All-Terrain Vehicle Injuries, Prevention of
Published 2018
Citation: J Trauma. 84(6):1017-1026, June 2018
Authors
Rattan, Rishi, MD; Joseph, D’Andrea, K., MD; Dente, Christopher, J., MD; Klein, Eric, N., MD; Kimbrough, Mary, K., MD; Nguyen, Jonathan, DO; Simmons, Jon, D., MD; O’Keeffe, Terence, MD; Crandall, Marie, MD
Author Information
From the DeWitt Daughtry Family Department of Surgery, University of Miami Miller School of Medicine (R.R.), Miami, Florida; Department of Surgery, New York University Winthrop (D.K.J.), Mineola, New York; Department of Surgery, Emory University School of Medicine (C.J.D.), Atlanta, Georgia; Department of Surgery, Hofstra University Zucker School of Medicine (E.N.K.), East Garden, New York; Department of Surgery, University of Arkansas for Medical Sciences (M.K.K.), Little Rock, Arkansas; Department of Surgery, Morehouse School of Medicine (J.N.), Atlanta, Georgia; Department of Surgery, University of South Alabama School of Medicine (J.D.S.), Mobile, Alabama; Department of Surgery, University of Arizona (T.O.), Tucson, Arizona; and Department of Surgery, University of Florida College of Medicine Jacksonville (M.C.), Jacksonville, Florida.
Submitted: January 1, 2018, Accepted: January 13, 2018, Published online: January 31, 2018.
Presented at: 29th Annual Scientific Assembly of the Eastern Association for the Surgery of Trauma, January 12–18, 2014 in Naples, FL.
Address for reprints: Rishi Rattan, MD, 1800 NW 10th Ave, Ste T215 (D-40), Miami, FL 33136; email: rrattan@miami.edu.
Abstract
BACKGROUND Despite increasing usage since their introduction, there exist no evidence-based guidelines on all-terrain vehicles (ATVs) and injury prevention. While the power and speed of these vehicles has increased over time, advancements in ATV safety have been rare.
METHODS A priori questions about ATV injury pattern and the effect of helmet and safety equipment use and legislation mandating use were developed. A query of MEDLINE, PubMed, Cochrane Library, and Embase for all-terrain vehicle injury was performed. Letters to the editor, case reports, book chapters, and review articles were excluded. Grading of Recommendations Assessment, Development, and Evaluation methodology was used to perform a systematic review and create recommendations.
RESULTS Twenty-eight studies were included. Helmet use reduced traumatic brain injury(TBI). However, studies examining whether legislation mandating helmet use reduced TBI had mixed results. When ATV safety legislation was enforced, overall injury rates and mortality decreased. However, enforcement varied widely and lack of enforcement led to decreased compliance with legislation and mixed results. There was not enough evidence to determine the effectiveness of non–helmet-protective equipment.
CONCLUSION Helmet use when riding an ATV reduced the rate of TBI. ATV safety legislation, when enforced, also reduced morbidity and mortality. Compliance with laws is often low, however, possibly due to poor enforcement. We recommend helmet use when riding on an ATV to reduce TBI. We conditionally recommend implementing ATV safety legislation as a means to reduce ATV injuries, noting that enforcement must go hand in hand with enactment to ensure compliance.
Overview
The US Consumer Product Safety Commission (CPSC) defines all-terrain vehicles (ATVs) as “off-road, motorized vehicles having…four low-pressure tires, a straddle seat for the operator, and handlebars for steering control.”[1] From 1982 to 2015, there were 14,129 reported ATV-related deaths in the US, with an annual average of over 500 deaths more recently.[1] Since 1982, 22% of fatalities were younger than 16 years, and of those, 44% were younger than 12 years.[1] In 2012, the last year in which data collection on ATV-related injuries was complete as of 2017, there were 573 fatalities. While reporting is ongoing for 2013 and 2014, fatalities are already 581 and 547, respectively.[1] In 2015, there were an estimated 97,200 ATV-related emergency department visits.[1] There are no data on the financial or socioeconomic impact of ATV injuries as it relates to hospital costs, lost employment, and postinjury quality of life.
Despite increases in the speed and power of ATVs since their introduction in the 1960s, few advancements have occurred in ATV safety. One of the few national safety measures was a 10-year joint decree implemented in 1988 between industry and the Department of Justice to stop sales of three-wheel ATVs after multiple independent studies demonstrated high rollover rates.[2]However, no other federal safety regulations have been implemented since its expiration. State safety regulations are minimal. Currently, the CPSC only advises avoiding roadways, ensuring all riders are younger than 16 years, mandatory helmet use, and ATV safety training courses.[3]
Since 1987, pediatric, emergency medicine, and surgical societies from multiple countries have published position statements and recommendations on ATV injury prevention, calling for mandatory helmet use, age restrictions, legislation, and industry cooperation to modify units intended for use by younger drivers.[4–11] However, there are no evidence-based practiced guidelines. The Eastern Association for the Surgery of Trauma (EAST) Guidelines Committee Injury Prevention Task Force conducted a systematic review of the literature to determine the quality of existing evidence to assess the effect of safety measures and legislation on ATV-related injury prevention.
Objectives
The objective of this systematic review was to assess the scientific evidence on ATV-related injury prevention strategies for riders. While there are myriad studies examining injury patterns, far fewer focus on injury prevention. For this study, we used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology, which has been previously validated.[12–14] The GRADE approach dictates a priori creation of questions in the Population, Intervention, Comparator, Outcome (PICO) format. The PICO questions to guide this systematic review were created using a modified Delphi method by the EAST Guidelines Committee Injury Prevention Task Force. No funding was obtained for this work. "However, J.D.S. is supported by a National Institutes of Health K08 grant (GM109113-01A1) and the American College of Surgeons Clowes Award." I will defer to the editor whether this is required in the body of the manuscript or a disclosure at the end of the manuscript is adequate.
