Pulmonary Contusion and Flail Chest Management
Archived PMG
Published 2006
EAST Practice Management Workgroup
Management Workgroup for Pulmonary Contusion- Flail Chest
Bruce Simon, MD
James Ebert, MD
Faran Bokhari, MD
Jeanette Capella, MD
Timothy Emhoff, MD
Thomas Hayward III, MD
Aurelio Rodriguez, MD
Lou Smith, MD
I Statement of Problem
Thoracic injury and the ensuing complications are responsible for as much as 25 percent of blunt trauma mortality.[1] Pulmonary contusion in turn is the most common injury identified in the setting of blunt thoracic trauma, occurring in 30 to 75 per cent of all cases [2-3] Isolated pulmonary contusion may occur consequent to explosion injury, but most multi-trauma patients have concurrent injury to the chest wall.[4] Conversely, flail chest, the most severe form of blunt chest wall injury with mortality rates of 10 to 20%, is typically accompanied by significant pulmonary contusion. [5-9] While injuries to the chest wall itself may rarely be the primary cause of death in multi-trauma patients, they greatly impact management and the eventual survival of these individuals.[10] In some series, most of the severe lung contusions that require ventilatory support (85%) are associated with severe bony chest wall injury. [10]
Despite the prevalence and recognized association of pulmonary contusion and flail chest (PC-FC) as a combined, complex injury pattern with inter-related pathophysiology, the mortality and short-term morbidity of this entity has not improved over the last three decades. [12] Advances in diagnostic imaging and critical care have also failed to impact upon outcome.[12] Additionally, there may be significant long term morbidity associated with both pulmonary contusion [13] and flail chest, the true extent of which remains unclear. [14] This injury constellation particularly affects the elderly who constitute approximately 10% of the cases but consume 30% of the clinical resources.[11]
The unchanging mortality and morbidity of pulmonary contusion / flail chest has been attributed to a misunderstanding of the associated pathophysiology and a lack of scientifically proven successful management guidelines.[12] Consequently, significant controversy and a wide range of management philosophy exists particularly as relates to fluid management and ventilatory support.[7] [9] [ 15-32]
II Questions to be Addressed
This evidence based review will identify the extent and quality of scientific support for management decisions in regard to the following questions:
1. What are the appropriate principles for fluid management for patients with pulmonary contusions.?
2. Ventilatory support
a. When is mechanical ventilation indicated for FC-PC?
b. Is there are role for non-invasive ventilation?
c. What is the optimal mode of ventilation for severe pulmonary contusion and/or flail chest?
3. Is there a role for surgical fixation of flail chest injuries?
III Process
A computerized search was conducted of the Medline, Embase, Pubmed and Cochrane controlled trials databases for North American and European English language literature for the period from 1966 through June 30, 2005 . The initial search terms were “pulmonary contusion”, “flail chest”, “rib fractures”. chest injuries”, and “thoracic injuries”. This search initially yielded 91 articles. An additional 45 works were obtained from the references of these studies yielding a total of 136 papers. Thirty-eight of these articles were excluded as being case studies, reviews, letters, or otherwise irrelevant to the questions being asked. The remaining 98 studies were reviewed, graded and listed in the evidentiary table.
The practice parameter workgroup for pulmonary contusion / flail chest consisted of eight trauma surgeons, three of whom were also trained and certified as thoracic surgeons. All studies were reviewed by two committee members and graded according to the standards recommended by the EAST Ad Hoc Committee for Guideline Development.[33] Grade I evidence was also sub-graded for quality of design utilizing the Jahad Validity Scale published in Controlled Clinical Trials in 1996.[34] Any studies with conflicting grading were reviewed by the committee chairperson as were all Grade I studies. Recommendations were formulated based on a committee consensus regarding the preponderance and quality of evidence.
IV Recommendations
Level 1
There is no support for Level I recommendations regarding PC-FC.
Level II
- Trauma patients with PC-FC should not be excessively fluid restricted, but rather should be resuscitated as necessary with isotonic crystalloid or colloid solution to maintain signs of adequate tissue perfusion. Once adequately resuscitated, unnecessary fluid administration should be meticulously avoided. A pulmonary artery catheter may be useful to avoid fluid overload.
- Obligatory mechanical ventilation should be avoided.
- The use of optimal analgesia and aggressive chest physiotherapy should be applied to minimize the likelihood of respiratory failure and ensuing ventilatory support. Epidural catheter is the preferred mode of analgesia delivery in severe flail chest injury. ( see EAST PMG “Analgesia in Blunt Thoracic Trauma)
- Patients with PC-FC requiring mechanical ventilation should be supported in a manner based on institutional and physician preference and separated from the ventilator at the earliest possible time. PEEP / CPAP should be included in the ventilatory regimen.
- Steroids should not be used in the therapy of pulmonary contusion.
Level III
- A trial of mask CPAP should be considered in alert, compliant patients with marginal respiratory status
- Independent lung ventilation may be considered in severe unilateral pulmonary contusion when shunt cannot be otherwise corrected due to mal-distribution of ventilation or when crossover bleeding is problematic.
- Diuretics may be used in the setting of hydrostatic fluid overload as evidenced by elevated pulmonary capillary wedge pressures in hemodynamically stable patients or in the setting of known concurrent congestive heart failure.
- Surgical fixation may be considered in severe unilateral flail chest or in patients requiring mechanical ventilation when thoracotomy is otherwise required.
V Scientific Foundation
Historical Background
Prior to the twentieth century, the entity of pulmonary contusion had rarely been described and its clinical significance was not recognized. During World War One, signficant numbers of battlefield dead were noted to be without external signs of trauma and postmortem studies revealed lung hemorrhage. [35] [36] [37] Subsequently, the critical study during this conflict identified pulmonary contusion as the major clinically significant effect of concussive force.[38] This concept was confirmed during the second world war by studies of animals placed at varying distances from explosive charges.[39-42] It was also first noted in military studies at that time that the contused lung produces more than its normal amount of interstitial and intra-alveolar fluid. [43] Aggressive fluid resuscitation was cited as a key factor in precipitating respiratory failure after blunt thoracic trauma.[44] Further studies during the Vietnam war laid the basis for the current philosophies in treatment of pulmonary contusion.[45-47] In a study of combined pulmonary and chest wall injury Reid and Baird [48] were the first to propose that parenchymal contusion rather than bony thoracic injury was the main factor in respiratory compromise.
Similarly , until the 1960s , the paradoxical movement of the flail chest component was believed to be the cause of respiratory compromise in blunt chest wall trauma. [49] [50] It was presumed that this “Pendelluft” caused deoxygenated air to shunt back and forth to the healthy lung, rather than being exhaled, resulting in hypoxia. Consequently, treatment was aimed at correcting the paradoxical movement through a variety of methods including external fixation [51] and internal fixation by either surgical repair [52] or positive pressure ventilation.[23] [53] It was not uncommon to electively maintain patients on ventilatory support until bony union had occurred.[53] It is currently believed that the underlying lung contusion is a major cause of respiratory compromise with the bony chest wall injury creating the secondary problems of pain and splinting.[48] Contemporary practice has therefore been directed at addressing these issues. [8] [22] [54]
Pathophysiology
The local pathophysiology of injured lung was first delineated by animal studies in the 1970’s. Oppenheimer [55] studied clinical behavior and pathologic findings in class I study of contused dog lung. He identified contusions as lacerations to lung tissue which leaked blood and plasma into alveoli . He noted reduced compliance resulting in reduced ventilation per unit volume and increased shunt fraction. Other studies identified thickened alveolar septa in contused lung with consequent impaired diffusion. [56] Fulton defined the significant and progressive decrease in pO2 values in contused dog lung over a 24 hour period.[57] An increase in pulmonary vascular resistance and consequent decrease in blood flow was noted in the contused lung. In other studies, these changes were not altered by the concurrence of flail chest injury.[58] In a small observational study of blunt trauma patients, Wagner also noted increases in pulmonary vascular resistance in proportion to contused volume and felt this acted as a compensatory mechanism to minimize shunt fraction.[59]
The effects of contusion on uninjured lung have also been recently elucidated through animal studies. Davis performed an elegant class 1 study of a porcine model of blunt chest trauma.[60] Unilateral chest trauma produced an early rise in bronchoalveolar lavage (BAL) protein on the injured side as well as a delayed capillary leak in the contralateral lung. Similarly, Hellinger showed that uninjured lung, both ipsilateral and contralateral developed thickened septa, increased vacuolation and edema over an eight hour post-injury period.[56] Though this occurred to a lesser extent than in injured lung, the findings were statistically significant compared to controls (p<.01) Also, in this study, BAL showed an increase in neutrophils (PMNs) in contused lung, and ipsilateral and contralateral uninjured lung compared to controls. Local and systemic complement levels (TCC = terminal complement complex) increased and C3 complement decreased to a statistically significant level.
Consequently, high grade evidence from animal studies indicated that pulmonary contusion is not merely a localized process , but probably has global pulmonary and systemic effects when occurring in a sufficient portion of the lung. Table 1 summarizes the reported physiologic effects of lung contusion. Reviewed literature is graded and summarized in the evidentiary tables.
| Local Effects |
|---|
|
Laceration to lung tissue |
|
Hemorrhage-filled alveoli |
|
Reduced compliance yielding reduced ventilation |
|
Increased shunt fraction with decrease in pO2, increase in AaDO2 |
|
Increased pulmonary vascular resistance |
|
Decreased pulmonary blood flow |
| Injured and Uninjured Lung (Ipsilateral and Contralateral) |
|
Thickened alveolar septa with impaired diffusion |
|
Decreased alveolar diameter |
|
Vacuolation of pulmonary tissue |
|
Delayed capillary leak with increased BAL protein |
|
Increased neutrophils in lung tissue |
| Systemic |
|
Increased TCC |
|
Decreased complement |
|
PO2 = partial pressure of oxygen |
Outcome
Numerous studies have addressed the outcome of pulmonary contusion / flail chest injury (PC/FC) but have had difficulty in separating the effects of the chest wall and parenchymal components.[5] [10] [13-14] [19] [61-68] In terms of mortality, it remains controversial whether this constellation of thoracic injury is a direct cause of death [63] or merely a contributor in the setting of multi-trauma.[5] [61] [64] In separate reviews, Clark and Stellin both noted that central nervous system trauma was the most common associated injury. Few deaths in these retrospective studies ( n=144; n=203 ) were due to pulmonary failure per se, but rather to brain injury and shock. While Rellihan agreed that associated brain injury was the most common cause of death in flail chest patients, his review (class III n=85) indicated that complications of the pulmonary injury were contributory at least half the time.[64] Conversely, Kollmorgen, in a retrospective review of 100 trauma deaths among patients with pulmonary contusion felt that 70% of the deaths were due to the lung injury or pulmonary failure primarily.[63]
In terms of morbidity, the long-term outcome of flail chest injury was first addressed in the 1980’s by several workers [14] [66] In a retrospective review, Landercasper noted that 46% (n=32) of flail chest patients did not have normal chest wall expansion, 24% had obstructive changes on spirometry and 20% had restrictive changes.[66] Vital capacity was normal in only 57% 70% had long term dyspnea and 49% had persistent chest wall pain. The possible contribution of pulmonary contusion was not addressed and CT scanning was not done at this time. Similarly, Beal reviewed 20 patients with flail chest and a variety of associated thoracic injuries from 50 to 730 days and also noted that the most common long-term problems were persistent chest wall pain, chest wall deformity and exertional dyspnea.[14] The etiology of the respiratory symptoms was not identified.
In the 1990’s, attempts were made to determine whether the flail chest, pulmonary contusion or both components were responsible for the long-term disability which is seen with the more severe injuries[. 13-14] [66] [69] In a small (n=18), but well-validated, blinded Class I study, Kishikawa followed the pulmonary functions and radiographic findings of PC-FC patients for 6 months.[13] His group was trying to explain the persistent dyspnea often seen after blunt chest trauma. They noted that pulmonary function recovered within 6 months in patients without pulmonary contusion, even in the presence of severe residual chest wall deformity. However patients with pulmonary contusion had decreased functional residual capacity (FRC) and decreased supine paO2 for years afterward. Figure 1, from Kishikawa’s work shows the course of FRC in patients with pulmonary contusion with or without flail chest and with flail chest alone.
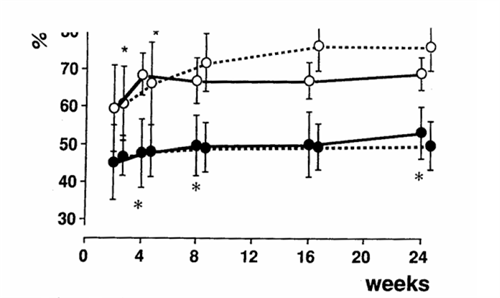
Figure 1. The course of functional residual capacity over 6 months in patients with pulmonary contusion alone (solid circle / dashed line), pulmonary contusion with flail chest (solid circle / solid line), flail chest without pulmonary contusion ( open circle / solid line), and trauma controls with neither injury (open circle / dashed line). From Kishikawa M, Yoskioka T: Pulmonary cotusion cause long-term respiratory dysfunction with decreased functional residual capacity. J Trauma 1991;32:1203-8.
In further work by Kishikawa, 58% (n=14/24) of contused lungs showed fibrosis on CT scan 1 to 6 years post-injury.[69] The average spirometry for patients with contused lungs was 76% of normal vs 98% of normal for controls. Air volume measured by CT scan supported these findings. From these studies, it was concluded that the flail chest component causes short term respiratory dysfunction while the pulmonary contusions are responsible for the long term dyspnea, low FRC and pO2. The main cause of the persistent decreased air volume was felt not to be the residual thoracic deformity but rather the loss of pulmonary parenchyma by fibrosis of the contused lung. Studies addressing the outcome of PC-FC are tabulated in the evidentiary tables.
