitude of effect may be observed for certain outcomes of interest.
Results for PICO Question 2
In adult patients with blunt thoracic trauma (P), does paravertebral block (I) versus nonregional modalities of pain control (C) (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
Qualitative Synthesis
Only one study[13] was included for narrative review. While this study examined several of our predefined critical and important outcomes of interest, the comparator was another regional anesthetic technique rather than a nonregional modality and hence did not meet the inclusion criteria for this recommendation. Therefore, a GRADE summary of findings table was not be completed. Thirty adult patients with three or more fractured ribs were randomized to receive either continuous thoracic paravertebral block or epidural analgesia. The paravertebral block group did not demonstrate any statistically significant improvement in pain control compared with the epidural analgesia group, although both groups demonstrated significant pain relief compared with baseline. There were no deaths in either group, and the incidence of pneumonia or pleural effusion was not statistically different. Respiratory rate and peak expiratory flow rate did not differ significantly between the two groups, although the epidural analgesia group had a statistically significantly higher arterial oxygen tension/inspired oxygen ratio (PaO2/FIO2 ratio, p = 0.018). Hospital length of stay was not statistically different between the two groups.
Strengths of Mohta et al.[13] were randomization, proper sequence generation, allocation concealment, and complete outcome data. Nevertheless, the study was small and underpowered, and there were more crush injuries in the paravertebral block group, potentially limiting external generalizability. Lack of a nonregional analgesic modality as a comparator was a substantial limitation.
Recommendation
It is important to note that paravertebral block had equivalent pain control compared with epidural analgesia and provided significant pain relief compared with baseline. While desirable consequences probably outweigh undesirable consequences, because of the lack of studies comparing paravertebral block to nonregional pain control modalities, we are unable to make a recommendation regarding the use of paravertebral blocks.
Results for PICO Question 3
In adult patients with blunt thoracic trauma (P), does continuous intrapleural infusions of local anesthetics (I) versus other regional modalities of pain control (C) (i.e., epidural or paravertebral nerve blocks) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
Qualitative Synthesis
Four studies were identified for qualitative synthesis.[25][35–37] Gabram et al.[35] conducted a randomized clinical trial comparing intrapleural analgesia versus systemic opioids in nonintubated adults with more than one rib fracture. Twenty-one patients were enrolled in each group. Patients in the systemic opioid group had more rib fractures (4.4 vs. 3.4; p < 0.05) and a higher initial forced vital capacity (FVC) compared with patients in the intrapleural group. Pain scores were not reported in this study. One patient died in the opioid group versus none in the intrapleural group. The number of PPCs (i.e., atelectasis, respiratory failure, pneumonia) was not statistically significantly different between the two groups; the opioid group had two PPCs versus three in the intrapleural group. In patients with an initial FVC less than 20%, patients in the opioid group had a greater increase in FVC (26%) compared with the intrapleural group (21.8%; p > 0.05). In patients with an initial FVC greater than 20%, the intrapleural group had a statistically significantly greater improvement in FVC compared with the opioid group (23.1% vs. 10.7%; p < 0.05). One patient required intubation in the intrapleural group, whereas none required intubation in the opioid group. Neither hospital nor ICU length of stay was statistically different between the study groups. This study had a high risk of bias due to lack of blinding, no description of allocation concealment, a small sample size in the absence of a power calculation, and lack of information regarding dosing of systemic analgesics.
Short et al.[36] enrolled nonintubated patients with blunt thoracic trauma into a prospective, randomized, double-blind, crossover, placebo-controlled study. Patients received either bupivacaine (experimental) or saline (control) via an intrapleural catheter. The solutions were alternated at 24 hours so that each patient served as his/her own control. Pain control, as assessed by milligrams of morphine sulfate, was not significantly different between the experimental and placebo groups. Forced expiratory volume in 1 second (FEV1), FVC, arterial carbon dioxide tension (PaCO2), and PaO2 were not statistically significantly different between the study groups. This study was underpowered with a very small sample (15 patients) and additionally limited by no description of sequence generation or allocation concealment and imprecision.