PICO Questions
PICO Question 1: Among four-wheel ATV riders, should helmets be used to reduce the incidence of traumatic brain injury (TBI)?
PICO Question 2: Among four-wheel ATV riders, should legislation requiring the use of helmets be enacted to increase helmet utilization?
PICO Question 3: Among four-wheel ATV riders, should non-helmet protective gear be utilized to lessen injury severity?
PICO Question 4: Among four-wheel ATV riders, should legislation regarding ATVs be enacted to lessen injury severity?
Patients and Methods
Inclusion Criteria for This Review
Study Types
Studies for review included randomized controlled trials, prospective and retrospective observational studies, and case-control studies. Case reports and reviews containing no original data or analyses, editorials, and opinion articles were excluded.
Participant Types
All relevant studies were included, irrespective of age, race, sex, or other demographic characteristics.
Intervention Types
All studies of ATV injury prevention methods falling into the categories of legislation and personal protective equipment usage were included.
Outcome Measure Types
The review was limited to studies in which either helmet or protective gear use, injury, or mortality was the outcome. Since the injury reports were heterogeneous, all injuries were felt to be essential to evaluating the literature within the GRADE framework.
Review Methods
Search Strategy
A research librarian identified references in MEDLINE, PubMed, Cochrane Library, and Embase. An initial search for articles of any language published from January 1, 1985, to December 31, 2105, was conducted using relevant Medical Subject Headings (MeSH). The MeSH terms used were: off-road motor vehicles, crash, mortality, wounds and injuries, and legislation. Keywords used were: all-terrain vehicles, all terrain vehicles, ATV, and trauma. An updated focused search for articles published between December 1, 2015, and June 30, 2017 was conducted in July of 2017. In addition to the electronic search, manual review of bibliographies of articles and recent reviews was by the lead author (D.K.J.).
Study Selection
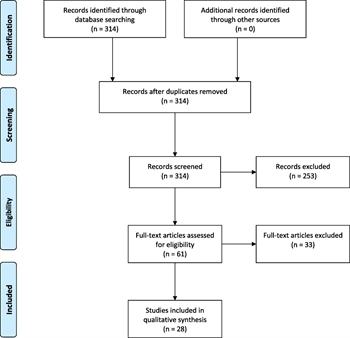
FIGURE 1. PRISMA flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Two independent researchers (R.R., D.K.J.) screened titles and abstracts using the aforementioned inclusion and exclusion criteria. Any disagreement was adjudicated by a third, senior, GRADE-trained researcher (M.C.) with experiencing in performing systematic reviews. Figure 1 demonstrates the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram outlining the study selection process.
Data Extraction and Management
All studies to be included were provided to all reviewers along with instructions and grading templates developed by GRADE and modified by EAST. Independent interpretations of the data were shared through group email, conference calls, and in-person discussion. No major reviewer discrepancies in data interpretation and extraction occurred.
Methodological Quality Assessment
Validated GRADE methodology was used.[12–14] A priori PICO questions were created. Reviewers independently assessed the quality of the data gathered through a comprehensive search that addressed each PICO question. By grading effect size, risk of bias, inconsistency, indirectness, precision, and publication bias to determine the quality of each study and the sum of all data, reviewers developed evidence-based recommendations of varying strength based on the quality of the evidence used. The GRADE methodology suggests that strong recommendations be phrased as “we recommend,” and that weak recommendations be phrased as “we conditionally recommend.”
Results
Results for Helmet Use to Reduce TBI when Riding ATVs (PICO 1)
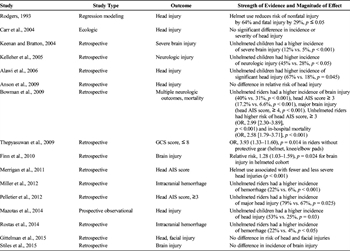
TABLE 1. Evidence Table for Helmet Use and TBI Incidence
Sixteen studies compared the incidence of traumatic brain injuries of any severity in helmeted versus unhelmeted ATV riders (Table 1). Twelve of 16 included studies demonstrated decreased rates or risk of TBI or TBI severity as determined by either Glasgow Coma Scale (GCS), Abbreviated Injury Scale (AIS), or Injury Severity Score (ISS).[15–26] The other four studies showed no difference.[27–30] Of note, the largest study in the positive group had a sample size of 11,589, while the largest study in the group without positive findings had a sample size of 285. Almost all studies were retrospective studies of patients seen in a hospital for injuries suffered secondary to an ATV crash. This has the potential to introduce selection bias. The ATV riders in the unhelmeted cohort who only required medical evaluation for TBI might not have otherwise been included in the study if a helmet prevented their TBI.
Kelleher et al.[15] noted the increase in pediatric ATV-related injuries and deaths seen at their pediatric trauma center after the Consumer Product Safety Commission “consent decree” expired in 1998. They retrospectively analyzed patients treated for ATV-related injuries from 1993 to 2003 to identify trends in patient characteristics and outcomes that might have resulted. Helmet usage was associated with a lower incidence of neurologic injury compared to no helmet use (28% vs. 45%, p < 0.05) in 184 children.