Fluid Management
Present practice regarding type of quanitity of fluid resuscitation for multi-trauma patients with concurrent pulmonary contusion has been largely extrapolated from animal research or retrospective studies.[15-20] As early as 1973, Trinkle studied experimental right lower lobe pulmonary contusions and noted that crystalloid resuscitation caused the lesions to be larger than did colloid use.[16] Concurrent diuresis caused all lesions to decrease in size. However, when lesion size was corrected for lobe weight to body weight index, these results were not statistically significant. Also in the 70’s , Fulton studied a dog model of pulmonary contusion and noted that fluid resuscitation increased the percentage of water in the contused lung over control groups resulting in “congestive atelectasis”. This effect was unchanged whether or not the animals were allowed to hemorrhage to shock prior to volume replacement or gradually resuscitated. Similarly, Richardson performed a well-designed randomized blinded (class I) study of canine pulmonary contusion (n=34).[17] He noted that animals receiving lactated ringers at various doses had declining oxygenation levels (pO2) and increased lung water when compared to those receiving plasma. (p<.05) The authors concluded that colloid was superior to crystalloid for resuscitation in the setting of pulmonary contusion. However, in a single limb study of109 human patients with PC, Bongard [18] could not find a correlation between plasma oncotic pressure and oxygenation as determined by the PaO2/FiO2 ratio. He concluded that pulmonary dysfunction after contuson is unrelated to hemodilution by crystalloid. Finally, Richardson retrospectively reviewed 86 patients with PC and found that mortality correlated with admission pulmonary function (PaO2/FiO2 <300 ; p<.05) but not with the amount of intravenous fluid administered.[17]
Decision for Ventilatory Support
As early as 1973, Trinkle showed that early intubation and application of positive end expiratory pressure (PEEP) decreased the size of experimental pulmonary contusion vs. controls.[16] Similarly, workers such as Shin provided some class III evidence that progressive pulmonary deterioration in humans was lessened by immediate intubation and ventilation for every lung contusion.[70] Consequently, the de facto standard at that time for treatment of PC was obligatory mechanical ventilation. Yet, there was no credible data showing improved survival with this approach. [9]
Similarly, in the 1970’s it was felt that some form of stabilization of the mobile chest wall was the critical treatment for the flail chest component and that mechanical ventilation for “internal pneumatic stabilization” was the optimal way to achieve this regardless of the patient’s pulmonary function.[23] [53] Evidence supporting this was mostly observational (Class II). [23] [53] Workers such as Christensson felt that mandatory tracheostomy and two to three weeks of positive pressure ventilation would allow the chest wall to stabilize in a “favorable position [”] .[23] Follow-up studies showed return of normal mechanics but non-ventilated control groups were not utilized.
Trinkle was the first to raise the possibility that obligatory mechanical ventilation for flail chest was not necessary.[9] In a small (n=30) retrospective review with well-matched cohorts, the obligatory ventilation group had a longer hospital stay (22.6 days vs. 9.3 days, p<.005), a higher mortality ( 21% vs. 0% p<.01) and a higher complication rate ( 23 vs 2 p<.01) than the selective group. The “selective” group averaged only .6 ventilator days, indicating that the conservative management was often successful. Similarly, Richardson studied 135 patients with isolated PC and 292 patients with PC-FC.[8] Intubation was successfully avoided in 80% of patients with PC and 50% of patients with PC-FC. This study did not employ matched cohorts and the intubated patients were selected by failure of selective management. But the study did demonstrate that the majority of patients could be successfully managed without ventilatory support.
In a landmark work, Shackford and colleagues carried out a well-constructed case control study (Class II) of selective ventilatory support with the endpoints of treatment being normalization of oxygenation, shunt and alveolar-arterial oxygen gradient.[22] Their study demonstrated worse survival in the ventilated group due to the complications of mechanical ventilation. Shackford’s group concluded that mechanical ventilation should be used to correct abnormalities of gas exchange rather than to overcome instability of the chest wall. In a prospective study several years later, Shackford’s group divided FC patients (n=36) by severity of injury and provided ventilatory support only when a clinical indication developed.[25] Outcomes were compared to historical controls. Overall ventilatory rates decreased from 74% to 38% (p<.01) from the prior study and mortality from 14% to 8%. (p<.01) Other recent studies have supported the selective use of ventilatory support for defects of gas exchange and clinical indications only, rather than for correction of mechanical abnormalities of the chest wall.[7] [24] [26] Studies addressing decision for ventilatory support are reviewed and graded in the evidentiary tables.
Modes of Ventilatory Support
As early as 1972 Trinkle clearly demonstrated that the size of experimental pulmonary conrtusions in dogs was significantly decreased by the applications of PEEP.[16] The initial prospective human study by Sladen involved varying levels of PEEP in a small group of patients (n=9) who served as their own controls.[21] Despite the small study size, pO2 improved to a significant degree in all patients with PEEP of 10 or 15 cm of water. There was no change in physiologic dead space and therefore the improvements were attributed to alveolar “recruitment” or increased functional residual capacity (FRC). Rib fracture alignment was anecdotally noted to be improved on fluoroscopy but the significance of this was not addressed. Survival benefit could not be assessed as this was a single arm study.
Only occasional work has addressed the actual choice of ventilatory modes for PC-FC injuries. In the salient work on this issue, Pinella studied the use of Intermittent Mandatory Ventilation (IMV) in 144 patients with varying severity of flail chest against historical controls on Continuous Mandatory Ventilation (CMV).[27] Groups were well matched in terms of severity of flail and associated injuries. No difference could be identified in terms of duration of ventilatory support, level of PEEP or FiO2 or outcome between the CMV and IMV group.
Recent attention has focused on the use of continuous positive airway pressures modes (CPAP) both non-invasively and by endotracheal intubation.[30] [32] The critical animal study by Schweiger compared IMV to CPAP in three groups of pigs: a control group, FC group and PC-FC group.[32] Ten to 15 cm of CPAP was beneficial over IMV alone for correcting alveolar closure thereby minimizing shunt fraction (p<.001) and improving compliance significantly (p<.006) The need for IMV was signficantly reduced after the application of CPAP in all animals. (p<.01) This effect was more pronounced in PC-FC than in isolated flail chest. (p<.01) Similarly, in humans, Tanaka prospectively studied the use of non-invasive CPAP in 59 patients with FC injury. (Class II) Study patients were compared to historical controls treated for respiratory failure prmarily with mechanical ventilation.[30] Groups were well matched in terms of extent of chest wall injury and overall injury severity. The CPAP group had a lower rate of pulmonary complications (atelectasis 47% vs 95%; pneumonia 27% vs 70%; p<.01). and a significantly lower rate of mechanical ventilation. Recently, Gunduz executed a well-designed randomized comparison of mask CPAP to intermittent positive pressure ventilation via endotracheal intubation (n=52).[71] CPAP led to a lower mortality (20%, 5/25 vs 33% 7/21 p<.01) and nosocomial infection rate (4/22, 18% vs. 10/21, 48% p=.001) Mean pO2 was higher in the ET group initially ( 2 days p<.05) but then equalized. A difference in the length of ICU stay could not be demonstrated.
Independent lung ventilation (ILV) has also been employed sporadically over the last 20 years.[72-82] This modality has been applied to patients with severe unilateral chest trauma, predominantly pulmonary contusion in whom major ventilation-perfusion (V/Q) mismatch has been unresponsive to conventional support. Most of the work on this modality has consisted of case reports[72-79] or small, uncontrolled, single-limb observational studies [80-82] which report improved oxygenation and survival in patients who were failing conventional ventilation. The rationale for ILV rests with the supposition that the severe V/Q mismatch of extensive pulmonary contusion is worsened by the asymmetrical compliance of the injured lung.[72] This occurs through diversion of ventilation to more compliant areas causing over-distention of normal alveoli. Hurst and colleagues initiated ILV for eight patients with unilateral pulmonary contusion with and without flail chest who were failing conventional support.[82] Significant improvements were obtained in PaO2 ( 72+8.7 to 153+37; p<.005) and shunt fraction (28+3.5 to 12.6+2.5; p<.005) No significant changes occurred in cardiac output, peripheral resistance or oxygen extraction index. Seven of the eight patients survived. Though this study was prospective, selection was non-random and no control group was studied. (class II) Studies addressing modes of ventilatory support are reviewed and graded in the evidentiary tables.
Finally, the successful use of high frequency jet ventilation has anecdotally been reported in pulmonary contusion.[83] However the indication and effectiveness has not been formally investigated.
Surgical Repair of Flail Chest
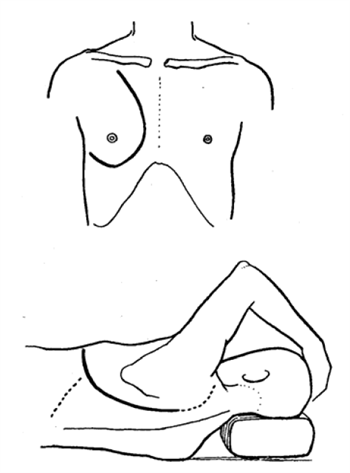
Figure 2. Incisions for internal fixation of flail chest injuries. From Moore BP. Operative Stabilization of Non-penetrating Chest Injuries. J. Thorac. Cardiovasc. Surg. 1975; 70:619-630.

Figure 3. Internal fixation of rib fracture by intramedullary nailing. From Moore BP. Operative Stabilization of Non-penetrating Chest Injuries. J. Thorac. Cardiovasc. Surg. 1975; 70:619-630.
Surgical stabilization of flail chest injury has been employed with some frequency in Europe and Asia from the 1950’s until present day.[84-89] Relatively little experience has been accrued recently in the United States.[90] The surgery involves a significant operative procedure with mobilization of large chest wall flaps or open thoracotomy.84 (see figure 2) A variety of devices are then employed to stabilize the fracture fragments including medullary wires or nails, Judet struts or compression plates. [84] [86-87] [89-91] (see figure 3) Specifics of the operative technique are beyond the scope of this review and the reader is referred to specific reports on the subject.[84] [86-87] [89-91]
Numerous European studies report “good” results with surgical fixation of FC, citing decreased pain, improved mechanics compared with pre-operative performance, “rapid” separation from mechanical ventilation and excellent return-to-work outcomes. Yet these studies are mostly small, single-limb, observational studies of personal experience lacking non-surgical controls. (classes II and III)[56] [84-85] [87] [90-94] In some, patient selection is non-random.[88-89] [91] [93-96] Consequently, though surgical fixation clearly corrects the anatomic chest deformity, comparison of efficacy to conservative treatment is problematic.[88]
Tanaka and associates performed the salient randomized, controlled study (class I) of operative fixation vs. internal pneumatic stabilization.[97] Groups (n=37) were well matched in terms of injury severity, criteria for ventilatory support and ventilator management. The incidence of pneumonia was less in the surgical group (22% vs 90%) as was the length of ventilation and length of ICU stay. The investigators reported improved lung volumes, decreased pain and dyspnea and higher return-to-work at one year with surgical fixation. All findings were significant to p<.05. Tanaka’s group concluded that surgical stabilization may be preferable for severe flail chest patients when prolonged ventilatory support would otherwise be expected. In a similar, but retrospective review of 64 patients, Balci also compared operative fixation to ventilator support.[96] The surgical group had a lower mortality (11% vs 21%), less ventilator days ( 3 vs 6.6) and less narcotic use. However, patient allocation was not randomized in this study. Finally, Voggenreiter compared the outcome of operative fixation for flail chest alone and flail with pulmonary contusion to a non-operative control group.[98] Groups were well matched. “Pure” FC patients benefited from surgical fixation in terms of separation from mechanical ventilation ( 6.5 vs 30 days; p<.02) while those with FCPC did not ( 27 vs. 30 days). These authors concluded that FC and respiratory insufficiency without underlying pulmonary contusion is an indication for surgical fixation. They felt that the presence of FC-PC precludes benefit from primary fixation but that secondary stabilization may be indicated in the weaning period. This study was uncontrolled, retrospective and involved a small sample size. No prospective, randomized controlled studies are identified comparing surgical fixation to modern conservative treatment with epidural analgesia and chest physiotherapy. Available literature addressing surgical fixation of flail chest is reviewed and graded in the evidentiary table.
Other Therapies
The use of steroids for the treatment of pulmonary contusion has rarely been addressed in the literature. Franz administered methylprednisolone 30 minutes after creation of experimental pulmonary contusion in dogs.[99] The weight ratio of contused to normal lung was significantly decreased in treated animals and the volume of injury was less on postmortem (p<.05). Since the animals were sacrificed, the effect of steroids on recovery and survival could not be assessed. In a small retrospective human study, Svennevig concluded that the mortality in severe chest injury was reduced through the use of steroids.[100] This study however, involved neither randomization nor constant criteria for administration of steroids. Since the cause of deaths were not specified, it was difficult to assess the complications and risk vs. benefit of steroid use.
VI Conclusion
Pulmonary contusion / flail chest is a common injury constellation in blunt trauma. While injuries to the chest wall itself may rarely be the primary cause of death in multi-trauma patients, they greatly impact management, survival, and long-term disability. When occurring in sufficient volume of the lung, pulmonary contusion may have adverse global pulmonary and systemic effects.
Most of the current practice in treatment of PC-FC derives from a modest quantity of Class II and III work , extrapolation of animal research and “local custom”. There is currently no credible human evidence that “fluid restriction“ improves outcome though it has been shown to improve oxygenation in animal models. Respiratory dysfunction after contusion may ultimately be shown to relate more to direct traumatic and indirect biochemical effects of the injury rather than amounts of fluid administered. In terms of ventilatory management, the bulk of current evidence favors selective use of mechanical ventilation with analgesia and chest physiotherapy being the preferred initial strategy. When support is required, no specific mode has been shown to be superior to others though there is reasonable evidence that addition of PEEP or CPAP is helpful in improving oxygenation. While the literature supporting the use of independent lung ventilation in severe unilateral. pulmonary contusion is largely observational, the majority of work supports the opinion that it may be beneficial in select patients. Finally, surgical fixation of flail chest has not been credibly compared to modern selective management, but may also be a valuable addition to the armamentarium in appropriate circumstances.
VII Areas for Further Investigation
Significant quantitative and qualitative gaps exist in the body of knowledge regarding PC-FC. Areas in need of further investigation include:
- Effect of hypertonic saline resuscitation on PC
- Anti-inflammatory “anti-cytokine” Rx
- Modes of ventilatory support
- Non-invasive ventilatory support
- Surgical fixation
- Long-term outcomes
References
- Lewis RF: Thoracic Trauma. Surg Clin North Am 69: 97-105, 1982
- Toombs BD, Sandler SV, Lester RG: Computed tomography of chest trauma. Radiology 140: 733-8. 1981.
- Webb RR Thoracic trauma. Surg Clin North Am. 54:1179-92, 1974.
- Taylor GA, Miller HA, Shulman HS, et al.: Controversies in the management of pulmonary contusion. Can J Surg 25: 167-170, 1982.
- Clark GC, Schecter WP, Trunkey DD: Variables affecting outcome in blunt chest trauma: Flail chest vs. pulmonary contusion. Jtrauma 28:298-304, 1988
- Glinz W: Problems caused by the unstable thoracic wall and by cardiac injury due to blunt injury. Injury 17:322-26, 1986.
- Miller HAB, Taylor GA, Harrison AW., et al: Management of Flail Chest. Canad Med Assoc J., 129 ;1104-7, 1983.
- Richardson JD, Adams L, Flint LM: Selective Management of flail chest and pulmonary contusion. Ann Surg., 196: 481-7, 1982.
- Trinkle JK, Richardson JD, Franz JL, et al.: Management of Flail Chest without mechanical ventilation. Ann Thorac Surg., 19: 355-363, 1975.
- Albaugh G, Kann B, Puc MM, et al: Age-adjusted Outcomes in Traumatic Flail Chest Injuries in the Elderly. Am. Surgeon. 66:978-81, 2000.
- Adegboye VO, Ladipo JK, Brimmo IA, et al: Blunt Chest Trauma. Afr. J. Med. Sci. 31:31520, 2002.
- Allen GS, Coates NE: Pulmonary Contusion: A Collective Review. Am Surg 62:895-900, 1996.