Studies by Luchette et al.[25] and Shinohara et al.[37] compared intrapleural with epidural analgesia. Luchette et al.[25] found no significant effect between intrapleural or epidural analgesia on vital capacity, FIO2, minute ventilation, or respiratory rate. Both pain at rest and pain with movement or coughing were significantly lower in the epidural group. Patients in the epidural group also required less parenteral opioid use. Strengths of Luchette et al.[25]include a randomized design with appropriate sequence generation and complete outcome data, including physiological data. However, the study was underpowered and imprecise because of a very small sample size of 19 patients. In Shinohara et al.,[37] intrapleural analgesia was found to be equally efficacious in terms of pain control; both intrapleural and epidural analgesia significantly reduced pain. More hypotension was reported in the epidural group. No changes in PaO2 or PaCO2 were observed between the groups. Although the study was randomized, a large degree of bias was present because of lack of information regarding sequence generation, no allocation concealment, lack of blinding, and a very small sample size (N = 17).
Grading the Evidence
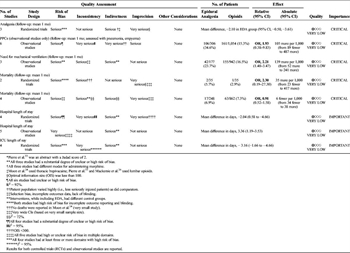
Table 2. GRADE Evidence and Summary of Findings Table for PICO 1
The overall quality of evidence was very low across all critical outcomes because of serious risk of bias, inconsistency, indirectness, and imprecision. The studies were underpowered with small sample sizes and few events. Because of these limitations, effect estimates were not pooled. A GRADE evidence profile is presented in Table 2.
Recommendation
There is limited available literature regarding intrapleural analgesia for blunt thoracic trauma. The few studies that were identified were of very poor methodological quality. Because of insufficient evidence, we are unable to make a recommendation.
Results for PICO Question 4
In adult patients with blunt thoracic trauma (P), does multimodal analgesia (I) (i.e., use of different classes of analgesics, including combinations of opioids with other agents such as NSAIDs, pregabalin/gabapentin, acetaminophen) compared with opioids alone (C) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
Qualitative Synthesis
Two studies[38][39] described a multimodal approach; however, neither study had a true comparator, and therefore, neither met the inclusion criteria for this review. Nevertheless, because a variety of critical and important outcomes related to blunt thoracic trauma were studied, these studies are included for narrative review.
Yang et al.[38] studied the effectiveness of ketorolac in reducing pulmonary morbidity in adults with rib fractures. This single-center retrospective case-control study compared 202 patients who received ketorolac versus 417 patients who did not. Both groups received various cointerventions including epidural analgesia and other NSAIDs; however, the number and type of cointerventions in both the ketorolac and historical control group were not reported, nor were the type, dosing, and route of administration of opioids. Poisson regression was used to adjust for known confounders. Both the unadjusted and adjusted odds of developing pneumonia were decreased in the ketorolac group; when adjusted for number of rib fractures, Abbreviated Injury Scale chest and extremity scores, and the presence of chronic obstructive pulmonary disease, the odds of developing pneumonia in the ketorolac group was 0.14 (95% CI, 0.04–0.46). Thirty-day ventilator-free days were significantly increased in the ketorolac group, as was 30-day ICU-free days. The lack of information regarding cointerventions is a major confounder in this study.
Solak et al.[39] conducted a prospective randomized clinical trial to determine the effectiveness of transdermal fentanyl as part of a multimodal approach for managing pain related to multiple rib fractures. Three groups were compared using three different routes for opioid administration: intramuscular pethidine (opioid), intravenous PCA with fentanyl, and transdermal fentanyl. All three groups received an intercostal nerve block and paracetamol (acetaminophen) during the first 5 days of admission. While the mean pain score decreased after treatment in each group, pain control was not statistically different among the groups when tested with analysis of variance. The study was limited by lack of blinding, lack of a direct comparison or placebo, and imprecision given the small number of subjects (N = 15) in each group.
Grading the Evidence
No studies met the inclusion criteria for this question; therefore, an evidence profile was not created. There is limited evidence of very low quality for the use of multimodal analgesia in blunt thoracic trauma.