Finn and MacDonald[16] queried multiple state databases and aggregated data on 741 patients in Utah who suffered ATV-related injuries between 2001 and 2005. Among 520 patients in whom helmet usage was documented, they found a relative risk of 1.28 ([1.03–1.59], p = 0.02) for TBI in the unhelmeted cohort. They found that head injuries disproportionately affected riders younger than 20 years and recommended concentrating efforts to intervene on this population.
Noting the disproportionately high rate of ATV injuries in children compared to their rate of ridership, Mazotas et al.[17] used surveys to prospectively collect data from three pediatric trauma centers regarding crash circumstances, safety equipment use, and injuries in 84 children between 2007 and 2012. Helmet usage was associated with a lower risk of head injuries than no helmet use (25% vs. 53%, p = 0.03). They also found that many parents and injured children were unaware of recommendations against ATV use in children younger than 16 years.
Bowman et al.[22] noted the proven protective benefits of motorcycle helmets in protecting riders from head injuries and death and sought to determine if helmets offered similar benefits for ATV riders. They queried the National Trauma Data Bank for patients with ATV-related injuries between 2002 and 2006 to identify associations between helmet usage and injury severity. They found that TBI was more common in 5,732 unhelmeted riders as compared with 5,857 helmeted riders (40% vs. 31%, p < 0.01). Further, TBI in unhelmeted riders was more severe (admission GCS score, 14.3 vs. 13.6, p < 0.01; head AIS score, > 4, 9% vs. 3%, p < 0.01) and required more invasive monitoring and surgical management.
Ontario also saw an increase in ATV use among children with a concomitant increase in ATV-related trauma. Alawi et al.[18] identified 17 patients younger than 18 years from their hospital’s trauma registry who suffered major ATV-related trauma (ISS ≥ 12), with unhelmeted riders more often experiencing significant head injury (67% vs. 18%, p = 0.05). Of note, “significant head injury” was undefined and inferential statistical analysis was not performed, so this study group performed a chi-square analysis based on the published data.
Rostas et al.[19] identified all patients in their trauma registry involved in ATV crashes between 2005 and 2010. They reviewed charts and also attempted to contact all patients to gather missing data. Only 7% of patients were wearing helmets at the time of the crash. The odds ratio for intracranial hemorrhage was 7.60 ([1.02–56.8], p = 0.02) in the unhelmeted group. Riders younger than 17 years comprised 58% of the study population and helmet usage was equally poor in both adults and children.
Miller et al.[20] abstracted data from the West Virginia Trauma System registry on patients who suffered ATV-related injuries in 2010. Recreational riders were more likely to be helmeted than those injured on farms or roadways. Similar to Rostas et al., they found that helmet use was associated with a lower rate of intracranial hemorrhage (6% vs. 22%, p < 0.01).
Like most Canadian provinces, Alberta does not require ATV helmet use. Pelletier et al.[21]collected data from the Alberta trauma registry. Between 2003 and 2008, they identified 435 patients who suffered major ATV-related trauma (ISS ≥ 12). Helmet use was documented in 401 patients. Similar to Bowman, they found that helmet use was associated with a decreased rate of major head injury (head AIS, ≥3; 67% vs. 79%, p = 0.03).
Keenan and Bratton[23] compared ATV-related injuries in children younger than 16 years in Pennsylvania and West Virginia to identify differences associated with legislation. Of the 1,080 children, 843 had helmet usage documented. Helmet usage was associated with a lower rate of initial GCS score of 8 or less (4.5% vs. 11.8%, p < 0.01). On multivariate logistic regression, living in a state without helmet legislation was an independent predictor of unhelmeted ATV use (odds ratio [OR], 2.7 [1.8–4.0], p < 0.05). The primary cause of death was head injury (45.7%) and unhelmeted children comprised the majority (81%) of fatal TBI.
Thepyasuwan et al.[24] queried their hospital trauma registry to identify 156 ATV-related injuries between 2003 and 2007. They also found that lack of helmet use was associated with a relative risk of 3.93 ([1.33–11.60], p = 0.01) of arriving with a GCS score of 8 or less.
Merrigan et al.[25] queried the National Trauma Data Bank for ATV-related injuries between 2000 and 2004 and identified 10,786 patients. Helmet usage and age was recorded for 5,897 drivers and 836 passengers. Helmeted riders were less severely injured, had lower ICU and hospital lengths of stay, and were more likely to be discharged home. Helmeted drivers were less likely to die than their unhelmeted counterparts (OR, 0.38 [0.24–0.59], p < 0.01).
Rodgers[26] analyzed both nonfatally and fatally injured ATV riders from a CPSC database. Using regression modeling, he demonstrated that head injuries were more often the most severe injury in unhelmeted survivors as compared to helmeted survivors. He also demonstrated that head injury was more frequently the cause of death in unhelmeted riders as compared with helmeted riders.
In contradiction, some studies did not find an association between TBI and helmet use or non-use. Anson identified 218 cases of children younger than 16 years hospitalized in New Zealand between 2000 and 2006 for ATV injuries.[27] Children are shown to be at increased risk of injury when riding ATVs as compared with adults.[31–34] There is no legislation regarding ATV use in New Zealand and safety guidelines are widely ignored.[27] Only 38% of charts documented helmet usage, and of those, only 36% of riders had used helmets. There was no statistically different risk of head injury found between helmeted and unhelmeted children.[27]
Similar to New Zealand, children in rural Kansas frequently use ATVs for farming. From their trauma registry, Stiles et al.[28] identified 54 patients younger than 18 years who were seen for ATV-related injuries between 2007 and 2012. Helmet usage was documented in 43 patients. No difference was found in TBI rate in the helmet versus unhelmeted groups.