- Kishikawa M, Yoskioka T: Pulmonary contusion causes long-term respiratory dysfunction with decreased functional residual capacity. J Trauma. 312:1203-8, 1991.
- Beal SL, Oreskovich MR: Long-term Disability Associated with Flail Chest Injury. Am. J. Surg. 150:324-6, 1985.
- Fulton RL, Peter ET: Physiologic effects of fluid therapy after pulmonary contusion. Am J Surg. 126:773-7, 1973.
- Trinkle JK, Furman RW: Pulmonary Contusion: Pathogenesis and effect of various resuscitative measures. Ann Thorac Surg 16:568-73, 1973.
- Richardson JD, Franz JL: Pulmonary contusion and hemorrhage – Crystalloid versus colloid replacement. J. Surg. Res. 16:336, 1974.
- Bongard FS, Lew FR: Crystalloid resuscitation of patients with pulmonary contusion. Am J Surg 148:145, 1984.
- Johnson JA, Cogbill TH: Determinants of Outcome after Pulmonary Contusion. J Trauma 26:695-7, 1986.
- Cohn SM, Zieg PM: Resuscitation of pulmonary contusion: Effects of a red cell substitute. Crit Care Med 25:484-91, 1997.
- Sladen A, Aldredge CF, Albarran R: PEEP vs. ZEEP in the Treatment of Flail Chest Injuries. Crit. Care Med. 1:187-91, 1973.
- Shackford SR, Smith DE, Zarins CK, et al: The Management of Flail Chest. Am. J. Surg. 132:759-62, 1976.
- Christensson P, Gisselsson L, Lecerof H, et al: Early and Late Results of Controlled Ventilation in Flail Chest. Chest. 75:456-60, 1979.
- Carpintero JL, Rodriguez Diez A, Elvira JR, et al: Methods of Management of Flail Chest. Intens. Care Med. 6:217-21, 1980.
- Shackford SR, Virgilio RW, Peters RM, et al Selective Use of Ventilator Therapy in Flail Chest Injury. J. Thorac. Cardiovasc. Surg. 81:194-201, 1981.
- Dittmann M, Steenblock U, Kranzlin M, et al: Epidural Analgesia or Mechanical Ventilation for Multiple Rib Fractures. Intensive Care Med. 8:59-92, 1982.
- Pinella JC: Acute Respiratory Failure in Severe Blunt Chest Trauma. J Trauma. 22:221-225, 1982.
- Odelowo FO: Successful Management of Flail Chest Without the Use of a Volume Ventilator. J. Med. East. Afr. 64:836-844, 1987.
- Rouby JJ, Ben Ameur M, Jawish D, et al: Continuous Positive Airway Pressure (CPAP) vs. Intermittent Mandatory Pressure Release Ventilation (IMPRV) in patients with Acute Respiratory Failure. Intensive Care Med. 18:69-75, 1992.
- Tanaka H, Tajimi K, Endoh Y, et al: Penumatic Stabilization for Flail Chest Injury: An 11Year Study. Surg. Today. 31:12-17, 2001.
- Velmahos GC, Vassiliu P, Chan LS, et al. Influence of Flail Chest on Outcome Among Patients with Severe Thoracic Cage Trauma. Int. Surg. 87:240-44, 2002.
- Schweiger JW, Downs JB, Smith RA: Chest Wall Disruption with and without Acute Lung Injury: effects of Continuous Positive Airway Pressure Therapy on Ventilation and Perfusion Relationships. Crit Care Med. 31:2364-70, 2003.
- EAST Ad Hoc Committee on Practice Management Guideline Development. Utilizing Evidence Based Outcome Measures to Develop Practice Management Guidelines: A Primer. Web-published; Eastern Association for the Surgery of Trauma. 2000 (www.east.org)
- Jadad AR, Moore RA, Carroll D,.et al. Assessing the Quality of reports of randomized clinical tirals.. Controlled Clinical Trials. 17: 1-12, 1996.
- Lockwood AL, Surgical experiences in the last war. Br Med J. 1:356, 1940.
- Thomson FG. Notes on penetrating chest wounds. Br Med. J. 1:44, 1940.
- Kretzschmar CH. Wounds of the chest treated by artificial pneumothorax. Lancet 1:832, 1940.
- Hooker Dr. Physiological effects of air concussion. Am J. Physiol. 67:219, 1924.
- Zuckerman S Experimental study of blast injury to the lungs. Lancet 2:219, 1940.
- Desaga H. Blast Injuries. In: German Aviation Med WWII. Washington D.C., US Government Printing Office; 1950.
- Cameron GR, Short RHD, Wakeley CPG. Pathological changes produced in animals by depth charges. Br J Surg 30:49, 1942.
- Clark SL, Ward JW. The effects of rapid compression waves on animals submerged in water. Surg Gynecol Obstet. 77:403, 1943.
- Burford TH, Burban B. Traumatic wet lung. J Thorac Surg. 14:415, 1945.
- Brewer LA, Burbank B, Samson PC, et al. The “wet lung” in war casualties. Ann Surg. 123:343, 1946.
- Moseley RV, Doty DB, Pruit BA. Physiologic changes following chest injury in combat casualties. Surg GynecolOBstet. 129:233, 1969,
- Lichtmann MW. The problem of contused lungs. J Trauma. 10:731, 1970.
- Ratliff JL, Fletcher JR, Kopriva CJ, et al., Pulmonary contusion: a continuing management problem. J Thorac Cardiovasc Surg. 62:638, 1971.
- Reid JM, Baird WLM. Crushed chest injury: some physiological disturbances and their correction. Br Med. 1:1105, 1965.
- Moleney JV, Schmutzer, Raschke E. Paradoxical respiration and “Penedelluft:. J Thorac cardiovasc Surg. 41:291, 1961.
- Proctor H, London PS. The stove-in chest with paradoxical respiration. Brit J Surg. 42:622. 1975.
- Avery EE, Morch ET, Benson DW. Critically Crushed Chests: A New Method of Treatment. J. Thorac. Surg. 32:191-311, 1956.
- Moore BP: Operative Stabilization of Non-penetrating Chest Injuries. J. Thorac. Cardiovasc. Surg. 70:619-630, 1975.
- Diethelm AG, Battle W: Management of Flail Chest Injury: A Review of 75 Cases. Am Surgeon 37::667-70, 1971.
- Garzon AA, Seltzer B, Karlson KE. Phsyiology of crushed chest injuries. Ann Surg. 168:1368, 1968.
- Oppenheimer L, Craven KD: Pathophysiology of pulmonary contusion in dogs. J Applied Phy 47:718-728, 1979.
- Hellinger A, Konerding MA: Does lung contusion affect both the traumatized and the noninjured lung parenchyma? A morphological and morphometric study in the pig. J Trauma 39:712-9, 1995.
- Fulton RL, Peter ET: The progressive Nature of Pulmonary Contusion. Surgery 67:499-506, 1970.
- Craven KD, Oppenheimer L: Effects of contusion and flail chest on pulmonary perfusion and oxygen exchange. J Applied Phys 47:729-37, 1979.
- Wagner RB, Slivko B: Effect of lung contusion on pulmonary hemodynamics. Ann Thorac Surg 52:51-8, 1991.
- Davis KA, Fabian TC: Prostanoids: early mediators in the secondary injury that develops after unilateral pulmonary contusion. J Trauma 46:824-31, 1999.
- Stellin G: Survival in trauma victims with pulmonary contusion. Am Surg; 57:780-4, 1991.
- Hoff SJ, Shotts ST: Outcome of isolated pulmonary contusion in blunt trauma patients. Am Surg 1994; 60:139-41
- Kollmorgen DR, Murray KA: Predictors of mortality in pulmonary contusion. Am J Surg 168:659-64, 1994.
- Relihan M, Litwin MS: Morbidity and Mortality Associated With Flail Chest injury: A Review of 85 Cases. J Trauma. 13:663-71, 1973.
- Schall MA, Fischer RP, Perry JF: The Unchanged Mortality of Flail Chest Injuries. J Trauma. 19:492-6, 1979.
- Landercasper JL, Cogbill TH, Lindesmith LA: Long-term Disability after Flail Chest Injury. J trauma. 24:410-14, 1984.
- Freedland M, Wilson RF, Bender JS, et al: The Management of Flail Chest Injury: Factors Affecting Outcome. J Trauma. 30:1460-68, 1990.
- Gaillard M, Herve C, Mandin L, et al: Mortality Prognostic Factors in Chest Trauma. J Trauma. 30:93-6, 1990.
- Kishikawa M, Minami T, Shimazu T, et al: Laterality of Air Volume in Lungs Long After Blunt Chest Trauma . J Trauma. 34: 908-13, 1993
- Shin B, McAslan C: Management of lung contusion. Am Surg. 45:168-75, 1979.
- Gunduz M, Unlugenc H, Ozalevli M, et al: A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 22:325-9, 2005.
- Katsaragakis S, Stamou KM, Androulakis G: Independent lung ventilation for asymmetrical chest trauma: effect on ventilatory and haemodynamic parameters. Injury. 36:501-4, 2005.
- Terragni P, Rosboch GL, Corno E, et al: Independent high-frequency oscillatory ventilation in the management of asymmetric acute lung injury,. Anesth and Analg. 100:1793-6, 2005.
- Ost D, Corbridge T: Independent lung ventilation. Clinics in Chest Medicine. 17:591-601, 1996.
- Miller RS, Nelson LD, Rutherford EJ, et al: Synchronized independent lung ventilation in the management of a unilateral pulmonary contusion with massive hemoptysis. J Tennessee Medical Assoc. 85:374-5, 1992.
- Watts DC, Boustany CB, Lung N, et al: Pressure-controlled inverse-ratio synchronized independent lung ventilation for a blast wound to the chest. Clinical Intensive Care. 2:356-8, 1991
- Wendt M, Hachenberg T, Winde G, et al: Differential ventilation with low-flow CPAP and CPPV in the treatment of unilateral chest trauma. Intensive Care Med. 15:209-11, 1989.
- Frame SB, Marshall WJ, Clifford TG, et al. Synchronized independent lung ventilation in the management of pediatric unilateral pulmonary contusion: a case report. J. Trauma. 29:395-7, 1989.
- Albert J, Varraux AR: Independent lung ventilation. Crit Care Med. 9: 131-2, 1981.
- Cinnella G, Dambrosio M, Brienza N, et al: Independent lung ventilation in patients with unilateral pulmonary contusion. Monitoring with compliance and EtCO2. Intensive Care Med. 27: 1860-7, 2001.
- Crimi G, Candiani A, Conti G, et al: Clinical applications of independent lung ventilation with unilateral high-frequency jet ventilation (ILV-UHFJV). Intensive Care Med. 12:90-4, 1986.
- Hurst JM, DeHaven CB Jr, Branson RD: Comparison of conventional mechanical ventilation and synchronous independent lung ventilation (SILV) in the treatment of unilateral lung injury. J Trauma . 25:766-70, 1985.
- Ip-Yam PC, Allsop E, Murphy J: Combined high-frequency ventilation in the treatment of an acute lung injury Ann Acad Med, Singapore. 27:437-41, 1998.
- Moore BP: Operative Stabilization of Non-penetrating Chest Injuries. J. Thorac. Cardiovasc. Surg. 70:619-630, 1975.
- Hellberg K, deVivie ER, Fuchs K, et al: Stabilization of Flail Chest by Compression Osteosynthesis – Experimental and Clinical Results. Thorac. Cardiovasc. Surgeon. 29:27581, 1981.
- Sanchez-Lloret J, Letang E, Matsu M, et al: Indicatons and Surgical Treatment of the Traumatic Flail Chest Syndrome: An original Technique. Thorac. Cardiovasc. Surgeon. 30:294-7 1982.
- Reber P, Ris HB, Inderbitzi R, et al: Osteosynthesis of the Injured Chest all: Use of the AO Technique. Scand J Thoracic Surg. 27:137-42, 1993.
- Ahmed Z, Mohyuddin Z: Management of Flail Chest Injury: Internal Fixation Versus Endotracheal Intubation and Ventilation. J Thorac. Cardiovasc. Surg. 110:1676-80, 1995.
- Lardinois D, Krueger T, Dusmet M, et al: Pulmonary Function Testing after Operative Stabilisation of the Chest Wall for Flail Chest. Eur. J. Cardiothorac. Surg. 20:496-501, 2001.
- Thomas AN, Blaisdell W, Lewis FR, et al: Operative Stabilization for Flail Chest after Blunt Trauma. J. Thorac. Cardiovasc. Surg. 75:793-801, 1978.
- Menard A, Testart J, Philippe JM, et al: Treatment of Flail Chest with Judet’s Struts. J Thorac. Cardiovasc. Surg. 86:300-305, 1983.
- Paris F, Tarazona V, Blasco E, et al: Surgical Stabilization of Traumatic Flail Chest. Thorax. 30:521-7,1975.
- Mouton W, Lardinois D, Furrer M, et al: Long-term Follow-up of Patients with Operative Strabilisaton of a Flail Chest. Thorac. Cardiovasc. Surgeon. 45:242-4, 1997.
- Mayberry JC, Terhes JT, Ellis TJ, et al: Asbsorbable Plates for Rib Fracture Repair: Preliminary Experience. J Trauma. 55:835-9, 2003.
- Galan G, Penalver JC, Paris F, et al: Blunt Chest Injuries in 1696 Patients. Eur. J. Cardiothorac. Surg.1992; 6:284-7, 1992.
- Balci AE, Eren S, Cakir O, et al: Open Fixaton in Flail Chest: Review of 64 Patients. Asian Cardiovasc. Thorac. Ann. 12:11-15, 2004.
- Tanaka H, Yukioka T, Yamaguti Y, et al: Surgical Stabilization or Internal Pneumatic Sdtabilization? A Prospective Randomized Study of Management of Severe Flail Chest Patients. J Trauma. 53:727-32, 2002.
- Voggenreiter G, Neudeck F, Aufmkolk M: Operative Chest Wall Stabilization in Flail Chest Outcomes of Patients With or Without Pulmonary Contusion. J. Am. Coll. Surg. 187:130-8, 1998.
- Franz JL, Richardson JD: Effect of methylprednisolone sodium succinate on experimental pulmonary contusion. J Thorac & CV Surg. 5:842-4, 1974.