Recommendation
Although the quality and quantity of evidence for the use of multimodal analgesia in adult patients with blunt thoracic trauma are very limited, we conditionally recommend this modality. This recommendation is based on very low-quality evidence but places a high value on patient preferences for analgesia. There is some indirect evidence that multiple analgesic modalities (i.e., transdermal fentanyl, NSAIDs), when combined, decrease pain in patients with blunt thoracic trauma. Use of alternative agents for patients with refractory pain is consistent with the clinical experience of the group, as patients often seek alternatives when a standard sole opioid regimen fails. Moreover, standard sole opioid regimens are often associated with adverse effects, especially as doses are escalated, thus requiring consideration for additional nonopioid analgesics.
Results for PICO Question 5
In adult patients with blunt thoracic trauma (P), does continuous intercostal infusions of local anesthetics (I) versus nonregional modalities of pain control (C) (i.e., intravenous or enteral analgesics such as opioids, acetaminophen, NSAIDs) improve analgesia, decrease pulmonary complications and need for mechanical ventilation, shorten length of stay, and/or decrease mortality (O)?
Qualitative Synthesis

Figure 5. Risk-of-bias summary.
No studies met the inclusion criteria for this PICO question, but two related studies[15][40] were included for narrative review. These studies warranted a brief narrative review insofar as both represent the limited literature available describing the use of intercostal nerve blocks for blunt thoracic trauma. Truitt et al.[15] examined 102 patients who were treated with intercostal nerve block catheters for three or more rib fractures. Postblock pain scores were significantly lower with coughing, and maximal sustained inspiration was statistically significantly higher postblock. When compared with 75 matched historical control patients who received epidural analgesia, mean hospital length of stay was reduced significantly (2.9 days in the intercostal nerve block group compared with 5.9 days in the historical control; p value not reported). Osinowo et al.[40] studied the efficacy of intercostal nerve block in 21 patients with rib fractures. Peak expiratory flow rates, arterial oxygen saturation, and pain scores were significantly improved postblock.
Recommendation
Because of the lack of studies that fulfilled our inclusion criteria, no evidence profile was created. Because of insufficient evidence, we are unable to make a recommendation.
Using These Guidelines in Clinical Practice

Table 3. GRADE Evidence and Summary Findings Table for PICO 3
These guidelines represent a detailed summary and comprehensive overview of the literature regarding analgesia for blunt thoracic trauma. They are meant to inform the decision-making process and not replace clinical judgment. The overall risk of bias for all studies was high (Fig. 5), with the exception of a few small, underpowered studies.[12][25][36] The limitations with the available literature precluded the formulation of strong recommendations by our panel (Table 3).
Conclusions
In summary, we propose two evidence-based recommendations regarding analgesia for patients with blunt thoracic trauma. In adult patients with blunt thoracic trauma, we conditionally recommend the use of epidural analgesia and multimodal analgesia (i.e., use of different classes of analgesics, including combinations of opioids with other agents such as NSAIDs, pregabalin/gabapentin, acetaminophen) versus opioids alone to treat pain. These recommendations are in contradistinction to the previously published Practice Management Guideline published by EAST in 2005.[9] The previous guideline included data from studies that examined the use of analgesic modalities in patients with thoracic surgery performed for reasons other than trauma and did not use the GRADE framework. Using the GRADE methodology for evaluating the data related to the outcomes of interest for this recommendation, we were unable to formulate any strong recommendations based on the very low quality of available literature pertaining specifically to patients with blunt thoracic trauma (Fig. 5). Our consensus view of the balance between desirable and undesirable consequences of analgesic interventions is based only on limited evidence but places a strong emphasis on patient values and preferences.
Despite several decades of research regarding the use of various analgesic modalities for thoracic surgery, there exists a relative paucity of data concerning optimal pain management for patients with blunt thoracic trauma. Interpretation of results from nontrauma studies is problematic; a consequence may be the slavish translation of analgesic modalities for trauma patients for which benefits and risks have not been fully verified. The GRADE approach is a systematic approach for grading the strength of management recommendations. This approach helps minimize bias and aid interpretation and explicitly requires careful identification of the patient population as a first step.[18] Our review of the literature indicates that future work is urgently required in this area, including the need for high-quality, prospective, controlled studies to evaluate analgesic modalities for patients with blunt thoracic trauma.