In Ohio, ATV usage is not regulated on private lands. Gittelman et al.[29] noted that the increasing use of ATVs and their greater engine sizes led to an increase incidence of pediatric ATV-related injuries. Collating data from seven pediatric trauma centers between 1995 and 2001, 285 cases of ATV-related injuries in children younger than 16 years were identified. Helmet use was documented in 231 patients. There was no difference in the risk of head or facial injury between helmeted and unhelmeted cohorts.
Carr et al.[30] analyzed 238 patients with ATV-related injuries admitted to their Level I trauma center in West Virginia between 1991 and 2000. Helmet usage was documented in 92% of patients. They documented the severity of head injury based on presenting GCS score, but did not perform inferential statistics. A chi-square analysis of their data demonstrates no difference in the distribution of TBI severity between the helmeted and unhelmeted cohorts.
Recommendation
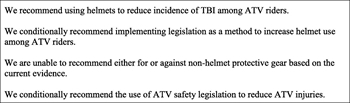
FIGURE 2. Summary of evidence-based review.
There is moderate quality evidence that helmet use decreases incidence of TBI among ATV riders, limited by risk of bias and imprecision but buttressed by a large effect. As a result, we recommend using helmets to reduce incidence of TBI among ATV riders (Fig. 2).
Results for Legislation to Increase Helmet Use (PICO 2)
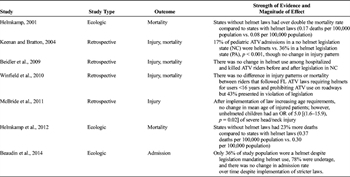
TABLE 2. Evidence Table for Helmet Legislation and Helmet Use
Of the seven studies included for review, most demonstrated that legislation increases helmet use amongst ATV riders (Table 2).[23], [35-40] However, not all studies examined how compliant its sample was in adhering to legislation mandating helmet use. In studies looking at compliance with legislation, compliance was generally low overall.[23],[37],[40]
Keenan and Bratton[23] found that the rate of helmet utilization in Pennsylvania, where helmet use has been required for riders younger than 16 years since 1985, was more than twice that of North Carolina, where no helmet legislation exists. However, Beidler et al.[36] and McBride et al.[38] found that the rates of helmet usage in North Carolina did not change after enactment of legislation in 2006 requiring their use among riders of all ages on public land. Limitations include small sample sizes and no washout period to account for the delay in changing culture and behavior after enactment of legislation.
Winfield et al.[37] found that 13% of ATV crash victims of any age seen in the hospital were wearing helmets. In Florida, only riders younger than 16 years are required to wear helmets. The study did not categorize helmet usage by age. Beaudin et al.[40] found that 53% of ATV crash victims seen in the hospital were wearing helmets. In Québec, all riders have been required to wear helmets since 1996. Helmkamp et al.'s [35],[39] studies multistate studies, while not examining helmet use specifically, found that lack of helmet legislation increased fatality rates by 23% to 53%.
All studies are limited by selection bias because they only included ATV riders who were part of hospital or medical examiner registries as a result of an ATV collision. It is conceivable that helmet legislation increases helmet utilization thereby decreasing the rate of head, neck, and face injuries, thus avoiding the need for hospitalization or death evaluated by the medical examiner. Analyzing the population of hospitalized patients could underestimate helmet utilization in ATV riders, because riders who wear helmets might be less likely to require hospital care.
Recommendation
There is low-quality evidence that helmet legislation impacts ATV helmet use, limited by risk of bias and indirectness. As a result, we conditionally recommend using legislation as a method to increase helmet use among ATV riders.
Results for the Use of Protective Gear to Lessen Injury Severity (PICO 3)

TABLE 3. Evidence Table for Nonhelmet Protective Equipment and Injury Severity
There are limited studies examining the effects of nonhelmet personal protective equipment on injury severity and none studying any possible effect independent of helmet use.[24],[41] There was one pediatric and one adult study including drivers and riders in both organized sport and recreational environments with contradictory results (Table 3).
Protective equipment including vests, boots, shin guards, and pads for the shoulders, knees, and elbows are currently marketed for ATV riders. No study could be found which only separated helmets from other protective gear; however, two studies did mention the use of other equipment. Mahida et al.[41] compared injury patterns in children who ride for sport and recreation and found that while the organized sport group more often wore extra protective gear (81% vs. 10% p < 0.01), their rates of surgery and other injury patterns were similar. Thepyasuwan et al.[24] had similar findings in their adult evaluation of patients wearing protective gear and suggested that elbow, knee, and arm pads were unlikely to help protect from intra-abdominal injuries and spine fractures.
Recommendation
There is very low-quality evidence with several limiters. As a result, we are unable to recommend either for or against non-helmet protective gear based on the current evidence.