- Svennevig JL, Pillgram-Larsen J, Fjeld NB, et al: Early Use of Corticosteroids in Severe Closed Chest Injuries: a 10-year Experience. Injury. 18:309-12, 1987.
|
MANAGEMENT OF PULMONARY CONTUSION / FLAIL CHEST: A LITERATURE REVIEW |
||||
|
First Author |
Year |
Reference |
Data Class |
Conclusions of Study / Comments v2.1 |
|
Historical Background |
||||
|
Pulmonary Contusion (4) |
||||
|
Sealy 1 |
1946 |
Sealy WC: Contusions of the lung from non-penetrating injuries to the thorax. Arch Surg 1949; 59: 882-7 |
|
|
|
Taylor 2 |
1982 |
Taylor GA, Miller HA, et al: Symposium on Trauma: Controversies in the Management of Pulmonary Contusions. Can J Surg. 1982; 25:167-170 |
|
|
|
Allen 3 |
1996 |
Allen GS, Coates NE: Pulmonary Contusion: A Collective Review. Am Surg 1996; 62:895-900 |
|
|
|
Cohn 4 |
1997 |
Cohn SM: Pulmonary Contusion: Review of the Clinical Entity. J Trauma 1997; 42:973-9 |
|
|
|
Flail Chest (9) |
||||
|
Wilkinson 5 |
1977 |
The Management of 220 Cases of Flail Chest Injuries. J. Surg. S. Afr. 1977; 15:21-30 |
|
|
|
Shorr 6 |
1987 |
Shorr RM, Crittenden M, Indeck M: Blunt Thoracic Trauma: Analysis of 515 Patients. Ann Surg 1987; 206:201-5 |
|
|
|
Brotzu 7 |
1988 |
Brotzu G, Montisci R, Pillai W, et al: Chest Injuries: A Review of 195 patients. Ann Chir et Gyn 1988; 77:158-9 |
|
|
|
Landercasper 8 |
1990 |
Landercasper J, Cogbill TM, Strutt PJ: Delayed Diagnosis of Flail Chest. Critical Care Med 1990; 18:611-13 |
|
|
|
Mangete 9 |
1992 |
Mangete ED, Kombo BB, Igbaseimokumo U, et al: Modern Concepts in the Mangement of Flail Chest. J Med East Afric. 1992; 69:167-9 |
|
|
|
Ciraulo 10 |
1994 |
Ciraulo DL, Elliott D, Mitchell KA, et al: Flail Chest as a Marker for Significant Injuries. J Am College Surgeons. 1994;178:466-70 |
|
|
|
Adegboye 11 |
2002 |
Adegboye VO, Ladipo JK, Brimmo IA, et al: Blunt Chest Trauma. Afr. J. Med. Sci. 2002; 31:315-20 |
|
|
|
Liman 12 |
2003 |
Liman ST, Kuzucu A, Tastepe AI, et al. Chest Injury due to Blunt Trauma. Eur. J. CT Surg. 2003; 23:374-8. |
|
|
|
Sirmalt 13 |
2003 |
Sirmalt M, Turut H, Topcu S, et al: A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur. J. CT. Surg. 2003; 24:133-8 |
|
|
|
Pathophysiology |
||||
|
Pulmonary Contusion / Flail Chest (12) |
||||
|
Fulton 14 |
1970 |
Fulton RL, Peter ET: The progressive Nature of Pulmonary Contusion. Surgery 1970; 67:499506 |
2 AN |
A prospective controlled experimental animal design without randomization or blinding – 6 dogs There is a significant and progressive decrease in pO2 values in the experimentally contused dog lung over a 1-24 hour period. There is an increase in PVR and a decreased flow in the contused lung. A short trial of high concentration, moderate positive pressure ventilation did not improve the oxygen diffusion barrier. Histologic examination of the lung revealed edema and cellular infiltration of the tissue over this same time period. |
|
Blair 15 |
1976 |
Blair EB: Pulmonary Barriers to Oxygen Transport in Chest Trauma. AM Surgeon. 1976;__:55-61 |
3 |
Retrospective cohort series. 75 % of both flail and flail/contusion patients demonstrated hypoxia day one without differentiating physiologic characteristics (A-aDO2) at that time. Beginning day 3, the A-aDO2 differentiated the two groups with values of 300 mm Hg or higher indicating flail chest accompanied by contusion. In flail/contusion, the A-aDO2 reached values up to 600 mm Hg. The elevation in A-aDO2 separated the two groups until day 5 when these values began to decline in the presence of contusion. No significant difference in A-aDO2 remained at day 8.Conclusion: Blood gas analysis and the estimation of the A-aDO2 differentiate between flail chest alone and flail chest accompanied by lung contusion. A-aDO2 increases indicating pulmonary contusion precede morphological findings of the same on CXR. Declining A-aDO2 values are superior to CXR in following the improvement of pulmonary contusion. A spike in the A-aDO2 will indicate complications such as pneumonitis before identification on CXR. A-aDO2 values assist in patient management concerning ventilator support, fluid restriction, diuretic and corticosteroid usage. No statistical validation provided. |
|
Craven 16 |
1979 |
Craven KD, Oppenheimer L: Effects of contusion and flail chest on pulmonary perfusion and oxygen exchange. J Applied Phys 1979;47:729-37 |
II An |
Cohort study of 24 dogs Sig. Decrease in PaO2 and RLL perfusion as well as increase in lobe weight with contusion. Not altered by concurrence of flail chest. Decreased perfusion of RLL limited shunt. |
|
Oppenheimer 17 |
1979 |
Oppenheimer L, Craven KD: Pathophysiology of pulmonary contusion in dogs. J Applied Phy 1979;47:718-728 |
I AN |
Prospective controlled, randomized laboratory study of 25 doegs with experimental pulmonary contusion. Pulmonary contusion leaks blood and plasma into air spaces of the lung, reducing its compliance and resulting in a reduced ventilation per unit of volume and increased shunt fraction both locally in the lobe and to a lesser extent overall. Lungs ventilated wih PEEP had a higher weight than those notventilated with PEEP. PEEP increased oxygenation, but worsened contusion. |
|
Richardson 18 |
1979 |
Richardson JD, Woods D: Lung bacterial clearance following pulmonary contusion. Surgery 1979; 86:730-5 |
2 AN |
A prospective randomized non –blinded animal cohort study of 16 dogs. Aerosolized bacteria introduced into four groups 1-contusion alone; 2-contusion + fluid loading; 3 – contusion +systemic hemorrhage; 4- contusion + steroids. Stat analysis: none. Conclusions: Contusion itself does not alter bacterial lung clearance . Clearance was lowered with contusion + fluid load, contusion + systemic hemorrhage and with steroids. |
|
Tranbaugh 19 |
1982 |
Tranbaugh RF, Elings VB: Determinants of pulmonary interstitial fluid accumulation after trauma. J Trauma 1982; 22:820-6 |
3 |
Study of 16 patients with alleged severe lung injury, but no definition of criteria for same. No standardization of terms or therapies. Generalized conclusion OK: interstitial lung water increases with membrane injury from any cause |
|
Wagner 20 |
1991 |
Wagner RB, Slivko B: Effect of lung contusion on pulmonary hemodynamics. Ann Thorac Surg 1991; 52:51-8 |
2 |
Prospective nonrandomized study of 25 blunt trauma pts with pulmonary contusion. There are 3 different subpopulations of patients: the reactors (5pts), the weak reactors (10pts) and the non-reactors (10pts). This refers to pulmonary vasoconstriction per unit of lung injury (PVRI/ASF). Rank correlation coefficient was used. The PVRI increases with size of contusion (ASF) more strongly in reactors than in the non-reactors. The shunt fraction remains below 0.31 in both the reactor groups. In nonreactors the PVRI remained normal while the shunt fraction increased with extent of injury. Conclusion: Pul vasoconstriction minimizes shunt fraction in lung injury in reactors. Criticism: Non-randomized trial, no non-contusion patients as controls . |
|
Hellinger 21 |
1995 |
Hellinger A, Konerding MA: Does lung contusion affect both the traumatized and the noninjured lung parenchyma? A morphological and morphometric study in the pig. J Trauma 1995; 39:712-9 |
2 AN |
Design: Cohort study with 12 pigs. Results: Contused lung has hemorrhage, thickened septa, and decreased alveolar diameter. Uninjured lung, both ipsilateral and contralateral, has thickened septa, increased vacuoles and increased edema. BAL showed increased PMN's in both contused and contralateral lung compared to controls. There was increased PVR and mPAP after contusion and decreased Horovitz quotient, and compliance. The TCC increased and C3 decreased. Statistical methods: Chi squared test for septal thicknesses and alveolar diameters; p<0.01. Student's t test for hemodynamic and respiratory parameters; p<0.05. Conclusions: Increased septal diameter and decreased alveolar diameter occur to different extents in both contused and contralateral lung. Measurements of TCC and C3 support presence of systemic inflammatory response after direct lung injury. Structural changes are accompanied by worsening hemodynamics and lung mechanics. Strengths: Very well done. Weakness: Only 8 hour time period. Do these structural changes reverse with time? |
|
Aufmkolk 22 |
1996 |
Aufmkolk M, Fischer R, Kleinschmidt C, et al: Effect of Lung Contusion on Surfactant Composition in Multiple Trauma Patients. J Trauma. 1996; 41:1023-9 |
2 |
No definition of lung contusion. No recommendations: observations only: only direct lung injury with organ failure results in changes in surfactant, however study did not include patients with organ failure who did not have lung injury. |
|
Cohn 23 |
1996 |
Cohn SM, Zieg PM: Experimental pulmonary contusion: Review of the literature and description of a new porcine model. J Trauma 1996; 41:565-71 |
N/A |
Animal study |
|
Obertacke 24 |
1998 |
Obertacke U, Neudeck F: Local and systemic reactions after lung contusion: An experimental study in the pig. Shock 1998; 10:7-12 |
2 AN |
Controlled, randomized, non-blinded animal study of 12 pigs. Results:
Recommendation: early use of ibuprofren or pentixophyline to protect contralateral lung. Justification: well done experimental study. “Opens door” to ue of drugs that protect contralateral lung. |
|
Davis 25 |
1999 |
Davis KA, Fabian TC: Prostanoids: early mediators in the secondary injury that develops after unilateral pulmonary contusion. J Trauma 1999; 46:824-31 |
1 AN |
Design of Study: Cohort study of anesthetized ventilated pigs with unilateral blunt injury from bolt gun (n=20) versus control sham (n=5). Injured group was subdivided into no treatment versus administration of Indomethacin 15 minutes before injury Type: Cohort. Number of Patients: 25 Animal. Results: Contusion resulted in a significant: rise in pulmonary artery pressure and hypoxia with decrease in PaO2 to 50% of baseline within 1 hour of injury. Indomethacin group had a higher PaO2 than no treatment group at every level of PEEP. Unilateral chest trauma produced an early rise in BAL protein on the injured side and a delayed capillary leak on the contralateral side. These changes were reduced by 40-60% with indomethacin. Thromboxane rise post injury blocked by indomethacin and Prostacyclin rise delayed by indomethacin for 18 hours. Statistical Methods / Significance: Analysis of variance and Fisher Exact test with 95% CI Conclusions / Recommendations of Study: Indomethacin blocked or attenuated two inflammatory mediators but did not prevent the progression of pulmonary failure. Jadad Validity Scale for Grade I Evidence Study described as randomized = 0/1 no but implied Randomization appropriate=0 Study described as double blinded=0 Blinding appropriate=0 Description of withdrawals or dropouts=0 Total=0.5 Justification grading: Limited numbers in animal study, animals always ventilated in controlled environment, treatment group pretreated prior to injury, frequent use of bilateral BAL, potential for ventilator induced lung injury from ventilator protocol in study. |
|
Borrelly 26 |
2005 |
Borrelly J, Aazami MH: New insights into the pathophysiology of the flail segment: implications of the anterior serratus muscle in parietal failure. Eur J CT Surg. 2005; 28:742-9 |
3 |
N=127.Authors demonstrated via radiographic studies that flail segments secondarily dislocate through a complex set of actions involving the serratus anterior and other muscles. They present this concept as a logical indication for surgical repair of flail segments. |
|
OUTCOME |
||||
|
Pulmonary Contusion (7) |
||||
|
Johnson (*2) 27 |
1986 |
Johnson JA, Cogbill TH: Determinants of Outcome after Pulmonary Contusion. J Trauma 1986; 26:695-7 |
|
|
|
Clark 28 |
1988 |
Clark GC, Schecter WP: Variables affecting outcome in blunt chest trauma: Flail chest vs. pulmonary contusion. J Trauma 1988; 28:298-304 |
3 |
Design: Retrospective chart review of 144 patients. Results: Main outcome variable was mortality. Fifteen percent of those with first and second rib fractures had an aortic injury. Twenty-eight percent of those with lower left rib fractures had a splenic injury. Fifty -six percent of those with lower right rib fractures had a liver injury. CNS injuries were the most common associated injury and most common cause of death. Those with flail chest and flail + pulmonary contusion had higher ISS, and higher morbidity and mortality. Atelectasis and pneumonia were the most common complications. ARDS was infrequent. Did not include isolated pneumothorax, hemothorax or rib fractures. Statistics: Two tailed Student's t test for age, ISS, number days ventilated, length of stay, days in ICU. Chi square test for male:female ratio, % ventilated, shock incidence, % associated thoracic injuries and incidence of complications. P<0.05 Conclusions: Those with first and second rib fractures should get aortography. Mortality was associated with shock, high ISS, brain injury, falls from heights, combination pulmonary contusion and flail, associated aortic injury. Few deaths were due to pulmonary failure but rather brain injury and shock. Strength: Main conclusions supported. Weaknesses: Retrospective. Cannot be sure all appropriate patients were included. Were there really only 144 patients over five years? |
|
Kishikawa 29 |
1991 |
Kishikawa M, Yoskioka T: Pulmonary contusion causes long-term respiratory dysfunction with decreased functional residual capacity. J Trauma 1991; :12038 |
1 Jadad 4 |
Prospective randomized blinded study measuring PFTS, particularly FRC in patients with PC and without. Results” In PC group, FRC remains abnormal > 6 months. Conclusions: Flail chest component causes short term respiratory disfunction while PC causes long term dysfunction with dyspnea, low FRC and PaO2.. Justify grading: well done study with stat support. Conclusions are supported by study. |
|
Stellin 30 |
1991 |
Stellin G: Survival in trauma victims with pulmonary contusion. Am Surg 1991; 57:780-4 |
3 |
Design of Study: Retrospective review from single trauma center over 5 years. All patients had either a pneumothorax or hemothorax or both. Contusions were defined with radiological evidence of progression on CXR or CT scan. Isolated rib fractures without evidence of pulmonary contusion were excluded. Type: Observational. Number of Patients: 203 Human. Results: Mortality for contusion 20% but 42% if patient older than 60. Flail chest occurred in 8% of patients with 30% mortality rate. 68% of patients who died had GCS<7 with 43% brain death. 25% died in ER. 34% of patients (all survivors) never required intubation. Statistical Methods / Significance: Chi square analysis of two proportions with Yate’s correction. P<0.05. Conclusions / Recommendations of Study: Head injury associated with presence of shock is responsible for high mortality of chest injuries. Justification grading: Limited numbers and lack of detailed homogenous subgroups with true isolated pulmonary contusions prevents quantification of true pulmonary outcomes. |
|
Kishikawa 31 |
1993 |
Kishikawa M, Minami T, Shimazu T, et al. Laterality of Air Volume in Lungs Long After Blunt Chest Trauma . J Trauma 1993;34: 908-13 |
3 |