PICO 1: In patients with blunt thoracic trauma, we conditionally recommend the use of epidural analgesia versus opioids alone to improve analgesia and patient outcomes.
PICO 4: In patients with blunt thoracic trauma, we conditionally recommend the use of multimodal analgesia versus opioids alone to improve analgesia and patient outcomes.
Authorship
M.D., E.R.H., B.R.H.R, A.D.F, G.S., D.E.R.A., E.A.H., and S.M.G. conceived of this study. S.M.G., M.D., C.E.S., A.J.V., K.B.T., G.S., E.A.H., B.A.J, B.R.H.R, E.R.H., and E.A.H. developed the PICO questions. S.M.G., C.E.S., and A.J.V. examined the literature. S.M.G. performed the data extraction. S.M.G., B.A.J., C.E.S., A.J.V., S.S., K.B.T., B.A.J., B.R.H.R., and E.R.H contributed to the data interpretation. S.M.G., C.E.S., A.J.V., and B.R.H.R. wrote the manuscript.
Disclosure
The authors declare no conflicts of interest.
References
- Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975–979.
- Flagel BT, Luchette FA, Reed RL, Esposito TJ, Davis KA, Santaniello JM, Gamelli RL. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138:717–723.
- Kerr-Valentic MA, Arthur M, Mullins RJ, Pearson TE, Mayberry JC. Rib fracture pain and disability: can we do better? J Trauma. 2003;54:1058–1063.
- Wisner DH. A stepwise logistic regression analysis of factors affecting morbidity and mortality after thoracic trauma: effect of epidural analgesia. J Trauma. 1990;30:799–805.
- Sirmali M, Türüt H, Topçu S, Gülhan E, Yazici U, Kaya S, Tastepe I. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorc Surg. 2003;24:133–138.
- Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48:1040–1046.
- Barnea Y, Kashtan H, Skornick Y, Werbin N. Isolated rib fractures in elderly patients: mortality and morbidity. Can J Surg. 2002;45:43–46.
- Carrier FM, Turgeon AF, Nicole PC, Trépanier CA, Fergusson DA, Thauvette D, Lessard MR. Effect of epidural analgesia in patients with traumatic rib fractures: a systematic review and meta-analysis of randomized controlled trials. Can J Anesth. 2009;56:230–240.
- Simon BJ, Cushman J, Barraco R, Lane V, Luchette FA, Miglietta M, Roccaforte DJ, Spector REAST Practice Management Guidelines Work Group. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59:1256–1267.
- Duch P, Møller MH. Epidural analgesia in patients with traumatic rib fractures: a systematic review of randomised controlled trials. Acta Anaesthesiol Scand. 2015;59:698–709.
- Zaw AA, Murry J, Hoang D, Chen K, Louy C, Bloom MB, Melo N, Alban RF, Margulies DR, Ley EJ. Epidural analgesia after rib fractures. Am Surg. 2015;81:950–954.
- Richardson J, Lönnqvist PA. Thoracic paravertebral block. Br J Anaesth. 1998;81:230–238.
- Mohta M, Verma P, Saxena AK, Sethi AK, Tyagi A, Girotra G. Prospective, randomized comparison of continuous thoracic epidural and thoracic paravertebral infusion in patients with unilateral multiple fractured ribs—a pilot study. J Trauma. 2009;66:1096–1101.
- Kvalheim L, Reiestad F. Interpleural catheter in the management of postoperative pain. Anesthesiology. 1984;61:A231.
- Truitt MS, Murry J, Amos J, Lorenzo M, Mangram A, Dunn E, Moore EE. Continuous intercostal nerve blockade for rib fractures: ready for primetime? J Trauma. 2011;71:1548–1552.
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJGRADE Working Group. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–998.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJGRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926.
- Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, Stassen N, Dahm PEastern Association for the Surgery of Trauma Practice Management Guidelines Ad Hoc Committee. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73:S283–S287.
- Higgins J, Green SE. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. Oxford, UK: The Cochrane Collaboration; 2011.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384.
- Shea BJ, Bouter LM, Peterson J, Boers M, Andersson N, Ortiz Z, Ramsay T, Bai A, Shukla VK, Grimshaw JM. External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS One. 2007;2:e1350.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560.
- Moon M, Luchette FA, Gibson SW, Crews J, Sudarshan G, Hurst JM, Davis K Jr, Johannigman JA, Frame SB, Fischer JE. Prospective, randomized comparison of epidural versus parenteral opioid analgesia in thoracic trauma. Ann Surg. 1999;229:684–691.
- Luchette FA, Radafshar SM, Kaiser R, Flynn W, Hassett JM. Prospective evaluation of epidural versus intrapleural catheters for analgesia in chest wall trauma. J Trauma. 1994;36:865–869.
- Mackersie RC, Karagianes TG, Hoyt DB, Davis JW. Prospective evaluation of epidural and intravenous administration of fentanyl for pain control and restoration of ventilatory function following multiple rib fractures. J Trauma. 1991;31:443–449.
- Wu CL, Jani ND, Perkins F, Barquist E. Thoracic epidural analgesia versus intravenous patient-controlled analgesia for the treatment of rib fracture pain after motor vehicle crash. J Trauma. 1999;47:564–567.
- Bulger EM, Edwards T, Klotz P, Jurkovich GJ. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136:426–430.
- Gage A, Rivara F, Wang J, Jurkovich GJ, Arbabi S. The effect of epidural placement in patients after blunt thoracic trauma. J Trauma Acute Care Surg. 2014;76:39–45.
- Kieninger A, Bair HA, Bendick PJ, Howells GA. Epidural versus intravenous pain control in elderly patients with rib fractures. Am J Surg. 2005;189:327–330.
- Yeh DD, Kutcher ME, Knudson MM, Tang JF. Epidural analgesia for blunt thoracic injury-Which patients benefit most? Injury. 2012;43:1667–1671.
- Ullman DA, Fortune JB, Greenhouse BB, Wimpy RE, Kennedy TM. The treatment of patients with multiple rib fractures using continuous thoracic epidural narcotic infusion. Reg Anesth. 1989;14:43–47.
- Pierre E, Martin P, Frohock J, Varon A, Barquist E. Lumbar epidural morphine versus patient-controlled analgesia morphine in patients with multiple rib fractures. Anesthesiology. 2005;103:A289.
- Sahin S, Uckunkaya N, Soyal S. The role of epidural continuous pain treatment on duration of intubation, ventilation and ICU stay in flail chest injuries. Agri Dergisi. 1993;5:18–20.
- Gabram SG, Schwartz RJ, Jacobs LM, Lawrence D, Murphy MA, Morrow JS, Hopkins JS, Knauft RF. Clinical management of blunt trauma patients with unilateral rib fractures: a randomized trial. World J Surg. 1995;19:388–393.
- Short K, Sheeres D, Mlakar J, Dean R. Evaluation of intrapleural analgesia in the management of blunt traumatic chest wall pain: a clinical trial. Am Surg. 1986;62:488–493.
- Shinohara K, Iwama H, Akama Y, Tase C. Interpleural block for patients with multiple rib fractures: comparison with epidural block. J Emerg Med. 1994;12:441–446.
- Yang Y, Young JB, Schermer CR, Utter GH. Use of ketorolac is associated with decreased pneumonia following rib fractures. Am J Surg. 2014;207:566–572.
- Solak O, Oz G, Kokulu S, Solak O, Dogan G, Esme H, Ocalan K, Baki ED. The effectiveness of transdermal opioid in the management of multiple rib fractures: randomized controlled trial. Balkan Med J. 2013;30:277–281.
- Osinowo OA, Zahrani M, Softah A. Effect of intercostal nerve block with 0.5% bupivacaine on peak expiratory flow rate and arterial oxygen saturation in rib fractures. J Trauma. 2004;56:345–347.