Results for Legislation to Lessen Injury Severity (PICO 4)
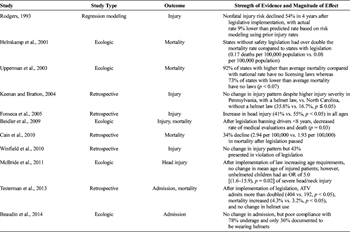
TABLE 4. Evidence Table for Legislation and Injury Severity
Of the 11 studies meeting inclusion criteria for PICO 4, most examined the outcomes of ATV injury or death, with four studying the outcome of trauma admissions, and one studying the outcome of helmet use (Table 4). All were retrospective studies. Several studies demonstrated reduced mortality and injury rates.[26],[35],[36],[42],[43] Multistate studies with large effect were consistent in this finding.[23],[26],[35],[43] Smaller studies did not always find a change in morbidity or mortality, though with noted limitations of limited study period or an increase in ATV use during the study period. When studies demonstrated poor compliance with legislation, there was still often increased helmet use with associated decreased brain injury though differences in outcome were not always demonstrated.[23],[37],[40]
In 1993, Rodgers examined whether the consent decree had any effect on injury. There was a 42% reduction in fatal TBI and 65% reduction in all brain injuries. Overall nonfatal injury rate dropped by 54%.[26] As the consent decree came towards an end in 1998, Helmkamp et al.[35] separated states based on helmet and other safety requirements, ATV-related safety, or no legislation at all. They found that states with no laws had double the mortality rates. Upperman et al.[43] subsequently assessed the pediatric population and found that there was double the mortality rate in states without any legislation. Similarly, Keenan and Bratton[23] compared states with and without ATV safety legislation between 1997 and 2000. Pennsylvania does not allow children younger than 10 years from riding, has restrictions on riders younger than 16 years, and has strict helmet laws. On the other hand, North Carolina has none of these regulations. They found that North Carolina children younger than 11 years rode unhelmeted more frequently (16.7% vs. 35.8%, p < 0.01). However, both groups still had similar rates of severe injury.
Fonseca et al.[44] compared ATV injury rate before and after the consent decree expired (1988–1998 compared to 1998–2004). There was an overall increase in the number of yearly ATV accidents (6.9 vs. 31.6, p < 0.01) and closed head injuries (41% vs. 55%, p <0.05). Compared to motorcycle riders, who still had active safety legislation, there was an increased incidence of closed head injury (54.2% vs. 44.9%, p < 0.05) and decreased helmet use (8.6% vs. 64.7%, p < 0.01) in the ATV group.
In 2006, North Carolina enacted several new mandates. Several restrictions on engine size and age were given in addition to regulation on helmets and eyewear. Additionally, no one younger than 8 years could ride an ATV. Beidler et al.[36] compared two groups, six months prior and after the laws were enacted, and found that the rates of riders 8 years to 15 years requiring hospitalization, unhelmeted riders, mortality from closed head injury, and riders under the influence did not change after the new laws were approved. However, the number of ATV riders younger than 8 years requiring medical attention did (6 vs. 0; p = 0.03). They suggest that the weak penalty for not adhering to the new legislation may have contributed to the lack of change between the two time periods. McBride et al.[38] furthered investigated the outcomes of ATV legislation in North Carolina by comparing a larger time period (2003–2008), and found that children without helmets were five times more likely to have a head or neck injury (p = 0.01). Passengers were five times more likely to die or require discharge to a rehabilitation facility (p = 0.03) and 13 times more likely to suffer a head and neck injury (p < 0.01) when compared to drivers. The authors postulate that the rate of children injured did not change between the two time periods because the overall number of ATV riders increased dramatically.
Testerman et al.[45] examined ATV admissions between 2001 and 2011. In 2006, legislation in Tennessee was enacted making it illegal to drive an ATV if: younger than 16 years, unhelmeted, with a passenger, under the influence of alcohol, or on a roadway. Despite this, the total number of admissions and deaths doubled. However, without knowing the total number of ATV riders during this period, it is difficult to determine if the rates themselves increased. Between the two groups of injured riders, severity of head, neck, thoracic and pelvic injuries tended to be higher in the postlegislation group (all p <0.05).
Cain et al.[42] examined the mortality rates in counties in West Virginia and identified that the rural counties had a higher mortality rate. Overall, however, the state had a general decrease in mortality rate over the years and they suggested this may be due to legislation passed two years prior to the study dates.
Winfield et al.[37] demonstrated that after the introduction of ATV laws, 43% of patients hospitalized for ATV accidents were still not adhering to legislation. They believe that inadequate laws and enforcement contributed to poor compliance.
Beaudin et al.[40] retrospectively reviewed injuries and rates of hospitalization for twenty years in Quebec as more ATV laws were enacted. They found that despite increasing restrictions, the number of evaluations or hospitalizations did not decrease. Furthermore, between 2005 and 2011, 45% of the patients injured on ATVs were younger than 16 years, despite laws prohibiting drivers in this age group. They believe that poor enforcement of legislation contributed to the higher percentage of underage ATV riders.
Recommendation
There is low quality evidence that legislation affects injury severity, limited by risk of bias, inconsistency, and indirectness, but with fairly consistent results around TBI. As a result, we conditionally recommend the use of ATV safety legislation to reduce ATV injuries.
Discussion
The purpose of this systematic review was to assess the quality of literature and make recommendations regarding initiatives designed to improve ATV safety. A total of 28 studies met inclusion criteria and were reviewed. As previously mentioned, the safety regulations for this particular class of motorized vehicle has lagged behind advancements in power and technology, contrasting with other motor vehicle classes. Unfortunately, there is a similar dearth in quality literature. Indeed, as a whole, we found the literature of low to very low quality and this limited our ability to make strong recommendations.
The most abundant literature in this arena revolves around the use of helmets to reduce TBI in this population.[16],[21],[25] While the bulk of these studies are retrospective or simple epidemiologic evaluations and therefore carry a risk of bias and imprecision, they are mostly consistent in their positive effect. This effect is also consistent with the findings of an EAST systematic review on the use of motorcycle helmets, published in 2010.[46] Similar to that literature in terms of quality and effect, the ATV literature, which is of moderate quality, demonstrated a large magnitude of effect, particularly in the larger studies, allowing this author group to recommend the use of helmets for ATV drivers and passengers to prevent TBI.