Retrospective review Results: 17 patients with severe blunt chest trauma and lung contusion were compared with 10 normal volunteers (control group) to clarify the cause of persistent decreased lung capacity. Ten patients had unilateral lung contusions, and 7 bilateral lung contusions. Flail chest was diagnosed in 7 patients with unilateral lung contusions and in 4 with bilateral lung contusion. CT scanning was used to measure air volume laterality in contused lung and compared reliably with spirometry measurements. 14 of 24 (58%) contused lungs showed fibrosis on CT scan 1 to 6 years following blunt chest trauma. The average air volume spirometry in patients with contused lungs was (76% +/- 8%) compared with the controls (98% +/-5%). The average air volume measured by CT (71% +/-8%).:: Paired or unpaired Student’s t test. Probabilities less than 5% (p<0.05) were considered significant. Conclusions: The main cause of decreased AV (air volume) is not thoracic deformity remaining after flail chest, but loss of pulmonary parenchyma from the constriction of fibrosis. Lung AV is decreased in patients with lung contusion long after blunt chest trauma; air volume of unilaterally injured lungs is severely reduced on the contused side, CT scans show fibrosis changes in contused lung long after the injury, persistent decreased AV long after lung contusion seems to be induced by fibrosis generated in the contused lung. |
|
Hoff 32 |
1994 |
Hoff SJ, Shotts ST: Outcome of isolated pulmonary contusion in blunt trauma patients. Am Surg 1994; 60:139-41 |
3 |
Retrospective chart review of 94 pts (less than 50 yo) with isolated pul contusion defined by cxr and iss of <25. 79% of the pts had a good outcome and 21% a bad outcome as defined by pneumonia 2%,atelactasis(needing bronch) 16%,effusion *%,bronchopleural fistula 5%,empyema 2%, bacteremia 1%. Poor outcome predicted by (univariate analysis) 1. pul contusion on admission cxr, hypoxia on admission, need for chest tube, high chest tube drainage, hypoxia on admission (po2<70 or po2/fiO2<250). On multivariate analysis only po2/fio2<250 was an independent predictor of poor outcome. There was no mortality. Conclusion: Isolated pul contusion causes no mortality and is predicted by low P/F ratios. Criticism: No clear def of how the pts were defined as having pul contusion’. No controls. Retro chart review with inherent bias. |
|
Kollmorgen (*2) 33 |
1994 |
Kollmorgen DR, Murray KA: Predictors of mortality in pulmonary contusion. Am J Surg 1994; 168:659-64 |
3 |
Design of Study: Retrospective single trauma center over 5 years of all trauma patients with pulmonary contusion defined radiologically or by the presence of flail chest. Type: Observational_X__Cohort___Prevalence___Case Control___ Number of Patients: 100 consecutive patients Human__X__ or Animal_____ Results: 97% of injuries blunt. 52% required intubation. Overall 10% mortality with 70% mortality attributed to a direct consequence of pulmonary failure or lung injury. Flail chest in 17% with 30% mortality. ISS and transfusion requirements higher and GCS and PaO2/FiO2 ratios lower in non-survivors. On regression patient age, oxygenation 24 post admission, resuscitation volume correlated with mortality. Of note, correlation between resuscitation volume and ISS significant (p<0.01)but correlation between resuscitation volume and oxygenation was not p(0.49). Statistical Methods / Significance: One way ANOVA and multivariate regression analysis. P<0.05 Conclusions / Recommendations of Study: Outcome of pulmonary contusion is dependent on a number of variables including the severity of pulmonary injury Justification grading: Limited number of patients, regression data overfit into limited data set which partly explains inability to narrow variable set. Also key variables not included in regression or based on even more limited subsets because of inadequate data. |
|
Balci 34 |
2005 |
Balci AE, Balci TA, Eren S, et al: Unilateral post-traumatic pulmonary contusion: findings of a review. Surgery Today. 2005, 35:205-210 |
3 |
Restrospective review of 107 patients with PC. Perfusion scans were done and a contusion score was utilized ranging from 1 to 9, where 9 represented entire lung contusion. Mortality was 15%. Mortality was predicted by age > 60, ISS>25, transfusion > 4 untis, paO2/FiO2 <300, concurrent flail chest and contusion score >7. (all p<.05) |
|
Flail Chest (7) |
||||
|
Relihan 35 |
1973 |
Relihan M, Litwin MS: Morbidity and Mortality Associated With Flail Chest injury: A Review of 85 Cases. J Trauma. 1973; 13:66371 |
3 |
Retrospective review of 85 cases: Results:. 3. Age and gender did not affect mortality. 4. Left lateral flail was more common than anterior or right sided. 5. Hypovolemia and pulmonary infection predominated as complications. 6. Patients who died more than 48 hours after admission had cranial injury 63% of the time and multiple fractures 50% of the time. Pulmonary infection was felt to directly contribute to the deaths in 50% of the group. 56% were hypovolemic at some point during the hospitalization. 25% had significant UGI bleeding from ulcer disease. 7.In comparing patients with and without head injury, death was more common in the head injured group (68 vs. 19%). Pulmonary complications were more common in the head injured group. (53% vs. 18%). 8. Pseudomonas and Staph aureus were the predominant organism of pulmonary infections amongst survivors and non-survivors. 9. A. auregonese, P Vulgaris, E.Coli, and K. pneumonia were more common (p<0.01) in patients who did not survive. Stats:Means, percentages, method sometimes omitted from method section and graphs Conclusions: 1. Recognition as a multiply injured group. Multidisciplinary approach of skilled, trained physicians, etc. to avoid therapeutic omissions and excesses. |
|
Schaal 36 |
1979 |
Schall MA, Fischer RP, Perry JF: The Unchanged Mortality of Flail Chest Injuries. J Trauma. 1979; 19:492-6 |
3 |
Retrospective review of 685 patients with thoracic trauma 1968-77 vs historical controls. Mortality changed significantly for those patients with one or more major extrathoracic injury whose major thoracic injury was a hemothorax. Conclusion: main determinant of mortality was shock of extrathoracic origin and head trauma. Stat methods not provided. |
|
Landercasper 37 |
1984 |
Landercasper JL, Cogbill TH, Lindesmith LA: Long-term Disability after Flail Chest Injury. J trauma. 1984; 24:410-14 |
2 |
Design: Retrospective chart review and prospective observations. Of 62 original patients, 32 were followed up. The rest died or were lost to follow up. 26 had CXR's. 21 had spirometry. 20 had CO diffusion study. 20 had dyspnea index. Results: 43% fully employed, 7% changed profession, 11% part-time and 39% not employed. All CXR's abnormal. 46% could not expand chest > 5cm. Spirometry showed 24% with obstructive airway changes, 20 % with restrictive findings and 15% with both. Vital capacity normal in 57% who were on vent and 22% of those off vent. CO diffusion normal in 90%. Mild dyspnea in 50% and moderate in 20%. Statistics: None. Conclusions: Impaired pulmonary function in most patients. Dyspnea in 70%. Pain in 49%. 80% with abnormal dyspnea index. Spirometry abnormal in 57%. Return to normal work 43%. Strengths: Not many previous studies looking at long term disability in patients with flail chest. This is a start. Weaknesses: No information on preinjury function or employment or activity. NO explanation of why all 32 available patients didn't get all of the objective studies done. No discussion of how other injuries may have affected the patients' ability to work. |
|
Beal 38 |
1985 |
Beal SL, Oreskovich MR: Long-term Disability Associated with Flail Chest Injury. Am. J. Surg. 1985;150:324-6. |
3 |
Retrospective review: 20 patients with flail chest and associated intrathoracic injuries, pulmonary contusion, hemothorax, and pneumothorax were followed in an outpatient setting from 50 to 732 days following injury. Group I (11), those with no extra-thoracic injury, 33% fully recovered and 67% had permanent sequelae after flail chest injury. One patient in Group I was not evaluated due to his placement in a nursing home. Group II (9), includes extra-thoracic injuries which were not thought to contribute to outcome, 40% were fully recovered and 60% had permanent sequelae. One patient in Group II was not evaluated due to his presence in an extended care facility. Two groups were compared using the chi-square or Student’s t test. Conclusion: The most common long-term problems after flail chest injury are persistent chest wall pain, chest wall deformity, and dyspnea on exertion. |
|
Freedland 39 |
1990 |
Freedland M, Wilson RF, Bender JS, et al: The Management of Flail Chest Injury: Factors Affecting Outcome. J Trauma. 1990; 30:1460-68. |
3 |
Retrospectiive review of 57 patients. Results: factors affecting outcome: etiology; age, extent of flail; assoc pulmonary contusion, HPTX, assoc. injuries, ISS. Recommendations: unsupported: fluid restriction; pain control |
|
Gaillard 40 |
1990 |
Gaillard M, Herve C, Mandin L, et al: Mortality Prognostic Factors in Chest Trauma. J Trauma. 1990; 30:93-6. |
3 |
Numbers don't add up: more chest injuries than there are patients: some had multiple injuries: not addressed. Self-fulfilling conclusion: more injured patients had higher mortality; no matched control group without chest trauma. Age was not addressed. No mention of associated injuries in the chest trauma patients |
|
Albaugh 41 |
2000 |
Allbaugh G, Kann B, Puc MM, et al: Age-adjusted Outcomes in Traumatic Flail Chest Injuries in the Elderly. Am. Surgeon. 2000; 66:978-81. |
3 |
58 pts who had flail chest were included in the retrospective chart review. They were divided into 2 groups: under 55yo(32pts) and over 55yo(26pts). No difference in groups re:ISS,LOS, vent days, head injury, tracheostomy, pneumonia development, ARDS. Older group has higher mort 58% vs 16%. Mort increases 132% for every 10 yr increase in age. Wicoxon t test. X2 and logistic regression used. 95% confidence interval used. Conclusion: Age is predictor of outcome with flail chest and shows increased mort. Criticism: Retrospective chart review without any controls. The two groups are not very comparable: many more males in first group. |
|
Athanassiadi 42 |
2004 |
Athanassiadi K, Gerazounis M, Theakos N: Management of 150 flail chest injuries: analysis of risk factors affecting outcome.Eur J. CT Surg.2004; 26:373-6. |
3 |
Retrospective review. Main factors correlating with adverse outcome (p,>05) were ISS and presence of associated injuries. Age and hemopneumothorax did not affect did not affect mortality but did influence length of stay. Main findings are as expected. |
|
Fluid Management (9) |
||||
|
Fulton 43 |
1973 |
Fulton RL, Peter ET: Physiologic effects of fluid therapy after pulmonary contusion. Am J Surg 1973; 126:773-7 |
2 An |
Changes in nl lung with opposite lung injury. Shows injured lung releases systemic factors that damage normal lung. |
|
Trinkle 44 |
1973 |
Trinkle JK, Furman RW: Pulmonary Contusion: Pathogenesis and effect of various resuscitative measures. Ann Thorac Surg 1973; 16:568-73 |
2 An |
Experimental pulmonary contusion to RLL. Crystalloid and Dextran caused lesion to be larger than colloid. Lasix and PEEP caused lesion to be smaller to statistically significant degree. Decadron had no effect on contusion size. No stat. sig. Difference when RLL weight to body weight index used. |
|
Fulton 45 |
1974 |
Fulton RL, Peter ET: Compositional and histologic effects of fluid therapy following pulmonary contusion. J Trauma 1974; 14:783-90 |
2 An |
3 limb dog study with experimental PC. Contused lung doubles its weight due to blood Fluid resuscitation increases the percentage of water in the contused lung over control groups resulting in congestive atelectasis.. This is unchanged whether or not the animal has hemorrhagic shock induced and resuscitated. Well designed study with statistical significance. |
|
Richardson 46 |
1974 |
Richardson JD, Franz JL: Pulmonary contusion and hemorrhage – Crystalloid versus colloid replacement. J Surg Res 1974; 16:336 |
1 Jadad 3 AN |
Prospective randomized animal model of 34 dogs. Results: 1. Plasma protein levels are progressively diminished in animals receiving volume replacement with crystalloid. 2. Animals exhibited declining arterial po2 levels with administration of Lactated Ringers at 90cc/kg with 30cc/kg blood loss as compared to matched plasma replacement. 3. Lung water increases significantly with administration of LR at both 30cc/kg and 90cc/kg compared to plasma. 4. Pathology exhibited alveolar disruption, hemorrhage, and interstitial edema in all groups. In plasma administered animals, hemorrhage was minimal and edema described as mild to moderate. In LR infused groups, interstitial edema was increased, there was more eosin-staining edema fluid with increased rate of infusion and the amount of edema outside of the central zone of contusion was likewise greater. Statistical methods/significance:P<-.01 to 0.5 Wilcoxon Rank Sum Test Conclusions: Plasma replacement was superior to RLS replacement of volume. Rate of replacement of RLS also affected the results. Evaluation: Animal study. Delayed studies not done to see if differences resolve. |
|
Bongard 47 |
1984 |
Bongard FS, Lew FR: Crystalloid resuscitation of patients with |
3 |
A Retrospective review of 109 patients with PC: attempted to correlate PaO2/FiO2 ratio with plasma oncotic pressure in survivors |
|
pulmonary contusion. Am J Surg 1984; 148:145-9 |
|
and non-survivors: Results: 1. No correlation between PaO2/FiO2 and Plasmo oncotic pressure. 2. No p-traumatic difference in PaO2/FiO2 between survivors and non-survivors. Conclusion: Pulmonary dysfunction after contusion is unrelated to hemodilution. (Use of crystalloid does not affect outcome) P.C. is not a progressive lesion unless pneumonia supervenes. Justification: - retrospective study does no support conclusions made. |
||
|
Johnson (*2) 48 |
1986 |
Johnson JA, Cogbill TH: Determinants of Outcome after Pulmonary Contusion. J Trauma 1986; 26:695-7 |
3 |
Retrospective case series of 86 patients . Results: Mortality was significantly greater (p<0.05) in patients with ISS greater than or equal to 25, initial GCS less than or equal to 7, transfusion of > 3units of blood and pO2/FIO2 <300. Conclusions: Mortality correlated with degree of hypoxemia on admission, extrathoracic injury , particularly head trauma and overall severity of injury.. Mortality was not correlated with either the presence of shock or amount of intravenous fluid administration. Concomitant flail chest did not lead to increased mortality, but did increase the incidence of mechanical ventilation (p<0.05). The extent of contusion assessed on admission CXR was not predicative of mortality or the need for intubation. Stats: Chi-square analysis of two proportions with Yates’correction. Level of confidence was defined p<0.05. |
|
Kollmorgen (*2) 49 |
1994 |
Kollmorgen DR, Murray KA: Predictors of mortality in pulmonary contusion. Am J Surg 1994; 168:659-64 |
|
|
|
Cohn 50 |
1997 |
Cohn SM, Zieg PM: Resuscitation of pulmonary contusion: Effects of a red cell substitute. Crit Care Med 1997; 25:484-91 |
2 AN |
Design: Cohort study with 10 pigs. Results: More decrease of hemoglobin with crystalloid. SVO2 unchanged with crystalloid but decreased with Hb substitute. Had increased MPAP greater with Hb substitute than crystalloid. Compliance decreased more with Hb substitute than crystalloid. Increased lesion size with Hb substitute on CT scan. Statistical methods: Tukey's difference test for post oc comparisons p<0.05. Conclusions: Increased hemorrhage with Hb substitute vs. crystalloid. Compliance decreased more with Hb substitute vs. crystalloid. Overall, Hb substitute did not perform well compared to crystalloid. Strength:None Weaknesses: Study of Hb substitute affect on lungs, not pulmonary contusion. There were no controls who were not contused. Study only lasted 4 hours. Did not see hypoxemia in either group; why? Used static rather than dynamic compliance. |
|
Cohn 51 |
1997 |
Cohn SM, Fisher BT: Resuscitation of pulmonary contusion: Hypertonic saline is not beneficial. Shock 1997; 8:292-9 |