As previously discussed, the design and sale of ATVs has largely been self-regulated, without significant federal legislation since the mid 1990s.[25] As such, there have been multiple legislative efforts designed to regulate the use of the vehicles in addition to the use of safety equipment. Some effort has also been placed on developing and mandating the attendance of ATV buyers at a variety of training courses. Unfortunately, the literature surrounding the efficacy of these legislative efforts is of low quality and not consistent in its findings. This study highlights the limitations of the ATV literature as it fails to incorporate enough nuanced data to allow for more sophisticated statistical analysis. The other limitation of this review is that the PICO questions largely revolve around the impact of legislation in changing injury severity, which is reliant on political motivation, constituent education, and enforcement, all of which are currently substandard. To extrapolate from other motorized vehicle legislative injury prevention data: when legislation is strictly enforced, safety measure use increases and mortality decreases.
Primary enforcement of legislation allows law enforcement to stop and cite violators independent of any other traffic behavior. Secondary enforcement allows citation only when violators are stopped for another reason.[47] In a recent national analysis, compared to states with secondary enforcement of seat belt laws, primary enforcement states had an adjusted reduced incidence rate ratio of 0.83 (0.78–0.90) of motor vehicle fatality.[48] A systematic review conducted by the Centers for Disease Control found primary enforcement laws increased belt use by 14% and reduced fatality by 8% compared to secondary enforcement laws.[49] In terms of motorcycle injury prevention, universal (i.e., mandatory) helmet laws leads to higher rates of helmet use (86% vs. 55%).[47] When universal helmet laws are repealed, helmet use drops from approximately 90% to approximately 50%.[50] When a universal helmet law was reimplemented in a state that previously repealed it, helmet use reliably jumped from 42% to 87%.[51] These changes take place almost immediately after legislation becomes effective.[47] Injury prevention laws are more effective when enforcement is enhanced by publicity and education efforts.[52–54] Thus, the group felt that primary enforcement of universal legislation, combined with efforts at increasing public awareness, especially around the use of helmets, would likely play a major role in decreasing the burden of injury from ATV usage.
Even with the aforementioned limitations, our group felt we could conditionally recommend efforts of state and local governments to increase the regulatory oversight of this industry. This of particular importance with respect to helmet laws as these seem to be the most consistently effective. Overall, the ATV literature does not directly address the concept of enforcement of the various efforts of legislation but several studies suggest that efforts have been lacking. The study group’s opinion is the same.
Finally, the literature regarding the effectiveness of non-helmet protective gear is very limited in terms of its effectiveness in preventing injuries or changing injury severity. The few studies that discussed gear designed to protect the torso and extremities did not have consistent findings or were unable to reach any discrete conclusions. Therefore, the study group was unable to provide any recommendation as to their usefulness. This is a fertile area for future research.
Using These Guidelines in Clinical Practice
While robust data is lacking, there is clear evidence in both ATV injury prevention literature and other motorized vehicle injury prevention literature that helmets reduce mortality and morbidity. Further, extrapolating from several other motorized vehicle injury prevention fields, properly publicized and enforced legislation effectively improves outcomes. As such, trauma surgeons, as clinicians, researchers, citizens, and community leaders, ought to: lead the push for research and policy to reduce ATV-related injury, counsel patients accordingly, and formalize injury prevention education in communities.
Future Directions
Despite a persistently significant morbidity and mortality rate, particularly affecting children, ATV injury prevention measures remain poorly studied. Further research is needed on the effectiveness of various safety measures, especially as newer ATVs have more power and speed and thus risk. Additionally, ATV safety is an area ripe for collaboration between researchers and policymakers, similar to automobile injury prevention on the cusp of mandating seat belt use through legislation. Importantly, primary enforcement is a critical tool to improving compliance. There is a robust body of evidence that enforced safety legislation of other motorized vehicles, namely automobiles and motorcycles, has a direct effect of reducing morbidity and mortality. This must be extrapolated to ATV safety. Efforts, both scientific and governmental, must focus on reducing injuries by improving helmet use, one of the few measures with adequate evidence supporting its use to reduce morbidity. Implementation of legislation is clearly not enough and must be accompanied by institutional willingness to enforce such legislation as a way to reduce injury rates among its citizens.
Conclusion
Overall, the literature surrounding ATV safety is frustratingly incomplete and the industry remains unregulated. A broader and more detailed understanding of the epidemiology and outcomes of patients involved in ATV collisions is urgently needed. Despite these facts, the group was able to make several conditional recommendations around legislative efforts to increase the use of protective gear, especially helmets, in ATV riders (Fig. 2). Such legislative efforts, combined with public awareness campaigns and increasing efforts at enforcement are likely to have a positive effect on outcome after ATV collisions.
Authorship
T.O., C.D., M.K.K., and J.D.S. designed this study. T.O. and M.C. conducted the literature search. R.R., C.D., T.O., E.K., J.N., M.C., M.K.K., B.C., J.D.S., and D.K.J. graded the evidence. M.C., R.R., C.D., J.D.S., and T.O. interpreted the data. R.R., D.K.J., C.J.D., E.N.K., M.K.K., J.N., M.C., and J.D.S. prepared the article. R.R. and M.C. edited the article.
Acknowledgements
Brendan Campbell, Karen Lommel, and Joseph Sakran assisted with initial study design and literature review. Ellen W. MacNaughton assisted with literature searches.
Disclosures
The authors have no other disclosures.
J.D.S. is supported by a National Institutes of Health K08 grant (GM109113-01A1) and the American College of Surgeons Clowes Award.
References
- Commission USCPS. 2015 Annual Report of ATV-Related Deaths and Injuries. In: Commission USCPS. Bethesda, MD: United States Consumer Product Safety Commission; 2017.