1 Jadad 4 AN |
Prospective randomized trial. Jadad scale 4 (1,0-doubleblind,1,1,1)18 pigs were used to evaluate the effects of pulmonary contusion and resuscitation with Normal saline (8pigs,NS, 90cc/kg) or 7.5%saline(HTS , 4cc/kg,10pigs). The pigs were also bled 30cc/kg and resuscitated at t=20 mins. Resuscitation was continued for 20 mins and then the pigs received maintenance fluids till 4 hrs. At 4 hrs the pigs were Ct scaned to obtain injury volume and then sacrificed to measure wet and dry lung weight. ANOVA used , p<0.05 null rejected. HR was same for both groups. MAPs were lower at 40 and 120 mins for HTS group. NS resus returned bp to baseline. Cardiac index was also lower for HTS upto 60 mins compared to NS.NS returned CI to baseline. Thus O2 extraction was lower in the HTS group and never returned to baseline as with NS. Compliance worsened in both groups similarly. CT lesion volumes and dry/wet lung wts remained same for both the groups. Conclusion: Small volume hypertonic resus does not decrease lung injury. Criticism: Time studied (4 hrs) might be too short. 90cc/kg too much wrt 4 cc/kg for the hypertonic saline. |
|
Ventilatory Support |
||||
|
Pulmonary Contusion (4) |
||||
|
Shin 52 |
1979 |
Shin B, McAslan C: Management of lung contusion. Am Surg 1979;45:168-75 |
3 |
Retrospective study of 132 patients immediate intubation and ventilation with PEEP for every lung contusion . Single limb study Progressive hypoxemia and pulmonary deterioration were not seen. Deaths due to brain injury or sepsis . Conclusions: early intubation and ventilation with peep minimizes development of interstitial edema and alveolar hemorrhage. Methodologically flawed: retrospective, no statistical validation, small numbers, no correction for severity of illness. Conclusion can’t be supported by the data. |
|
Richardson 53 |
1982 |
Richardson JD, Adams L: Selective management of flail chest and pulmonary contusion. Ann. Surg 1982; 196:481-6 |
3 |
Retrospective study (retrospective review of prospectively accrued data) of 427 patients with FC-PC. 95 pts. Had FC. (86% of those also had PC) 135 pts. had PC without FC. Treatment modalities varied by physician judgment., including fluid restriction. 99 intubated. 328 not. Results: Half the FC patients were intubated and 20% of the PC patients were also. The intubated patients had a higher mortality but were more severely injured. Overall mortality 6.5% with _ of that due to pulmonary complications. Conclusions :Use ventilatory support only as a last resort with specific indications. Justification: Mostly expert opinion . No statistical analysis. |
|
Moomey 54 |
1998 |
Moomey CB, Fabian TC: Cardiopulmonary function after pulmonary contusion and partial liquid ventilation. J Trauma 1998; 45:283-90 |
2 AN |
Design: Cohort study with 23 pigs. Results: Confirmed decreased PaO2/FIO2 ratio and increased PVR, increased dead space, increased shunt in injured animals. The increase of peak inspiratory pressure was greater with partial liquid ventilation(PLV) than with PEEP. Increased PEEP caused a better increase of PaO2/FIO2 ration and a better decrease of dead space than PLV. Shunt fraction was lower and compliance higher for PEEP than PLV but difference was not statistically significant. PEEP caused a decrease in Cardiac index, stroke index and oxygen delivery; there was no change with PLV. There was less hemorrhage in uninjured lung on PLV than on PEEP. The injured lung had no histologic changes between the treatment groups. Statistics: ANOVA and Fisher's t test; p=0.05 Conclusions:Neither PLV nor PEEP was 100% effective. There were advantages and disadvantages with both. Neither reversed increased airway resistance caused by contusion. PEEP was better than PLV at restoring PaO2 and decreasing dead space. PEEP was as good at PLV at correcting PaCO2, compliance and shunt fraction. PLV is better than PEEP at maintaining cardiac index, stroke index and oxygen delivery. Strengths: Good controls. Weaknesses: Ventilator strategy did not include low tidal volumes. Could this have caused injury to both groups and been attenuated in the PLV group. Was PEEP of 25 needed? Total treatment time lasted only 2 hours and there was only 30 minutes between PEEP changes. Only single dose of perflubron was given and there was no account for evaporation; not using PEEP with PLV as is usually done may have caused more evaporative losses. |
|
Riou 55 |
2001 |
Riou B, Zaier K: High-frequency jet ventilation in life-threatening bilateral pulmonary contusion. Anesthesiology 2001; 94:927-30 |
2 |
Report on 9 patients: no controls. HFJV used after conventional ventilation failed: lung protective strategies not addressed. 4/9 patients died: all from "severe head injury": no information on the effects of HFJV on the head injury. HFJV was successful "salvage" therapy for resistant hypoxia. |
|
Flail Chest - Ventilatory Support vs. Conservative Treatment (10) |
||||
|
Diethelm 56 |
1971 |
Diethelm AG, Battle W: Management of Flail Chest Injury: A Review of 75 Cases. Am Surgeon. 1971; ___:667-70 |
3 |
Retrospective cases series review: Results: 75 patients were treated by both internal and external means of stabilization. Early stabilization was achieved by endotracheal intubation and positive pressure ventilation in 56 patients usually lasting 7 to 14 days. External fixation was required in 19 patients by using towel clips, sternal wiring or sandbags. Nine of the patients died none of which were related to hypoxia or thoracic instability. No statistics identified. Conclusions: 75 patients were treated by both internal and external means of stabilization. Early stabilization was achieved by endotracheal intubation and positive pressure ventilation in 56 patients usually lasting 7 to 14 days. External fixation was required in 19 patients by using towel clips, sternal wiring or sandbags. Nine of the patients died, none of which were related to hypoxia or thoracic instability. Justify grading: observational study without stats. Historical interest. No usable conclusions today. |
|
Trinkle 57 |
1975 |
Trinkle JK, Richardson JD, Franz JL, et al: Management of Flail Chest Without Mechanical Ventilation. Ann. Thoracic Surg. 1975; 19:355-62. |
3 |
Retrospective review of 30 patients. Results: 1. The groups were comparable with respect to age, mechanism, number and types of organs injured, requirement of operations, rib fractures, and ED stability. 2. Tracheostomy was also the preferred method of intubation in group 1. 3. Avg. # of ventilator days was 22.6 in group 1 and 0.6 in group 2 (p<0.005) 4. Group 1 was hospitalized 22.6 days avg. vs. 9.3 in group 2. (p<0.005) 5. 21% mortality in Group 1 vs. 0% in group 2. (p< 0.01) 6. 23 complications in Group 1 vs. 2 in group 2. (p<0.001) Stats:Wilcoxon Rank Sum Test/ Chi Square Test p<0.01 Conclusions/Recommendations: 1. Internal stabilization is not warranted in all cases of flail chest 2. Mandatory tracheostomy and ventilation is not needed. Justify grading. Strengths/weaknesses Compared two methods being practiced in a large center by different areas of the hospital supervised by two different groups of physicians. Methods significantly different between groups. The data are rather convincing, but the small numbers of patients and the study design do not allow major confidence in most of the statements. |
|
Shackford 58 |
1976 |
Shackford SR, Smith DE, Zarins CK, et al: The Management of Flail Chest. Am. J. Surg. 1976; 132:759-62. |
2 |
Case control group of ventilated vs non-ventilated patients with flail chest. Failure of mechanical ventilation to improve survival with flail chest is due to complications of vent support. Groups well matched for severity of thoracic injury and overall. Mechanical ventilation should be used to correct abnormalities of gas exchange rather than to overcome instability of chest wall. Endpoint is normalization of PaO2, shunt and Aa gradient. Well identified groups and stat. sig. achieved but retrospective study with small numbers. |
|
Christensson 59 |
1979 |
Christensson P, Gisselsson L, Lecerof H, et al: Early and Late Results of Controlled Ventilation in Flail Chest. Chest. 1979; 75:456-60. |
2 |
Single limb prospective observational study of 35 patients with FC. All were treated with obligatory tracheostomy and IPPB for two to three weeks. The goal was to stabilize the chest wall in a favorable position for healing. Seven patients died of other injuries. Results – 1-8 year PFTs revealed minimal to no impairment of mechanics. Zenon perfusion revealed reduction in regional perfusion in 5/35 patients. Conclusion: Mandatory IPPB is useful in allowing healing and preventing long term disability in patients with FC and paradoxical respiratory movements. Justify grading: small sample of patients in single limb study. Not compared to a control group of non-vented patients. |
|
Carpintero 60 |
1980 |
Carpintero JL, Rodriguez Diez A, Elvira JR, et al: Methods of Management of Flail Chest. Intens. Care Med. 1980; 6:217-21 |
3 |
Non-randomized observational study of 30 patients: Two groups of patients were identified. All received initial therapy identically, but those who progressed to mechanical ventilation were designated Group B. Age, initial vital signs, number of ribs fractured, hemopneumothoraces, evidence of cardiovascular injury/anomaly by EKG, head injury, initial po2 and pCO2, and need for abdominal procedure were statistically the same. 1. The ventilated group had a statistically higher incidence of pneumonia and sepsis. 2. The average stay was 3.2 for the nonventilated group vs. 11.7 for the ventilated group (p<0.01) 3. There were no statistically significant parameters in patients who received surgical fixation of fractures vs. those with flail chest that did not. 4. Static compliance measurements were the only variable in which survivors were statistically different than nonsurvivors. (56 vs/ 25 p<0.01) Stats: Student T and Chi Square ; p< 0.01 Conclusions: 1. Conservative management can be successful for flail chest and has a lower morbidity and mortality. 2. Mechanical ventilation with IMV + PEEP if the patient cannot be oxygenated conservatively. 3. The static compliance is a good prognostic indicator. 4. Early surgical fixation is needed in the very unstable chest. Justify grading. Strengths/weaknesses Observational study in which patients who were not doing well and required mechanical ventilation were stratified as a separate group. Small numbers. No real criteria for stabilization. Arms of study not random. Conclusions not well supported. |
|
Shackford 61 |
1981 |
Shackford SR, Virgilio RW, Peters RM, et al Selective Use of Ventilator Therapy in Flail Chest Injury. J. Thorac. Cardiovasc. Surg. 1981; 81:194-201 |
2 |
Design of Study: Prospective evaluation of flail chest patients in a treatment protocol for limited use of mechanical ventilation. Group I patients had severe pulmonary dysfunction. Group II patients had no pulmonary dysfunction on admission but did require temporary ventilatory support for an associated injury. Group III had no pulmonary dysfunction on admission. Blunt injuries only. Type: Cohort study of 36patients. . Group I = 13, Group II = 7, Group III = 16 Results: Complication rate in Group I significantly higher than others at 40% with pneumonia occurring in 69%. Mortality rate in group I was 15%. Group II duration of ventilation <24 hours in all but one with no deaths. Group III patients 94% didn’t require ventilatory support. Decreased proportion of flail chest patients ventilated from 74% in earlier study to 38% in this study. Mortality rate also decreased from 14% to 8% from earlier to current period. Statistical Methods / Significance: Student’s t test. P<0.01. Conclusions / Recommendations of Study: Ventilatory support should be reserved for patients who manifest some degree of pulmonary dysfunction such as hypoxemia, increased intrapulmonary shunt fraction or clinical respiratory distress. Justification grading: Limited study but defined treatment protocols and relatively homogenous groups. Ventilator protocol with 15 mg/kg tidal volumes would in and of itself contribute to lung injury. |
|
Dittmann 62 |
1982 |
Dittmann M, Steenblock U, Kranzlin M, et al: Epidural Analgesia or Mechanical Ventilation for Multiple Rib Fractures. Intensive Care Med. 1982; 8:59-92 |
3 |
Prospective analysis of treatment protocol. For 283 patients. Results: 155 patients were treated with primary ventilation, 112 patients with primary epidural analgesia, and 16 patients with general anesthesia. Primarily ventilated patients were treated for an average of 13.5 days in the ICU, spent 26.2 days in the hospital with 22 dying predominantly due to pulmonary causes and 16 solely due to non-pulmonary causes. 21 of the 155 primarily ventilated patients could be extubated early with thoracic epidural analgesia. Spontaneously breathing patients receiving thoracic epidural analgesia spent an average of 6.1 days in the ICU and a total of 17 days in the hospital. Five of the patients treated primarily with epidural analgesia needed secondary ventilation. Stats: none supplied. Conclusions: The severity of gas exchange abnrmality, not mechanical defect is the indication for ventilatory support. For patients with only moderate gas exchange abnormality , spontaneous breathing with epidural analgesia is preferable. This is a descriptive study of a protocol. Since groups are not homogenous no statement can be made regarding relative effectiveness of each modality. |
|
Miller 63 |
1983 |
Miller HA, Taylor GA, Harrison AW, et al: Management of Flail Chest. Can. Med. Assoc. J. 1983; 129: 1104-1107 |
3 |
Conclusion that not all patients with flail chest need mechanical ventilation is supported. However in the group that was ventliated, only 2 (out of 57) were intubated because of pulmonary/respiratory problems. The use of diuretics, colloids, fluid restriction and steroids was not controlled. Patients grouped retrospectively; few had ISS recorded. |
|
Odelowo 64 |
1987 |
Odelowo FO: Successful Management of Flail Chest Without the Use of a Volume Ventilator. J. Med. East. Afr.1987; 64:836-844 |
3 |
Clinical series of 7 flail chest patients treated with intercostal nerve block and chest stabilization using adhesive plaster across the flail portion. Pts received O2,and nasotracheal suction along with antibiotics. One pt expired. 2 pts could not tolerate the plaster (1-increase ICP,1pregnant). Hospital course 11-38d. No statistics used. Conclusion: Developing countries should use the management scheme since it produces good results. Criticism: No evidence that this scheme is any better than any other non-vent management. Not clear that their result are better than no management at all. |
|
Velmahos 65 |
2002 |
Velmahos GC, Vassiliu P, Chan LS, et al. Influence of Flail Chest on Outcome Among Patients with Severe Thoracic Cage Trauma. Int. Surg. 2002; 87:240-44 |
2 |
Prospective comparative study of 60 patients with thoracic trauma. 22 pts had flail chest and 68 rib fractures without flail. Outcomes looked at were, mort, resp complications (pneumonia and ARDS), need for ventilation, and length of ICU and hospital stay. Student t-test, Chi-square or Fischer’s exact test was used. P<0.05 was considered significant. Flail pts were similar to the rib-fracture-only pts except for higher ISS. Flail pts needed vent support more(despite similar rates of lung contusion) (86% vs 42%),and had more resp complications (64% vs 26%overall; pneumonia 55%vs 24% ; ARDS 27% vs 9%). They also had longer hospital stays(28d vs 17 d) and ICU stays (20d vs 9 d). Conclusion: Pts with flail chest need intubation and develop pulm complications. Criticism: Pts with flail chest had higher ISS scores and the calculation of pul contusion volume can be subjective. |
|
Modes of Ventilatory Support (9) |
||||
|
Sladen 66 |
1973 |
Sladen A, Aldredge CF, Albarran R: PEEP vs. ZEEP in the Treatment of Flail Chest Injuries. Crit. Care Med. 1973; 1:187-91. |
2 |
Prospective serial controlled study of 9 patients, patient serving as own control: Results: 1. PO2 improves in nearly all patients with the addition of PEEP of 10 or 15 (t=5.15. p<0.001) 2. No change in physiologic dead space measurement with administration of peep at 0, 10, and 15. 3. Rib alignment “usually improved” with PEEP. Stats:Student’s paired T test, p<0.001 Conclusions: 1. Oxygenation improves with application of PEEP. The authors state it is the FRC that is responsible. 2. PEEP can affect cardiac output. 3. Rib fracture alignment is improved with PEEP. Justification: 1. Very small study in which patients serve as their own controls showing that oxygenation is improved with PEEP and that it is not secondary to changes in the physiologic dead space. These conclusions are supported. 2. The conclusion that rib alignment is improved is weak as there is no real description or quantitative data. All patients had a tracheostomy and were placed on the ventilator. This is not truly applicable or acceptable in current practice standards. 3. Some of the pO2 were in the 200-300 range. ? need for vent/trach in this group 4. Statement regarding cardiac output is based on experience with only one patient in this group. I think we are now aware that this is true from other authors, but this study does not support this well. |
|
Cullen 67 |
1975 |
Cullen P, Modell JH, Kirby RR, et al: Treatment of Flail Chest. Arch Surg. 1975; 110:1099-1103 |
3 |
Retrospective human study with significant confounding: groups "contaminated" with criteria from other groups; patients weaned differently, then claiming weaning on IMV was better: CMV patients NOT given same spontaneous breathing trial at the same time as IMV group. Conclusions not justified by their methods. |
|
Pinella 68 |
1982 |
Pinella JC: Acute Respiratory Failure in Severe Blunt Chest Trauma. J Trauma. 1982; 22:221-225 |
3 |
Retrospective review of prospective protocol, cohort study of 144 patients. Results: The size of flail chest segments were measured and classified as small (<100cm2), medium (101-199 cm2) and large (>200cm2) with the size of the flail chest segment determining the need for ventilatory support. Aggressive medical management did not prevent most patients (79%) with large flail segments (>200 cm2) from requiring intubation. The initial Pa02/FIO2 and the number of associated extra-thoracic injuries did not correlate significantly with mortality. Further, the presence of pulmonary contusion, number of fractured ribs and hemopneumothorax were not significant determinants of death. When comparing continuous mandatory ventilation to intermittent mandatory ventilation in the two study groups, the number of days on respirator, thoracic injuries, level of PEEP used did not significantly vary, but the course of respiratory failure was improved with IMV. Stats: Comparisons for determinants of mortality, use of ventilatory support and the degree of severity by size of the flail segment used a fourfold table of X2. Comparison of the degree of respiratory failure in the two historical periods was accomplished by the standard error of differences between the means and the probability related to multiples of standard deviation or error for a normal distribution. |
|
Hurst 69 |
1985 |
Hurst JM, DeHaven CB, Branson RD: Comparision of Conventional Mechanical Ventilation and Synchronous Independent Lung Ventilation (SILV) in the Treatment of Unilateral Lung Injury |
2 |
Prospective single limb observational study of eight patients with PC +/- FC who were “failing” conventional ventilation and were placed on SILV. ) Significant improvements were obtained in PaO2 ( 72+8.7 to 153+37; p<.005) and shunt fraction (28+3.5 to 12.6+2.5; p<.005) No significant changes occurred in cardiac output, peripheral resistance or oxygen extraction index. Seven of the eight patients survived. Though this study was prospective, selection was non-random and no control group was studied. However , some support is lent to the claim that appropriate patients with severe unilateral disease who are failing with a single ventilator may do better with independent lung ventilation. |
|
Hurst 70 |
1989 |
Hurst JM, Branson RD, Davis K, et al: Cardiopulmonary Effects of Pressure Support Ventilation. Arch Surg.1989; 124:1067-1070 |
2 |
Conclusion, that patients with flail, pulmonary contusion, should be placed on PSV,is not supported. Patients not randomized, no controls. No data collected was shown to be statistically significant. Some observations on the changes in pulmonary mechanics after instituting PSV are beneficial. |
|
Tzelepis 71 |
1989 |
Tzelepis GE, McCool FD, Hopppin FG: Chest Wall Distortion in Patients with Flail Chest. Am. Rev. Resp. Dis. 1989; 140:31-37. |
2 |
Design of Study: Cohort study of hemodynamically stable flail chest patients on mechanical ventilation able to breathe without ventilatory assistance for several minutes versus normal control volunteers. Breath to breath variability in patterns of chest wall motion over 10 breaths was assessed by measuring the angle between displacements of the rib cage in various positions. Type: Cohort study of 9 Patients. in ventilated flail chest and 4 in control Results: There was a greater degree of chest wall distortion in flail chest wall patients the greater the loading of the ventilator, thus more distortion with spontaneous breathing IMV versus CPAP through a ventilator demand valve circuit versus CPAP through a high flow gas system. Statistical Methods / Significance: Paired t test to determine significance of pressures and angles. p<0.05. Conclusions / Recommendations of Study: The distortion imposed by ventilators increases the work of breathing in flail chest patients and may contribute to difficulty breathing. Justification grading: Conclusion not supported by study evidence. Degree of distortion of chest wall interesting, but in my opinion the ability to wean ventilator or recover from flail chest injury is related to the underlying parenchymal lung injury, the inflammatory response and the presence or absence of complications and not the paradoxical motion of the overlying chest wall |
|
Rouby 72 |
1992 |
Rouby JJ, Ben Ameur M, Jawish D, et al: Continuous Positive Airway Pressure (CPAP) vs. Intermittent Mandatory Pressure Release Ventilation (IMPRV) in patients with Acute Respiratory Failure. Intensive Care Med. 1992; 18:69-75. |
2 |
Design: Prospective cohort study with 16 patients divided into two groups. All patients in respiratory failure; most with either pneumonia or pulmonary contusion. Group 2 was supposed to have abnormal spontaneous breathing either from flail chest, quadriplegia or fentanyl sedation. Each patient in both groups was put on CPAP and IMPRV for an hour each; the order was random. Results: Only parameter different between groups 1&2 was pCO2 which was lower in Group 1; authors attribute this to less efficient spontaneous breathing in group 2. IMPRV significantly increased minute ventilation in group 2 patients but provided no change in group 1 patients. Peak inspiratory pressure was higher in IMPRV in both groups. Statistics: Groups compared using Mann-Whitney U test; Ventilator parameters compared using student t test; respiratory and hemodynamic data were compared using Kruskall and Wallis H test and Mann-Whitney U test. Conclusion: IMPRV improves ventilation in patients who have poor spontaneous respiration because of either flail chest or sedation or paralysis. IMPRV caused decreased spontaneous respiration in group 1. Strengths: None. Weaknesses: Only 3 patients in Group 2 had flail chest. Group 2 was too heterogenous. Each ventilator mode was tried in the same patient for only an hour in a random order. Very poorly designed study. No conclusions can be drawn from it. |
|
Ip-Yam 73 |
1998 |
Ip-Yam PC, Allsop E, Murphy J: Combined high-frequency ventilation in the treatment of an acute lung injury Ann Acad Med, Singapore. 1998; 27:437-41. |
N/A |
An anecdotal report of the successful use of high frequency jet ventilation in the treatment of resistant hypoxia consequent to multiple thoracic injuries. |
|
Tanaka 74 |
2001 |
Tanaka H, Tajimi K, Endoh Y, et al: Pneumatic Stabilization for Flail Chest Injury: An 11-Year Study. Surg. Today. 2001; 31:1217. |
2 |
2 Cohort series, one serving as control comprised of a retrospective review of charts of 59 pts with flail chest. (historical controls) One group of pts with flail chest were treated with mechanical ventilation as the primary treatment. A later group admitted to the same institution was treated with CPAP and pulmonary therapy in an attempt to avert intubation. The first group had 39 pts and the 2nd 20. Mort was lower in the 2nd group (51vs21%)..non significant statistically. Hemorrhage and brain injury caused 15 deaths. The surviving pts were identical in both the groups..same ISS,age and gender. However, they had different rates of atelactasis and pneumonia. The rates were lower in the 2nd group..(95vs 47% for atelactasis; 70 vs 27% for pneumonia) The rate of CMV was higher in the first group and the number of pts needing endotracheal intubation was lower in the 2nd group. Fisher’s test used , CI>95% significant. Conclusion:Pulmonary morbidity and the need for ETI is reduced by the introduction of analgesia, CPAP and respiratory physical therapy. Criticism: Trial is non-randomized and non-blinded. Bias may be introduced.Difference in mortality could not be demonstrated. |
|
Schweiger 75 |
? |
Schweiger JW, Downs JB, Smith RA: CPAP Improves Lung Mechanics After Flail Chest Injury. |
N/A |
Animal study |
|
Schweiger 76 |
2003 |
Schweiger JW, Downs JB, Smith RA: Chest Wall Disruption with and without Acute Lung Injury: effects of Continuous Positive Airway Pressure Therapy on Ventilation and Perfusion Relationships. Crit Care Med. 2003; 31:2364-70. |
1 Jadad 3 AN |
Prospective randomized lab investigation of 22 pigs. Three groups ventilated on IMV: uninjured control; chest wall disruption only; chest wall disruption and lung injury. Extensive measurments on IMV prior to application CPAP: Results: significant decrease in open units with chest wall disruption and an even greater decrease with disruption + lung injury. Applicaton of CPAP decreased shunt, increased # of open alveolar units, reduced FiO2 requirements without impairment of cv function. Conclusion: CPAP is beneficial for correcting alveolar closure and VQ mismatch in both FC and FC with lung injury in animals. Justification: well done prospective randomized study with good statistics. Use of acid lung injury as a mimic to pulmonary contusion is presumptive.. Otherwise, conclusions are well supported. |
|
Schreiter 77 |
2004 |
Schreiter D, Reske A, Stichert B, et al: Alveolar recruitment in combination with sufficient positive end-expiratory pressure increases oxygenation and lung aeration in patients with severe chest trauma. Crit Care Med. 2004; 32:968-75. |
3 |
A retrospective analysis (n=17) of a protocol to use lung recruitment strategy to improve oxygenation in patients with acute lung injury or full ARDS secondary to pulmonary contusion. The temporary ( less than five minutes) stepwise application of high insipiratory pressures started with 50 cm H2O and progressed in 15 cm H2O increments (range 50-80). Authors demonstrated increased paO2/FiO2 ratio, aerated lung volume by CT scan and measured total lung volumes (p<.05) Sample size was small though results statistically significant. Effect on survival or total ventilator days could not be assessed with sample size. Such protocols seem to have possible applicability to patients with pulmonary contusion. |
|
Gunduz 78 |
2005 |
Gunduz M, Unlugenc H, Ozalevli M, et al: A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 2005; 22:325-9. |
2 |
A prospective, randomized non-blinded comparison of non-invasive (mask) CPAP to IPPV via endotracheal tube. (n=52 divided into two limbs). Noninvasive CPAP led to a lower mortality (20%, 5/25 vs 33% 7/21 p<.01) and nosocomial infection rate (4/22, 18% vs. 10/21, 48% p=.001) Mean pO2 was higher in the ET group initially ( 2 days p<.05) but then equalized. A difference in the length of ICU stay could not be demonstrated. Statistical validation well done. |
|
Surgical Repair of Flail Chest (17) |
||||
|
Moore 79 |
1975 |
Moore BP: Operative Stabilization of Non-penetrating Chest Injuries. J. Thorac. Cardiovasc. Surg. 1975; 70:619-630 |
3 |
A retrospective review of 50 cases of chest wall stabilization. Results: 11 deaths of which two were related to primary respiratory failure. Ventilation via tracheostomy was used for less than 3 days in eight patients. Conclusions: operative stabilization prevents or reduces the use of mechanical ventilation and lessens or avboids permanent chest wall deformity. Justification: Expert opinion only . No comparison to other options. |
|
Paris 80 |
1975 |
Paris F, Tarazona V, Blasco E, et al: Surgical Stabilization of Traumatic Flail Chest. Thorax. 1975; 30:521-7 |
3 |
Observational study of 233 chest injured patients with 29 cases of flail. Results: 1. Group I (internal stabilization) had a mortality of 73% due to non-chest causes. 2. Group II had late surgical stabilization due to unstable medical condition on presentation and had a 40% mortality. 3. Group III was stable and had early surgical repair and no mortality. 4. Group IV had early surgical stabilization but also had internal injuries to chest or abdomen approached operatively. Mortality 1 in 4 or possibly 2 in 4. Unclear. Stats: None Conclusions: Surgical stabilization is helpful. Justify grading: Small study. Groups clearly heteogenous. No real statistical analysis. Conclusions not adequately supported. |
|
Thomas 81 |
1978 |
Thomas AN, Blaisdell W, Lewis FR, et al: Operative Stabilization for Flail Chest after Blunt Trauma. J. Thorac. Cardiovasc. Surg. 1978; 75:793-801. |
3 |
Clinical series of 4 pts with flail chest treated with operative stabilization. Pt 1 improved and was extubated in 48 hrs. Pt 2 improved her vital capacity and MIF but then died of an MI. Pt 3 improved his VC and MIF but died of hypoxic failure. Pt 4 was extubated at nine days post op but had no preop VC or MIF done to compare to post op values. Conclusion: Internal stabilization of flail chest is advantageous Criticism: Small series without good data to support the conclusion of the authors. Cannot assume that the small improvements in pul mechanics will translate into any real benefit for the patients. |
|
Hellberg 82 |
1981 |
Hellberg K, deVivie ER, Fuchs K, et al: Stabilization of Flail Chest by Compression Osteosynthesis – Experimental and Clinical Results. Thorac. Cardiovasc. Surgeon. 1981; 29:275-81 |
3 |