- CPSC Approves Consent Decrees for All-Terrain Vehicle [press release]. Bethesda, MD: United States Consumer Product Safety Commission, 14 Mar 1988 1988.
- Commission USCPS. ATV Safety Information Center: Quick Facts for a Safer Ride Bethesda, MD: United States Consumer Product Safety Commission; 2014 [updated 22 May 2014. Available from: https://www.cpsc.gov/Safety-Education/Safety-Education-Centers/ATV-Safety-Information-Center/Quick-Facts-for-a-Safer-Ride/. Accessed: January 16, 2018.
- American Academy of Pediatrics Committee on Accident and Poison Prevention: all-terrain vehicles: two-, three-, and four-wheeled unlicensed motorized vehicles. Pediatrics. 1987;79(2):306–308.
- All-terrain vehicle injury prevention: two-, three-, and four-wheeled unlicensed motor vehicles. Pediatrics. 2000;105(6):1352–1354.
- Trauma Committee of the Canadian Association of Pediatric S. Canadian Association of Pediatric Surgeons' position statement on the use of all-terrain vehicles by children and youth. J Pediatr Surg. 2008;43(5):938–939.
- American College of S, Sub-Committee on Injury P, Control, Committee on T. Statement on all-terrain vehicle injuries. Bull Am Coll Surg. 2009;94(2):37–38.
- Burd R. American Pediatric Surgical Association Trauma Committee position statement on the use of all-terrain vehicles by children and youth. J Pediatr Surg. 2009;44(8):1638–1639.
- Yanchar NL. Preventing injuries from all-terrain vehicles. Paediatr Child Health. 2012;17(9):513–514.
- American College of Emergency Physicians (ACEP). Motorized recreational vehicle and watercraft safety. Policy statement. Ann Emerg Med. 2013;61(6):725–726.
- Franklin RC, Knight S, Lower T. Mount Isa statement on quad bike safety. Rural Remote Health. 2014;14(3):2687.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ, Group GW. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926.
- Jaeschke R, Guyatt GH, Dellinger P, Schunemann H, Levy MM, Kunz R, Norris S, Bion J, Group GW. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008;337:a744.
- Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, Stassen N, Dahm P. Eastern Association for the Surgery of Trauma Practice Management Guidelines Ad Hoc C. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S283–S287.
- Kelleher CM, Metze SL, Dillon PA, Mychaliska GB, Keshen TH, Foglia RP. Unsafe at any speed—kids riding all-terrain vehicles. J Pediatr Surg. 2005;40(6):929–934; discussion 934–5.
- Finn MA, MacDonald JD. A population-based study of all-terrain vehicle-related head and spinal injuries. Neurosurgery. 2010;67(4):993–997; discussion 997.
- Mazotas I, Toal M, Borrup K, Saleheen H, Hester AL, Copeland D, Danielson PD, DeRoss A, Lapidus G, Bentley G, et al. A prospective, multi-institutional study of pediatric all-terrain vehiclecrashes. J Trauma Acute Care Surg. 2014;77(1):103–108; discussion 107–8.
- Alawi K, Lynch T, Lim R. All-terrain vehicle major injury patterns in children: a five-year review in Southwestern Ontario. CJEM. 2006;8(4):277–280.
- Rostas JW, Donnellan KA, Gonzalez RP, Brevard SB, Ahmed N, Rogers EA, Stinson J, Porter JM, Replogle WH, Simmons JD. Helmet use is associated with a decrease in intracranial hemorrhage following all-terrain vehicle crashes. J Trauma Acute Care Surg. 2014;76(1):201–204.
- Miller M, Davidov D, Tillotson R, Whiteman C, Marshall T, Lander O. Injury prevention and recreational all-terrain vehicle use: the impact of helmet use in West Virginia. W V Med J. 2012;108(3):96–101.
- Pelletier JS, McKee J, Ozegovic D, Widder S. Retrospective review of all-terrain vehicle accidents in Alberta. Can J Surg. 2012;55(4):249–253.
- Bowman SM, Aitken ME, Helmkamp JC, Maham SA, Graham CJ. Impact of helmets on injuries to riders of all-terrain vehicles. Inj Prev. 2009;15(1):3–7.
- Keenan HT, Bratton SL. All-terrain vehicle legislation for children: a comparison of a state with and a state without a helmet law. Pediatrics. 2004;113(4):e330–e334.
- Thepyasuwan N, Wan XT, Davis VJ. All-terrain vehicle injuries at Arrowhead Regional Medical Center (Level II): epidemiology, risks, and outcome. Am Surg. 2009;75(10):1004–1008.
- Merrigan TL, Wall PL, Smith HL, Janus TJ, Sidwell RA. The burden of unhelmeted and uninsured ATV drivers and passengers. Traffic Inj Prev. 2011;12(3):251–255.
- Rodgers GB. All-terrain vehicle injury risks and the effects of regulation. Accid Anal Prev. 1993;25(3):335–346.
- Anson K, Segedin E, Jones P. ATV (quad bike) injuries in New Zealand children: their extent and severity. N Z Med J. 2009;122(1302):11–28.
- Stiles PJ, Helmer SD, Drake RM, Haan JM. All-terrain vehicle accidents in children. Am Surg. 2015;81(1):103–105.
- Gittelman MA, Pomerantz WJ, Groner JI, Smith GA. Pediatric all-terrain vehicle-related injuries in Ohio from 1995 to 2001: using the Injury Severity Score to determine whether helmets are a solution. Pediatrics. 2006;117(6):2190–2195.
- Carr AM, Bailes JE, Helmkamp JC, Rosen CL, Miele VJ. Neurological injury and death in all-terrain vehicle crashes in West Virginia: a 10-year retrospective review. Neurosurgery. 2004;54(4):861–867.