Cases series, cohort study of 10 patients: Results: 2 patients with type A flail chest (anterior type with unilateral or bilateral rib fractures in the costochondral area with or without sternum fracture), 3 type B (lateral type with serial segmental fractures), 4 type B (lateral type with serial rib fractures) and one dislodged sternum fracture had 29 dynamic compressions plates implanted in the lateral or anterolateral ribs; 2 compression plates utilized for sternum fixation; and 2 rib struts for additional fixation in type A flail chest. All compression osteosynthesis plates resulted in immediate stabilization of the fractured rib and stabilization of the chest wall. 8 patients survived to be successfully weaned from the respirator 3 to 14 days (mean 5.4) after the stabilization procedure. The three deaths resulted from injuries not related to the stabilization procedure. Stats not identified. Conclusions: The use of compression osteosynthesis plates results in marked reduction of pain, immediate stabilization and decreased ventilator support time. This technique is particularly suited for lateral or anterolateral serial fractures. Patients with bilateral rib serial fractures close to the costochondral junction , plate osteosynthesis can be difficult and chest wall stabilization is better achieved with one or two rib struts. Justify grading: technical description; no comparison to alternative therapies. No conclusions can be drawn. |
|
Schmit- Neuerburg 83 |
1981 |
Schmitt-Neuerburg KP, Weiss H, Labitzke R: Indication for Thoracotomy and Chest Wall Stabilization. Injury. 1981; 14:2634 |
3 |
Two limb retrospective review of 50 patients with surgical chest wall stabilization vs none. Mortality in operative group was _ that of nonop group ( 36 vs 64%) Deaths in non-op group were due to pulmonary and septic complications from prolonged vent support. Conclusion: it is better to stabilize flail chest with rib plates than pneumoatic stablization on ventilator. Weaknesses: - observational study with no discussion of design, methods or statistics. No evidence of randomization or homogeneity between two groups. |
|
Sanchez- Lloret 84 |
1982 |
Sanchez-Lloret J, Letang E, Matsu M, et al: Indicatons and Surgical Treatment of the Traumatic Flail Chest Syndrome: An original Technique. Thorac. Cardiovasc. Surgeon. 1982; 30:294-7. |
TA |
Retrospective review, cohort series Results: 7 cases of flail chest were treated by rib fixation using extraperiostal plates. Of this group, 4 patients required “lung suture”, 2 diaphragm suture and 1 splenectomy. All patients were managed with IPPV with a mean postoperative time of mechanical ventilation 15 days (variance 0 to 30 days). No deaths were directly attributed to extraperiostal plate placement. Stats: None identified. Conclusions: Extraperiosteal rib plates allow the fixation of 2 rib fracture sites with the same plate. This rib fixation technique can be used with associated intrathoracic lesions requiring emergency thoracotomy, thoracoabdominal trauma, bilateral multiple rib fractures with moderate to severe paradoxical motion of the chest wall and“flail chest syndrome”. |
|
Menard 85 |
1983 |
Menard A, Testart J, Philippe JM, et al: Treatment of Flail Chest with Judet’s Struts. J Thorac. Cardiovasc. Surg. 1983; 86:300305 |
3 |
Prospective trial of use of Judets struts to operatively stabilize flail chest in 18 pts. There were 5 deaths in the series. 3pts were extubated in 24 hrs, 2 in 8 days,7 in the third week. Info not available for the rest of the pts. Postop complications included 2 atelactases, 2 pneumonias, 1 pleurisy, 2 wound infections, 1 septicemia, 1 wire migration,1 brochoalveolitis. 6 pts had nl cxr’s, 8 had abnormalities. Only 3 pts had PFTs and they were all restrictive. Conclusion: Judets struts are better than other modes of operative flail chest immobilization and obviate the need for ventilation. Criticism: Conclusion not supported by data. There are high rates of ventilatory support. No controls or comparison of other modalities are presented. No reason given why these particular pts were chosen for operative stabilization, other than request or preferences of MDs. |
|
Galan 86 |
1992 |
Galan G, Penalver JC, Paris F, et al: Blunt Chest Injuries in 1696 Patients. Eur. J. Cardiothorac. Surg.1992; 6:284-7. |
3 |
Design of Study: Retrospective review single trauma center of blunt trauma patients with a full range of thoracic injuries over a 20 year period. Type: Observational_X__Cohort___Prevalence___Case Control___ Number of Patients: 1696 total Human_X___ or Animal_____ Results: Overall mortality in total group 5% but 37% in patients with multiple injuries. Intercostal tube in 638 patients and thoracotomy in 105 patients. Surgical fixation for flail chest performed in 29 patients only one in past decade. Mortality of surgical fixation 24% (7/29). In fixation group 9 patients no mechanical ventilation post op, 11 paitents short course of mechanical ventilation and 2 with prolonged ventilation. Statistical Methods / Significance: Not done. Conclusions / Recommendations of Study: Surgical stabilization is the best policy. Justification grading: Conclusion not supported by study data. No conclusion from study can be drawn regarding surgical stabilization in blunt chest patients. |
|
Reber 87 |
1993 |
Reber P, Ris HB, Inderbitzi R, et al: Osteosynthesis of the Injured Chest all: Use of the AO Technique. Scand J Thoracic Surg. 1993; 27:137-42. |
TA |
Retrospective study of author’s personal experience with a particular method of rib fixation in 11 patients. Does not speak to the efficacy of surgical fixation of flail. |
|
Ahmed 88 |
1995 |
Ahmed Z, Mohyuddin Z: Management of Flail Chest Injury: Internal Fixation Versus Endotracheal Intubation and Ventilation. J Thorac. Cardiovasc. Surg. 1995; 110:1676-80. |
3 |
Conclusions (implied), are not supported: that patients with flail chest should have internal rib stabilization (Kirschner wire). Patients not randomized, no statistical analysis done. Those who had surgical stabilization had surgery for other reasons, not just stabilization. Observations ARE interesting though: stabilized patients had fewer complicatioins, weaned faster, less chest deformities, lower mortality. |
|
Gyhra 89 |
1996 |
Gyhra A, Torres P, Pino J, et al: Experimental Flail Chest: Ventilatory Function with Fixation of Flail Segment in Internal and External Position. J Trauma. 1996; 40:977-9. |
2 |
Prospective controlled animal study of nine cases: In an experimental model of flail chest , authors compared fixation in internal and external position. TV, RR and minute volume were significantly improved by fixation in external position, but were worsened by fixation in internal position. PaO2 and PaCO2 were not affected. Therefore changes in mechanics were not secondary to hypoxemia. Conclusions: rib fixation in external position is preferred. Also, this work confirms other works indicating that hypoxemia is not induced by flail per se as hypoxemia was not present and oxygen administration did not affect respiratory rate. Statistics support conclusions though study size small. |
|
Mouton 90 |
1997 |
Mouton W, Lardinois D, Furrer M, et al: Long-term Follow-up of Patients with Operative Strabilisaton of a Flail Chest. Thorac. Cardiovasc. Surgeon. 1997; 45:242-4 |
3 |
Design of Study: Case series report over 6 years with flail chest after trauma and respiratory insufficiency not responding to peridural analgesia without need for mechanical ventilation for “other” reasons. Stabilization provided by osteosynthesis of chest wall using AO-technique with 3.5 mm thick reconstruction plates Type: Observational_X_Number of Patients: 23 patients Human_X Results: 30 day survival rate 91.4% with deaths secondary to 1 arrhythmia and 1 ARDS/MODS. Mean period to extubation and transfer to the ward 3.9 and 7.8 days respectively. Chest wall appeared symmetrical in all patients during 28 month mean follow-up. No implant dislocation. 24% complained of prolonged pain and discomfort more than 3 months post op. Removal of material in 2 patients resolved chronic pain. 95% of patients returned to preoperative work capacity and 86% to preoperative sports activity. Statistical Methods / Significance: Not done Conclusions / Recommendations of Study: External chest wall fixation appears attractive in this select subgroup of patients. Justification grading: Observational study only, no control group, no firm conclusions can be drawn. |
|
Voggenreiter 91 |
1998 |
Voggenreiter G, Neudeck F, Aufmkolk M: Operative Chest Wall Stabilization in Flail Chest – Outcomes of Patients With or Without Pulmonary Contusion. J. Am. Coll. Surg. 1998; 187:130-8 |
3 |
Retrospective observational study of 42 patients. Results: 1. No significant difference in age, ISS, extent of injury between groups. 2. In patients with operative stabilization for flail chest without pulmonary contusion, the ventilator day use was shorter than for those patients with flail and no contusion without stabilization (6.5 vs. 27 p<0.02) and for flail chest with pulmonary contusion (6.5 vs. 30.8.) Statistical methods: ANOVA (p<0.02) Conclusions: 1. Flail chest and respiratory insufficiency without underlying pulmonary contusion is an indication for chest wall stabilization. 2. Underlying pulmonary contusion precludes benefit of primary stabilization. Secondary stabilization may be indicated in the weaning period. Justify grading: One group of patients dropped from analysis. Retrospective in nature, uncontrolled. Did have a hospital set of criteria. Are the conclusions supported? There may be some validity in the claims regarding stabilization for insufficiency without contusion, but this cannot be claimed with major confidence from this study. . |
|
Lardinois 92 |
2001 |
Lardinois D, Krueger T, Dusmet M, et al: Pulmonary Function Testing after Operative Stabilisation of the Chest Wall for Flail Chest. Eur. J. Cardiothorac. Surg. 2001; 20:496-501. |
2 |
Prospective, non-randomized observational study of 66 patients with operative stabilization for flail chest. . Results: 6 month PFTs revealed VC, FEV1,TLC not indicative of restriction in all but 5 patients. ( All 5 patents had returned to work.) Conclusion: the best indication for early operative chest wall stabilization is antero-lateral flail and respiratory failure without PC. Secondary stabilization should be considered for PC-FC patients who have persisting chest wall instability and vent dependence after healing of contusions. Justiifcation: Patients had good outcome but non-comparative study. |
|
Tanaka 87 |
2002 |
Tanaka H, Yukioka T, Yamaguti Y, et al: Surgical Stabilization or Internal Pneumatic Sdtabilization? A Prospective Randomized Study of Management of Severe Flail Chest Patients. J Trauma. 2002; 53:727-32. |
1 Jadad 3 |
Design: Randomized controlled study with 37 patients. One group had rib stabilization, the other managed with internal pneumatic stabilization. Results: Both groups same based on demographics, and severity of injury. Ventilator management was the same in both groups. Incidence of pneumonia at day 21 was 22% in surgical group and 90% in nonsurgical group. Length of ventilation and Length of ICU stay was much higher in the nonsurgical group. Tracheostomy was required in the nonsurgical group in almost all patients and in only a few of the surgical patients. Total medical expenses in the nonsurgical group was nearly twice that of the surgical group. Spirometry showed significantly better %FVC in the surgical group at one through 12 months. Incidence of chest tightness, thoracic pain and dyspnea was significantly higher in the nonsurgical group. More of the surgical group returned to work sooner than the nonsurgical group. Statistics:Two way analysis of variance with repeated measures was used to analyze the interactions between groups and time factors. Tukey's test was used to compare values between the groups at individual times. Student's t test and chi squared test were used to compare nonrepeated variables. p<0.05 Conclusions: Judet strut surgical stabilization may be preferably applied for severe flail chest patients in whom prolonged ventilatory assistance is expected. Strengths: Well done. Similar groups to start with. Same ventilator management with reasonable parameters for intubation and extubation. Weaknesses: Few numbers. Other: Some might think that the exclusion of patients with severe brain or spinal cord injury or perhaps some of the other exclusion criteria introduced bias. However, the authors were trying to select homogenous groups of patients with similarly severe chest trauma and to remove other factors that can affect time on ventilator, etc. |
|
Mayberry 93 |
2003 |
Mayberry JC, Terhes JT, Ellis TJ, et al: Asbsorbable Plates for Rib Fracture Repair: Preliminary Experience. J Trauma. 2003; 55:835-9. |
3 |
10 patients, non randomized, had fixation of rib fractures with absorbable plates. Only conclusion: method is safe, was demonstrated. No statistical analysis; no non-operated cohort; no objective analysis of results in terms of pain reduction, ICU days, ventilator days or chest wall stability. |
|
Balci 94 |
2004 |
Balci AE, Eren S, Cakir O, et al: Open Fixaton in Flail Chest: Review of 64 Patients. Asian Cardiovasc. Thorac. Ann. 2004; 12:11-15. |
3 |
RETROSPECTIVE chart review of 64 pts with flail chest. # groups of pts were identified by the treatments they received: 1.operative internal fixation of ribs 2. vent support with intermittent PPV or 3 vent with SIMV. Surgically treated pts did well with lower mort (11% vs 21 and 33% in group 2 and 3),less duration of vent (3d vs 6.6, 7.8d in groups 2,3). Both groups 2,3 needed pain control beyond epidural analgesia; group 1 needed only non-narcotic analgesics. ANOVA used to compare groups. Conclusion:Operative fixation of flail chest is advantageous Criticism: Nonrandomized pt allocation…treatment was based on individual [t indications, thus pts with poor prognosis might not have been referred for surgery |
|
Other Therapies (4) |
||||
|
Sinha 95 |
1973 |
Sinha K, dayal A, Charan A: Towel Clip Tarction: A Simple and Effective Method for the Treatment of Flail Chest. Indian J. Chest Diseases. 1973; 15:30711 |
3 |
Clinical series of towel clips applied to traumatic flail chest in 23 pts.15/23 pts had good results(symptom free and without any chest deformity), 6 had fair results (some pain and deformity on D/C). Main problem was secretion retention due to ineffective cough. No towel clip site infections or pneumo occurred. No statistical analysis done Conclusion: External traction by towel clips is effective and safe. Criticism: Poor study. No controls, no exact measures of ‘good’ results. |
|
Franz 96 |
1974 |
Franz JL, Richardson JD: Effect of methylprednisolone sodium succinate on experimental pulmonary contusion. J Thorac & CV Surg 1974; 5:842-4 |
I Jadad 4 An |
Methylprednisolone 30 minutes after experimental pulmonary contusion in 20 anesthetized dogs.. In steroid treated animals. Weight ratio between injured and uninjured lung significantly lower. Volume of injury was less. Results of course not correlated with clinical outcomes. |
|
Svennevig 97 |
1987 |
Svennevig JL, Pillgram-Larsen J, Fjeld NB, et al: Early Use of Corticosteroids in Severe Closed Chest Injuries: a 10-year Experience. Injury. 1987; 18:30912. |
3 |
Conclusion, that mortality in patients with severe chest injury may be reduced with use of steroids, is not supported. No randomization, no criteria used whether or not to give steroids; patients with "severe" chest injury: only 34% required mechanical ventilation. Cause of patient mortality not specified, making it impossible to decide whether or not steroids could have been a factor. |
|
Beg 98 |
1987 |
Beg MH, Reyazuddin, Ansari MM, Conservative Management of Flail Chest. J. Indian Med. Assoc. 1990; 88:186-7. |
3 |
Retrospective series of 100 patients. Results: 1. Multiple injuries are common with 45% intrathoracic and 30% extrathoracic. 2. Mortality rate is 11%, .average hospital stay is 15 days. Stats: None except demographic statistics, averages and percents. Conclusions: Pad and strapping recommended. Justify grading: Purely observational study. Some treatment options exercised (e.g. steroid, strapping) would not be considered standard of care. No conclusions were given in this paper. |