- Commission USCPS. All-Terrain Vehicle Exposure, Injury, Death, and Risk Studies. In: Commission USCPS. Bethesda, MD: United States Consumer Product Safety Commission; 1998.
- Commission USCPS. 2005 Annual Report of All-Terrain Vehicle (ATV)-Related Deaths and Injuries. In: Commission USCPS. Washington, D.C.: United States Consumer Product Safety Commission; 2006.
- Smith LM, Pittman MA, Marr AB, Swan K, Singh S, Akin SJ, Watson DK, Caldito G, Vidal R, Wise WR, et al. Unsafe at any age: a retrospective review of all-terrain vehicle injuries in two level I trauma centers from 1995 to 2003. J Trauma. 2005;58(4):783–788.
- Ross RT, Stuart LK, Davis FE. All-terrain vehicle injuries in children: industry-regulated failure. Am Surg. 1999;65(9):870–873.
- Helmkamp JC. A comparison of state-specific all-terrain vehicle-related death rates, 1990–1999. Am J Public Health. 2001;91(11):1792–1795.
- Beidler SK, Kromhout-Schiro S, Douillet CD, Riesenman PJ, Rich PB. North Carolina all-terrain vehicle (ATV) safety legislation: an assessment of the short-term impact on ATV-related morbidity and mortality. N C Med J. 2009;70(6):503–506.
- Winfield RD, Mozingo DW, Armstrong JH, Hollenbeck JI, Richards WT, Martin LC, Beierle EA, Lottenberg L. All-terrain vehicle safety in Florida: is legislation really the answer? Am Surg. 2010;76(2):149–153.
- McBride AS, Cline DM, Neiberg RH, Westmoreland KD. Pediatric all-terrain vehicle injuries: does legislation make a dent? Pediatr Emerg Care. 2011;27(2):97–101.
- Helmkamp JC, Aitken ME, Graham J, Campbell CR. State-specific ATV-related fatality rates: an update in the new millennium. Public Health Rep. 2012;127(4):364–374.
- Beaudin M, Dunand L, Piché N, Rousseau E, St-Vil D. Legislation in Québec for all-terrain vehicles: are we doing enough? Pediatr Emerg Care. 2014;30(3):169–173.
- Mahida JB, Asti L, Patel K, Deans KJ, Minneci PC, Groner JI, Raval MV. A comparison of injuries sustained from recreational compared to organized motorized vehicle use in children. J Pediatr Surg. 2015;50(7):1188–1191.
- Cain L, Helmkamp J. Geographic and temporal comparisons of ATV deaths in West Virginia, 2000–2008. W V Med J. 2010;106(3):26–29.
- Upperman JS, Shultz B, Gaines BA, Hackam D, Cassidy LD, Ford HR, Helmkemp J. All-terrain vehicle rules and regulations: impact on pediatric mortality. J Pediatr Surg. 2003;38(9):1284–1286.
- Fonseca AH, Ochsner MG, Bromberg WJ, Gantt D. All-terrain vehicle injuries: are they dangerous? A 6-year experience at a level I trauma center after legislative regulations expired. Am Surg. 2005;71(11):937–940; discussion 940–1.
- Testerman GM, Matrisch MS, Hensley S. Increased severe all-terrain vehicle accidents at a rural Tennessee Trauma Center despite safety legislation. Am Surg. 2013;79(5):E204–E205.
- MacLeod JB, Digiacomo JC, Tinkoff G. An evidence-based review: helmet efficacy to reduce head injury and mortality in motorcycle crashes: EAST practice management guidelines. J Trauma. 2010;69(5):1101–1111.
- Center UoNCHSR. Countermeasures That Work: A Highway Safety Countermeasure Guide for State Highway Safety Offices. 6th ed. Washington, DC: National Highway Traffic Safety Administration; 2011.
- Lee LK, Monuteaux MC, Burghardt LC, Fleegler EW, Nigrovic LE, Meehan WP, Schutzman SA, Mannix R. Motor vehicle crash fatalities in states with primary versus secondary seat belt laws: a time-series analysis. Ann Intern Med. 2015;163(3):184–190.
- Shults RA, Nichols JL, Dinh-Zarr TB, Sleet DA, Elder RW. Effectiveness of primary enforcement safety belt laws and enhanced enforcement of safety belt laws: a summary of the Guide to Community Preventive Services systematic reviews. J Safety Res. 2004;35(2):189–196.
- Ulmer RG, Preusser DF. Evaluation of the Repeal of Motorcycle Helmet Laws in Kentucky and Louisiana. Washington, DC: National Highway Traffic Safety Administration; 2003.
- Gilbert H, Chaudhary NK, Solomon MG, Preusser DF, Cosgrove L. Evaluation of the Reinstatement of the Helmet Law in Louisiana. Traffic Tech—Technology Transfer Series: Traffic Safety Facts; 2008.
- Rivara FP, Thompson DC, Patterson MQ, Thompson RS. Prevention of bicycle-related injuries: helmets, education, and legislation. Annu Rev Public Health. 1998;19:293–318.
- Kanny D, Schieber RA, Pryor V, Kresnow MJ. Effectiveness of a state law mandating use of bicycle helmets among children: an observational evaluation. Am J Epidemiol. 2001;154(11):1072–1076.
- Rodgers GB. Effects of state helmet laws on bicycle helmet use by children and adolescents. Inj Prev. 2002;8(1):42–46.
Keywords:
Injury prevention; all-terrain vehicle; brain injury; guideline; evidence-based medicine